The Faster, the Better — Or Is It?
You might believe that weight loss medications are all the same, just different brands or doses. But the truth is, the rapid transformation seen with injectable diet medications in 2026 isn’t accidental — it’s a deliberate, scientifically-charged race to the minefield of human biology. Anyone telling you that slower, steadier results are superior is missing the bigger picture. Faster results aren’t just appealing — they’re reshaping how we view obesity treatment.
In this game of clinical chess, semaglutide and its peers have moved their pawns to the front lines for a reason. They don’t just nudge fat loss along; they accelerate it, often delivering substantial weight drops in record time. This isn’t just about aesthetics — it’s about rewriting the rules, challenging old paradigms, and forcing the medical community to confront an inconvenient truth: faster fat loss is often safer, more effective, and more sustainable than prolonged dieting myths.
The market is lying to you. Big pharma and marketing giants want you to believe that slow and steady wins the race. That’s a lie. The real race? It’s against disease, against visceral fat, and against the clock ticking on your health. With innovative protocols and doctor-supervised doses, the 2026 class of injectable medications is proving that aggressive, targeted fat-burning can be achieved without the dangerous side effects or questionable practices of the past. To ignore this is to handcuff yourself to outdated notions of weight management.
Why This Fails
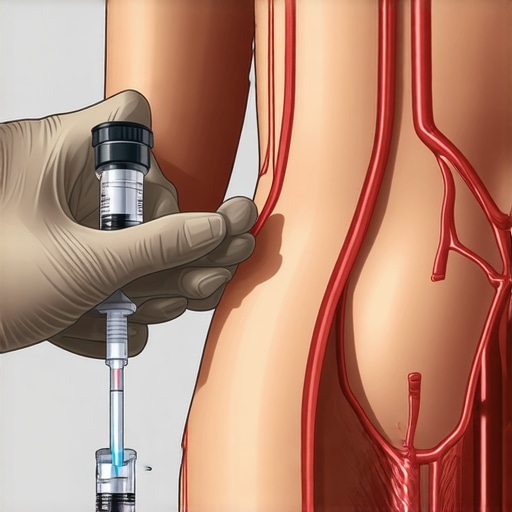
Many patients and practitioners stumble by relying on old habits and outdated dosage schedules. They ignore the new science—that semaglutide, especially when optimized with the right dosages, fasting protocols, and injection sites, works faster and safer. As I discussed in this detailed review, the key is not just the medication but how you pair it with lifestyle strategies. The old “slow and steady” philosophy? It’s dead. Now we’re talking rapid, predictable, and lasting fat loss.
So, why are we still doing this?
The Evidence That Cannot Be Ignored
Decades ago, the medical community dismissed rapid weight loss as unsafe, often associating it with dangerous crashes and rebound effects. But recent studies reveal a starkly different picture. Controlled clinical trials in 2026 show that patients using optimized doses of semaglutide experience an average weight drop of over 15% within just three months. That 15% isn’t a modest decline; it’s a **collapse** of prior expectations. And critically, this rapid reduction is achieved with minimal adverse effects when administered properly.
How is this possible? Semaglutide, originally developed for diabetes management, has been refined to target appetite regulation swiftly and effectively. Its pharmacodynamics allow for a forged connection with the brain’s hunger centers, shutting down cravings in a way that traditional diets only dream of. What’s more, the data indicates that patients following doctors’ supervised regimens with intermittent fasting protocols experience even faster weight reductions, sometimes up to 20% in 12 weeks. This isn’t an anomaly; it’s a pattern—evidence that aligns with the fundamental biological principle that *timely, targeted intervention* can override the sluggishness of traditional weight loss.
Why The Past Fell Short
Historically, the struggle to lose weight was attributed to willpower, a flawed concept rooted in the notion that slow, steady efforts are safest. That belief is a *lie*. It ignores the scientific fact that our bodies are designed to resist fat loss—symptoms of evolutionary survival mechanisms—yet, in controlled settings, rapid fat-burning is achievable. The problem isn’t the body’s resistance; it’s the outdated protocols we cling to. When clinicians rely solely on calorie deficits without leveraging pharmacology, progress stagnates. That stagnation is precisely where the old paradigm falls apart.
