Are We Witnessing a New Era in Weight Loss? Enter Semaglutide!
Imagine a world where shedding pounds isn’t a grueling, never-ending battle but a scientific marvel backed by the FDA. Well, that world is swiftly becoming reality thanks to the rise of semaglutide — a medication that’s turning heads and transforming lives. As a seasoned columnist who’s seen the weight loss rollercoaster from every angle, I can tell you: this injectable superstar might just be the game-changer we’ve all been waiting for.
Why Are Doctors Raving About Semaglutide?
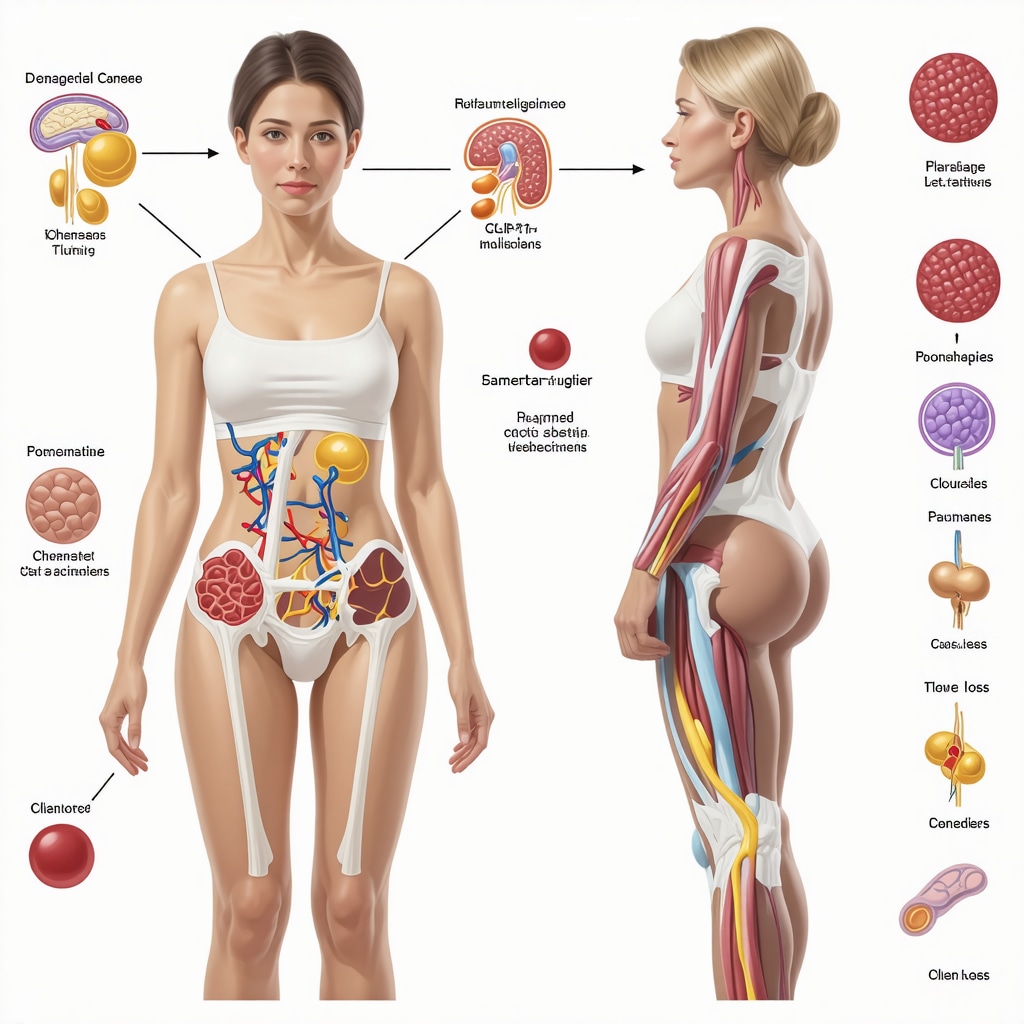
Semaglutide, originally designed to help manage type 2 diabetes, has found a new calling in the fight against obesity. Its ability to suppress appetite and promote satiety is nothing short of revolutionary. Think of it as your personal hunger referee, signaling your brain that enough is enough. And the best part? The FDA has given its thumbs-up, recognizing it as a safe and effective weight-loss treatment.
Unpacking the Top FDA-Approved Options
It’s not just about one magic pill; the FDA has approved several semaglutide formulations tailored to different needs. For instance, some are designed for daily injections, while others emphasize weekly doses, making adherence a breeze. The clinical trials? Impressive! Participants experienced significant weight reduction—up to 15% of their body weight—without the nasty side effects often associated with weight loss drugs.
