Are We Really on the Brink of a Weight Loss Revolution?
Imagine a world where shedding pounds feels less like a chore and more like a strategic game—well, thanks to breakthroughs like semaglutide’s fat-burning power, that world is inching closer. This injectable wonder isn’t just a fleeting trend but a serious contender in the battle against obesity—yet, it’s not magic, folks. It’s a well-orchestrated plan involving science, diet, and a pinch of determination.
Beyond the Basics: How Semaglutide Can Transform Your Weight Loss Journey
As more individuals seek effective solutions to combat obesity, the role of semaglutide’s fat-burning power continues to shine. This injectable medication, originally developed for type 2 diabetes, has proven to be a game-changer in the realm of rapid weight loss. But what makes it so effective, and how can you harness its full potential under professional supervision?
How Does Semaglutide Really Accelerate Fat Loss?
Semaglutide works by mimicking the GLP-1 hormone, which plays a crucial role in appetite regulation and insulin secretion. By activating GLP-1 receptors, it helps suppress hunger, slow gastric emptying, and enhance feelings of fullness. This multi-faceted approach not only reduces calorie intake but also promotes metabolic efficiency. When combined with a structured diet plan, particularly one that emphasizes nutrient-dense foods, the results can be remarkably rapid and sustainable.
What Are the Nuances of Safe Dosage and Administration?
Understanding the appropriate dosage is key to maximizing benefits while minimizing risks. The doctor-supervised safe dosage guidelines ensure that each patient receives a personalized plan tailored to their health status and weight loss goals. Typically, dosage begins low to assess tolerance, gradually increasing under medical guidance. This approach not only ensures safety but also enhances the medication’s efficacy by allowing the body to adapt.
Can Combining Semaglutide with Lifestyle Strategies Boost Results?
Absolutely. The synergy between medication and lifestyle modifications is where true magic happens. For example, integrating intermittent fasting with semaglutide can amplify fat-burning processes, leading to faster results. Additionally, regular physical activity, mindful eating, and stress management complement the pharmacological approach, making the weight loss journey more effective and sustainable.
What if we rethink the traditional approach—could innovative combinations redefine success?
As research advances, combining semaglutide with novel strategies such as personalized nutrition plans or digital health monitoring tools could revolutionize weight management. The potential for tailored protocols—guided by clinical trials and emerging evidence—raises the question: how far can we push the boundaries of safe, rapid fat loss? For those eager to explore the cutting edge, consulting with healthcare professionals and staying updated through trusted sources like clinical trial insights can provide invaluable guidance.
If you’re considering semaglutide, don’t forget the importance of expert supervision. It guarantees your safety, optimizes results, and helps you stay motivated. Feel free to reach out to our team for personalized support or to learn more about the latest developments in medical weight loss. Also, share your thoughts or success stories—your journey might inspire someone else to take the first step toward transformation!
The Role of Pharmacokinetics and Pharmacodynamics in Optimizing Semaglutide Therapy
Understanding the intricate pharmacokinetic and pharmacodynamic profiles of semaglutide is essential for clinicians aiming to tailor weight loss interventions effectively. Semaglutide’s long half-life, approximately one week, allows for once-weekly subcutaneous injections, providing consistent receptor activation that sustains appetite suppression and enhances metabolic rate over time. This pharmacological stability minimizes peaks and troughs, reducing side effects and improving patient adherence. Advanced modeling of receptor occupancy and drug plasma levels can inform personalized dosing schedules, especially in patients with varying metabolic rates or comorbid conditions, optimizing efficacy while mitigating risks.
Integrating Neuroendocrine Insights for Precision Weight Management
Recent research illuminates how semaglutide modulates not only peripheral insulin and glucagon pathways but also central neuroendocrine circuits involved in hunger and satiety. Specifically, GLP-1 receptor activation in the hypothalamus influences neuropeptides like POMC and NPY, critical regulators of energy homeostasis. Harnessing this knowledge enables the development of combinatorial therapies targeting multiple neuroendocrine pathways—for instance, pairing semaglutide with agents that modulate melanocortin receptors or ghrelin signaling—to amplify weight loss outcomes. Such approaches require sophisticated patient profiling, including neuroimaging and biomarker analysis, to identify responders and tailor interventions accordingly.