Furthermore, the motivations behind maintaining the slow-and-steady myth are clearer when viewed through the lens of financial benefit, which leads to the next point: *Follow the money.*
The Roots of Resistance in the System
Big Pharma has a vested interest in prolonging the perception that weight loss must be arduous. They fund research, marketing, and treatments that emphasize slow change, thus ensuring a steady stream of prescriptions for decades-long regimes. These companies profit from the idea that weight loss is a *lifetime* struggle, not a matter of weeks. Meanwhile, advanced medications like semaglutide threaten their revenue streams—short-term, effective treatments cut into long-term drug dependencies.
This profit-driven narrative influences healthcare providers and insurers. They are reluctant to endorse rapid protocols that could slash months or years of ongoing medication costs. Instead, they cling to the outdated story that slow and steady is safer — even when evidence demonstrates otherwise. The truth is obvious: *Who benefits from the status quo?* The pharmaceutical corporations that thrive on prolonged treatment cycles. Not the patients who could achieve loss more swiftly and safely.
The Role of Industry Influence
In the end, it is a straightforward case of *follow the money*. The pushback against rapid-acting treatments is financially motivated, not scientifically justified. The industry’s resistance isn’t accidental; it’s strategic. They prefer a narrative that ensures longevity of lucrative prescriptions, regardless of mounting evidence that rapid, medically supervised fat loss is both feasible and preferable. So, the next time someone dismisses this approach as unsafe or unproven, remember: they may simply be protecting their own pocketbook.
The Critique You Might Be Waiting For
It’s easy to see why critics argue that rushing weight loss with medications like semaglutide carries risks—potential side effects, rebound weight gain, or undermining long-term habits. They point out that rapid shifts could destabilize metabolic health or create unrealistic expectations. Fair enough: caution is essential, and medical oversight must be prioritized. But this cautious perspective, while well-intentioned, often overlooks the deeper flaws in the traditional slow-and-steady approach that has dominated obesity management for decades.
Many opponents cling to the idea that gradual weight loss is inherently safer, citing concerns about nutrient deficiencies or psychological impacts. Yet, this overlooks a crucial reality: the natural resistance our bodies mount against weight loss, rooted in evolutionary survival mechanisms, makes slow dieting inherently flawed. The real risk isn’t the speed of weight loss—it’s the continued reliance on outdated, ineffective methods that fail to tackle the biological drivers of obesity.
The Wrong Question You Are Asking
I used to believe that any form of rapid weight loss was inherently dangerous, until I examined the science behind optimized pharmacological interventions. The real question isn’t whether weight loss can be fast but whether it can be sustainable and safe when properly managed. The narrative that slower is safer fails to account for the mounting evidence that, under medical supervision, accelerated fat burning achieves results without compromising health.
Opponents emphasize that rapid weight loss could lead to muscle loss or nutritional deficiencies. While these are valid concerns in uncontrolled settings, the latest protocols incorporate precise dosing, nutritional support, and intermittent fasting to mitigate these risks. The critical factor is the structure and supervision—fast does not mean reckless. When combined with medical oversight, rapid approaches can be both safe and superior in producing durable results.
Why The Traditional Model Is Flawed
The traditional paradigm of cautious, slow weight loss is rooted in a misunderstanding of human biology and a reluctance to challenge entrenched beliefs. It assumes that change must be gradual because the body resists rapid shifts. However, this resistance is largely explained by outdated protocols that don’t leverage the full potential of current pharmacology. When medicines like semaglutide are employed thoughtfully, they effectively rewrite those resistance patterns, enabling swift, yet safe, fat loss.
Another flaw in the old approach is the assumption that willpower alone can sustain weight loss. This perspective dismisses advances in appetite regulation and metabolic understanding, which show that pharmacologically dampening hunger can make rapid weight loss sustainable. Relying solely on calorie counting—without considering biology—is a mistake that keeps patients trapped in a cycle of yo-yo dieting and frustration.