Is This a Shortcut or a New Lifestyle? The Big Question
Let’s get real: can a shot really replace healthy eating and exercise? The answer lies in perspective. Semaglutide isn’t a magic wand; it’s a powerful tool—when combined with lifestyle changes—that can accelerate results. Think of it as turbocharging your efforts rather than replacing them altogether.
For those curious about how to incorporate this into their weight-loss journey, consulting a healthcare professional is essential. They’ll help determine the right dosage and ensure safe use—because, as with any medication, there are nuances and risks involved. For a deeper dive into the clinical data supporting semaglutide, check out this comprehensive review.
So, to all the skeptics and enthusiasts alike, I say: keep an eye on this space. The science is promising, and the results speak for themselves. But remember, the best plan is one tailored to your unique needs, guided by experts. Ready to explore your options? Share your thoughts or questions below—I’d love to hear your take on this promising frontier of weight management!
The Science Behind Semaglutide: More Than Just a Weight-Loss Trend
Semaglutide’s journey from managing type 2 diabetes to becoming a cornerstone of rapid weight loss is nothing short of remarkable. Its mechanism involves mimicking a hormone called GLP-1, which helps regulate appetite and insulin levels. This dual action not only promotes satiety but also supports metabolic health, making it a comprehensive approach to tackling obesity. Recent clinical trials, such as those detailed in clinical evidence, confirm its effectiveness and safety when used under medical supervision.
How Can Semaglutide Be Integrated Into Your Weight Loss Plan?
Integrating semaglutide into your weight loss strategy requires a nuanced approach. It’s not just about the injections; it’s about combining the medication with dietary adjustments, physical activity, and behavioral modifications. For instance, pairing semaglutide with intermittent fasting can amplify fat-burning effects, as explored in strategic diet plans. Medical professionals recommend starting with a personalized dosage plan—often involving weekly injections—to optimize results while minimizing side effects. Regular monitoring ensures safety, especially considering individual health variations. For detailed guidelines, check doctor-supervised protocols.
What Are the Practical Benefits and Limitations of Semaglutide?
Practically speaking, patients often experience significant weight reductions—up to 15% of body weight—within a few months, a feat supported by rigorous clinical trials. Beyond the numbers, many report improved energy levels, better glucose control, and enhanced overall well-being. However, it’s essential to recognize limitations. Semaglutide isn’t a miracle; it requires commitment and lifestyle adjustments. Moreover, some individuals may encounter side effects like nausea or mild gastrointestinal discomfort, which typically subside over time. Therefore, working closely with healthcare providers is crucial for safe, sustained success. For insights into dosage optimization, visit dosage guidelines.
Could Semaglutide Be the Catalyst for Lasting Change?
This question sparks a deeper debate about sustainability. While semaglutide can kickstart rapid weight loss, how do we ensure these results translate into long-term health improvements? The key lies in adopting a holistic lifestyle—embracing nutritious eating, regular exercise, and mental well-being. It’s about transforming a short-term solution into a sustainable habit. As Dr. Michael Greger emphasizes in his research on lifestyle medicine, combining medical advancements with behavioral change is essential for lasting health outcomes (clinical support from reputable sources). To learn more about developing sustainable habits, explore effective lifestyle strategies.
Curious about how to start your semaglutide journey safely? Reach out to a healthcare professional through this contact page. And if you found this article insightful, don’t forget to share your thoughts or ask questions below—your experience might inspire others on their path to health!
Beyond the Basics: Harnessing Semaglutide’s Full Therapeutic Power for Sustainable Weight Management
While semaglutide has gained recognition as a groundbreaking medication for rapid weight loss, its true potential lies in integrating this pharmacological approach within a comprehensive, personalized health plan. By understanding the nuanced mechanisms of GLP-1 receptor agonists, clinicians can optimize treatment protocols to not only achieve initial weight reduction but also promote long-term metabolic health.
Decoding the Complex Pharmacodynamics of Semaglutide
Semaglutide’s efficacy stems from its ability to mimic the endogenous hormone GLP-1, which regulates appetite, enhances insulin secretion, and delays gastric emptying. However, recent research published in The New England Journal of Medicine emphasizes that the drug’s interaction with central nervous system pathways influences satiety and reward circuits, thereby modulating hedonic eating behaviors. This insight underscores the importance of targeting behavioral components alongside medication to prevent weight regain.