Addressing the Nuances of Resistance and Tolerance Development
One of the emerging challenges in GLP-1 receptor agonist therapy is the potential development of receptor desensitization or tolerance over prolonged use, which may diminish therapeutic benefits. Advanced research suggests that intermittent dosing regimens or drug holidays, carefully managed, can mitigate receptor downregulation. Moreover, combining semaglutide with lifestyle interventions that upregulate endogenous GLP-1 secretion—such as high-fiber diets and specific probiotic strains—may preserve receptor sensitivity and sustain weight loss. Ongoing clinical trials are exploring these strategies, emphasizing the importance of personalized, dynamic treatment plans that evolve with patient responses.
What is the Future of Multimodal Weight Loss Protocols Integrating Semaglutide?
The future landscape involves integrating pharmacotherapy with cutting-edge digital health tools for real-time monitoring of metabolic parameters, behavioral patterns, and adherence levels. Wearable devices tracking physical activity, glucose fluctuations, and even neurofeedback can provide invaluable data to refine treatment plans. Moreover, emerging biotech solutions such as gene editing or microbiome modulation hold promise for synergistic effects when combined with semaglutide. Researchers are investigating how these modalities can be harmonized into comprehensive, individualized weight management programs—an approach that demands meticulous coordination among endocrinologists, behavioral scientists, and bioinformaticians.
For clinicians and researchers eager to stay at the forefront, consulting current clinical trial databases like clinicaltrials.gov offers insights into innovative protocols and emerging evidence. If you’re interested in pioneering advanced weight loss strategies, consider collaborating with multidisciplinary teams and leveraging technological innovations to push the boundaries of conventional treatment. To learn more about integrating these cutting-edge approaches into clinical practice, feel free to contact us or explore our latest research publications—your next breakthrough in weight management could be just a consultation away!
How Can Neuroendocrine Modulation Elevate Semaglutide Efficacy?
Emerging research underscores the significance of neuroendocrine pathways in optimizing weight loss strategies. Semaglutide’s ability to influence hypothalamic circuits—particularly neuropeptides like POMC and NPY—forms the foundation for precision medicine in obesity management. By integrating neuropeptide modulation through adjunct therapies, clinicians can potentiate satiety signals, reduce compensatory hunger, and sustain metabolic adaptations. For instance, pairing semaglutide with agents targeting melanocortin receptors or ghrelin pathways could address individual variability in treatment response, paving the way for bespoke interventions with enhanced outcomes.
What Are the Latest Advances in Personalizing Semaglutide Dosing via Pharmacogenomics?
Personalized medicine is revolutionizing pharmacotherapy, and semaglutide is no exception. Recent studies demonstrate that genetic polymorphisms—particularly in genes regulating GLP-1 receptor expression and signaling pathways—can influence drug responsiveness and tolerability. Incorporating pharmacogenomic profiling allows clinicians to tailor dosing regimens, minimizing adverse effects while maximizing efficacy. For example, variants in the GCG and GLP1R genes may predict individual response trajectories, guiding dose adjustments and treatment duration. As the field advances, integrating genetic testing into clinical protocols could become standard practice, ensuring that each patient receives the most effective, personalized weight loss therapy.