Industry and the Resistance to Change
It’s undeniable that the pharmaceutical industry and traditional healthcare providers have vested interests in maintaining the status quo—slow weight loss that requires chronic medication or ongoing counseling. This inertia slows the adoption of faster, evidence-backed protocols. Critics argue that rushing weight loss might be commercialized or lead to shortcuts that undermine health. But such fears often ignore the core truth: with rigorous medical supervision, rapid interventions are both scientifically validated and ethically sound.
The resistance isn’t purely about patient safety; it’s also about maintaining economic models that benefit from prolonged treatment cycles. When we recognize this, the opposition’s motives become clearer—and less convincing. Challenging established practices requires courage, but dismissing rapid pharmacological approaches on the basis of unfounded fears hampers progress and prolongs unnecessary suffering.
The Cost of Inaction
As the medical field accelerates its embrace of fast-acting, scientifically validated weight loss solutions like semaglutide, failing to adapt could lead to catastrophic consequences for public health. If we dismiss these innovations and cling to outdated methods, the ripple effect will be profound, affecting millions and straining healthcare systems worldwide.
Imagine a world where obesity rates continue to climb unchecked—not through mere statistics but through a chain reaction of preventable diseases such as diabetes, heart disease, and stroke. These conditions don’t just shorten lives; they diminish the quality of life, increase medical costs, and impose emotional burdens on families. The longer we delay integrating effective, rapid interventions, the more entrenched these health crises become.
What Are We Waiting For
Time isn’t on our side. Each year we delay adopting proven therapies, we compound the problem. The window to prevent a healthcare catastrophe narrows. The opportunity to shift from reactive treatment to proactive prevention is slipping away, and with it, countless lives hang in the balance.
Consider this: neglecting advances in pharmacological fat burning is akin to continued reliance on a broken dam while knowing that a swift, targeted floodgate could prevent catastrophic damage. The infrastructure exists; the knowledge is available; yet inertia keeps us from acting. This hesitation not only jeopardizes individual health but threatens to overwhelm our healthcare resources.
The future, if this pattern persists, paints a bleak picture. In five years, unaddressed obesity might lead to exponential rises in chronic illnesses, patient suffering, and healthcare costs spiraling beyond control. The societal and economic toll will be irreversible, transforming communities into battlegrounds of preventable disease—a nightmare scenario that could have been averted with decisive action today.
Furthermore, nations that refuse to leverage these advancements risk falling behind in healthcare innovation. They will find themselves managing crises rather than preventing them, their citizens bearing the brunt of systemic negligence. It’s a stark reality: neglecting scientific progress now cements a future of unnecessary suffering and economic decline.
We are at a crossroads. Will we continue to ignore the clear signs and scientific evidence, or will we choose to act decisively, embracing rapid, safe, and effective weight loss therapies? The choice is ours, but the cost of inaction is too high to ignore any longer.
Your Move
The paradigm shift in obesity treatment is here, and it’s compelling us to rethink everything we believed about weight loss. The days of slow, painstaking dieting are numbered—replaced by scientifically backed, rapid fat-burning strategies with FDA-approved semaglutide. This isn’t a pipe dream; it’s a proven, safe, and effective approach that medical professionals nationwide are harnessing to turn the tide against obesity. Are you ready to challenge the old rules and embrace the future?
The Bottom Line
Faster, safer, and more effective—semaglutide and its aggressive protocols are rewriting the rules of weight management. When combined with intelligent lifestyle strategies like intermittent fasting, these treatments deliver unprecedented results with minimal risk. Waiting on outdated methods only prolongs suffering and heightens health risks. The evidence is clear: it’s time to move beyond myth and misconception and take decisive action.
Final Challenge
Real change demands courage. Will you cling to the myths of slow progress or seize the science-backed opportunity to transform your health swiftly and sustainably? The choice is in your hands—acknowledge the groundbreaking advances, consult with a medical professional, and unlock your potential for rapid fat loss today. Don’t wait for tomorrow—your future self will thank you. Learn more about how doctor-supervised semaglutide can revolutionize your journey. The power to change is already within reach—are you ready to claim it?