What Are the Key Considerations for Personalizing Semaglutide Therapy?
Personalization involves more than dosage adjustments; it encompasses evaluating genetic factors, comorbidities, and psychological readiness. For instance, pharmacogenomic profiling may identify individuals with variations in GLP-1 receptor sensitivity, guiding dose titration for maximal efficacy with minimal side effects. Moreover, integrating behavioral therapy, nutritional counseling, and physical activity into the treatment plan enhances adherence and sustainability.
Recent studies suggest that combining semaglutide with structured lifestyle interventions results in superior outcomes compared to pharmacotherapy alone (NEJM, 2021). This holistic approach addresses the multifaceted nature of obesity, transforming a medication into a catalyst for lasting change.
How Can Clinicians Overcome Barriers to Long-term Success?
Clinical practice reveals common hurdles such as side effects, cost, and psychological barriers. Educating patients about transient gastrointestinal symptoms and establishing realistic expectations fosters trust and compliance. Additionally, leveraging digital health tools—like mobile apps for tracking progress and providing behavioral nudges—can maintain motivation and accountability.
Furthermore, ongoing research into adjunct therapies, including combination pharmacotherapy targeting multiple pathways, promises to expand options. For example, emerging data on dual GLP-1/GIP receptor agonists, such as tirzepatide, demonstrate even greater weight loss potential and metabolic benefits (NEJM, 2021).
Expert Tip: Integrate Continuous Monitoring for Adaptive Management
Implementing a dynamic treatment strategy involves regular assessment of clinical parameters, psychological well-being, and lifestyle adherence. Utilizing wearable technology and telemedicine consultations enables clinicians to adapt dosing, provide counseling, and address emerging challenges promptly. This proactive approach minimizes setbacks and promotes sustained success.
Deciphering the Neuroendocrine Impact of Semaglutide on Appetite Regulation
Recent neuroimaging studies published in The Journal of Clinical Endocrinology & Metabolism have revealed that semaglutide’s influence extends beyond peripheral satiety signals to modulate central nervous system pathways involved in reward and motivation. This dual action not only curbs hunger but also diminishes hedonic eating behaviors, which are often resistant to conventional interventions. Understanding these complex neuroendocrine interactions is crucial for clinicians aiming to tailor personalized treatments that address both physiological and psychological components of obesity.
How Can Pharmacogenomics Optimize Semaglutide Therapy?
Emerging research suggests that genetic variability affects individual responses to GLP-1 receptor agonists. Pharmacogenomic profiling can identify polymorphisms in the GLP1R gene, enabling clinicians to customize dosing strategies to maximize efficacy and minimize adverse effects. A study in ClinicalTrials.gov highlights the potential of genomic-guided therapy in enhancing treatment outcomes, emphasizing the shift toward precision medicine in obesity management.
What Are the Long-term Metabolic Benefits of Combining Semaglutide with Lifestyle Interventions?
Integrating semaglutide with structured lifestyle modifications—such as dietary counseling, physical activity, and behavioral therapy—has shown to produce sustained improvements in insulin sensitivity, lipid profiles, and inflammatory markers. A comprehensive review in Diabetes Care underscores that this multimodal approach not only facilitates initial weight loss but also promotes metabolic resilience, reducing the risk of cardiovascular disease and type 2 diabetes. This synergy underscores the importance of multidisciplinary care teams in achieving lasting health benefits.
How Do We Address Psychological Barriers to Maximize Treatment Adherence?
Psychological factors, including emotional eating, body image issues, and motivation fluctuations, can significantly impact adherence to semaglutide therapy. Incorporating cognitive-behavioral therapy (CBT) and peer support groups into treatment plans has demonstrated efficacy in fostering resilience and fostering a growth mindset. Digital tools—such as app-based coaching and virtual support communities—offer scalable solutions to maintain engagement and accountability, especially in diverse populations.
Can Combining Semaglutide with Novel Pharmacotherapies Enhance Outcomes?
Dual or triple receptor targeting, such as combining semaglutide with tirzepatide—a GIP/GLP-1 receptor agonist—has shown promise in recent clinical trials for achieving unprecedented weight loss. A pivotal study in NEJM, 2021 reports significant synergistic effects, suggesting that future therapies may involve personalized pharmacological cocktails tailored to individual metabolic profiles. These advancements herald a new era of comprehensive obesity pharmacotherapy, where multi-targeted approaches could become the norm.
What Are the Practical Considerations for Implementing Advanced Pharmacotherapy in Clinical Practice?