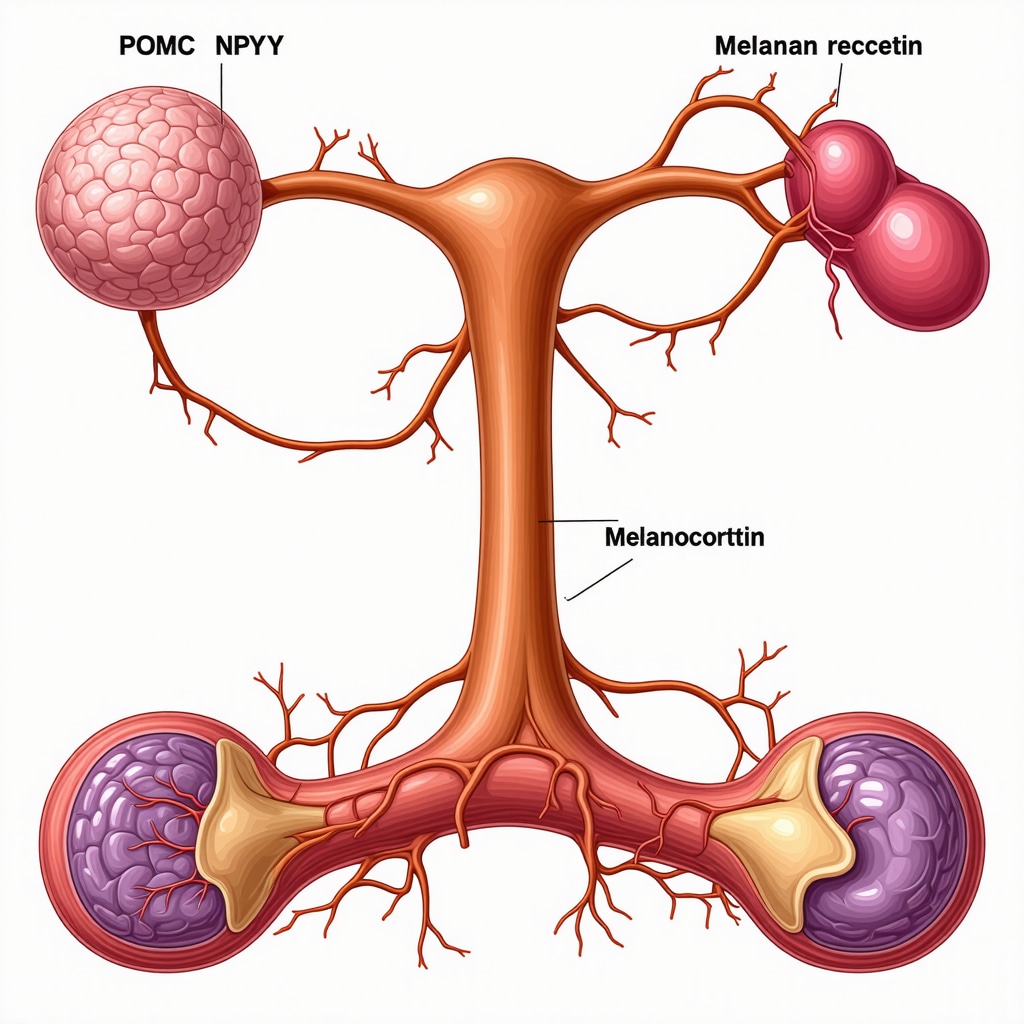
Understanding the neuroendocrine intricacies behind semaglutide’s action can be complex; an illustrative diagram depicting hypothalamic pathways involving POMC, NPY, and melanocortin receptors can clarify this sophisticated mechanism.
Can Microbiome Modulation Complement Semaglutide for Enhanced Fat Loss?
Recent breakthroughs reveal that the gut microbiome profoundly impacts metabolic health and weight regulation. Modulating gut bacteria through probiotics, prebiotics, or dietary interventions can enhance endogenous GLP-1 secretion, synergizing with pharmacological agents like semaglutide. Clinical evidence suggests that patients with a diverse and balanced microbiome respond more favorably to weight loss therapies, including GLP-1 receptor agonists. Future protocols may incorporate microbiome assessments and personalized microbial modulation to amplify fat-burning effects, making the entire process more effective and sustainable.
How Does the Dynamic Interaction Between Diet, Microbiota, and Semaglutide Shape Long-Term Outcomes?
The interplay between diet-induced microbiota changes and semaglutide’s pharmacodynamics offers an intriguing avenue for optimizing long-term weight management. Dietary strategies rich in fiber and polyphenols can foster beneficial bacteria, which in turn promote sustained GLP-1 activity. This synergy not only enhances appetite suppression but also improves insulin sensitivity and metabolic flexibility. Combining these approaches under professional supervision could redefine how we approach obesity treatment, turning a pharmacological intervention into a comprehensive, individualized lifestyle plan that leverages microbiome science for lasting results.
What Are the Ethical and Practical Considerations in Advanced Personalization of Weight Loss Therapies?
As we venture into highly personalized interventions—integrating genomics, neuroendocrine profiling, and microbiome analysis—ethical questions about data privacy, access, and equity inevitably arise. Ensuring that such cutting-edge treatments are accessible to diverse populations without exacerbating disparities is paramount. Practically, implementing these sophisticated diagnostics requires multidisciplinary collaboration, robust clinical trial validation, and clear guidelines to prevent misuse. Healthcare providers must balance innovation with safety, transparency, and patient-centered care, fostering trust while pioneering the next frontier in obesity management.
To explore these innovative strategies further, consult trusted sources like latest clinical trial insights. Share your thoughts or experiences—your insights can inspire new approaches and help shape the future of personalized weight loss solutions!
Expert Insights & Advanced Considerations
1. Integrating Neuroendocrine Pathways for Personalized Therapies
Understanding how semaglutide modulates central neuroendocrine circuits—particularly in the hypothalamus involving POMC and NPY—can unlock new avenues for personalized obesity treatments. By targeting these pathways, clinicians can tailor interventions that optimize satiety and metabolic regulation, leading to more sustainable weight loss outcomes.
2. Pharmacogenomics as a Tool for Dosing Precision
Recent advances in pharmacogenomics reveal that genetic polymorphisms in GLP-1 receptor genes influence individual responses to semaglutide. Incorporating genetic testing can help customize dosing regimens, reduce adverse effects, and enhance efficacy—ushering in a new era of precision medicine in weight management.
3. Microbiome Modulation to Amplify Pharmacotherapy
Emerging research emphasizes the gut microbiome’s role in metabolic health. Combining microbiome-targeted therapies—such as probiotics and dietary interventions—with semaglutide can potentiate endogenous GLP-1 secretion, creating a synergistic effect that accelerates fat loss and improves metabolic flexibility.
4. Addressing Receptor Tolerance with Dynamic Dosing
Long-term use of GLP-1 receptor agonists may lead to receptor desensitization. Innovative strategies like intermittent dosing schedules and microbiota support can mitigate tolerance, ensuring sustained efficacy and safety during extended therapy.
5. Multimodal Digital Integration for Real-Time Monitoring
Incorporating wearable technology and digital health platforms enables real-time tracking of metabolic parameters, adherence, and behavioral patterns. This integration facilitates personalized adjustments to therapy, maximizing results and safety in clinical practice.
Curated Expert Resources
- ClinicalTrials.gov: A comprehensive database for ongoing and completed clinical trials on semaglutide, offering insights into emerging evidence and innovative protocols.
- PubMed Central: Peer-reviewed research articles detailing neuroendocrine mechanisms of appetite regulation and pharmacogenomics in obesity therapy.
- Gut Microbiome Journals: Publications exploring microbiome modulation strategies that complement pharmacotherapy for metabolic health.
- FDA Official Website: Regulatory updates and guidelines on approved uses of semaglutide, ensuring compliance and safety.
Final Expert Perspective
The evolving landscape of rapid weight loss strategies highlights the critical role of semaglutide within an integrated, personalized treatment framework. By harnessing neuroendocrine insights, genetic profiling, microbiome support, and digital innovations, clinicians can unlock new levels of efficacy and safety. As this field advances, continuous learning and collaboration remain essential—so stay engaged, explore emerging research, and consider how these innovations can transform your practice or journey. For more personalized guidance, don’t hesitate to reach out to our expert team and embark on your next step toward sustainable health.