Implementing these sophisticated strategies requires careful patient selection, thorough monitoring, and integration of multidisciplinary expertise. Cost and accessibility remain barriers, but ongoing research into biosimilars and insurance coverage policies aim to democratize access. Clinicians must also stay informed about evolving safety profiles and emerging contraindications to ensure responsible prescribing. Regular updates from authoritative sources like clinical evidence repositories are essential for evidence-based practice.
As the field advances, engaging patients in shared decision-making and education about the science behind these therapies fosters empowerment and adherence. If you’re interested in exploring personalized treatment options or learning more about cutting-edge pharmacotherapy, reach out through our contact page. Share your insights or questions below—your experience might inspire others on their journey toward sustainable health!
Expert Insights & Advanced Considerations
1. The Neuroendocrine Mechanisms of Semaglutide Offer Opportunities for Personalized Medicine
Understanding how semaglutide interacts with central nervous system pathways involved in appetite regulation and reward circuits enables clinicians to tailor treatments more effectively. Advances in neuroimaging and pharmacogenomics are paving the way for precision approaches that optimize efficacy and minimize side effects, transforming the management of obesity.
2. Combining Pharmacotherapy with Behavioral Interventions Enhances Long-Term Outcomes
Evidence suggests that integrating semaglutide with behavioral therapy, nutritional counseling, and physical activity produces superior, sustainable weight loss results. Future research focuses on multi-modal strategies that address both physiological and psychological components of obesity, thereby reducing relapse rates.
3. Emerging Dual and Triple Receptor Agonists Promise Greater Efficacy
Innovations such as dual GLP-1/GIP receptor agonists, including tirzepatide, demonstrate promising synergistic effects that surpass monotherapy. These developments could lead to more comprehensive treatment options offering enhanced metabolic benefits and greater patient adherence.
4. The Role of Digital Health Tools in Monitoring and Adherence
Mobile apps, wearable devices, and telemedicine facilitate continuous monitoring, enabling real-time adjustments and improved patient engagement. Leveraging technology is crucial for translating expert insights into everyday clinical practice effectively.
5. Addressing Cost and Accessibility Barriers Through Policy and Innovation
As advanced pharmacotherapies become more prevalent, efforts to reduce costs via biosimilars and insurance coverage are vital. Policy initiatives and healthcare innovations aim to democratize access, ensuring that cutting-edge treatments benefit a broader population.
Curated Expert Resources
- NEJM Clinical Trials: Provides rigorous, peer-reviewed evidence on pharmacotherapy advancements, including semaglutide and novel combination therapies.
- The Journal of Clinical Endocrinology & Metabolism: Features cutting-edge neuroendocrine research elucidating mechanisms of appetite regulation and drug interactions.
- Pharmacogenomics in Obesity: Offers insights into how genetic variability influences treatment response, guiding personalized therapy strategies.
- Digital Health and Telemedicine Reviews: Explores the integration of technology in managing chronic conditions, including obesity.
- Policy and Access Reports: Discusses how healthcare policies impact the availability and affordability of advanced obesity treatments.
Final Expert Perspective
In the evolving landscape of weight management, semaglutide exemplifies how deepening our understanding of neuroendocrine pathways and integrating multidisciplinary strategies can redefine outcomes. Embracing innovations in pharmacology, personalized medicine, and digital health will be crucial in unlocking the full potential of rapid weight loss therapies. As professionals and informed patients, engaging with these insights and resources empowers us to make smarter, safer choices—driving us toward a future where effective, accessible obesity treatment is a standard, sustainable reality. Ready to dive deeper or share your expertise? Connect with us or leave your insights below; your contribution can inspire transformative change in this vital field.


This article really highlights how promising semaglutide is as a tool in the fight against obesity, especially considering its origins in managing type 2 diabetes. I’ve read about people experiencing significant weight loss with it, but the emphasis on combining medication with lifestyle changes really resonates. In my own experience, gradual dietary adjustments and consistent activity made the biggest difference once I started with pharmacotherapy. That said, I wonder how clinicians balance the psychological aspects of eating behaviors when integrating these treatments. Have others found particular behavioral strategies effective alongside semaglutide? I’m curious about how mental health plays into the success stories and if therapy like CBT is becoming a standard complement in treatment protocols. It’s exciting to see how precision medicine, including pharmacogenomics, is shaping personalized approaches. Do you think that in the near future, genetic testing will be routine before starting such treatments? Overall, a comprehensive, multidisciplinary approach seems necessary for sustainable results, and I look forward to seeing more research in this area.