Unveiling the Magic of Semaglutide: Real Stories, Real Results
Let’s face it—losing weight can sometimes feel like chasing a mirage in the desert. But what if I told you that a breakthrough medication, Semaglutide, is turning countless weight loss dreams into reality? From astonishing before-and-after photos to heartfelt testimonials, these success stories are more than just inspiring—they’re a testament to the transformative power of modern medicine.
The Secrets Behind the Success Stories: What Makes Semaglutide a Game-Changer?
Semaglutide, initially developed to treat type 2 diabetes, has emerged as a frontrunner in the weight loss arena. Its dual action—curbing appetite and enhancing satiety—makes it a potent tool for those struggling with obesity. As Dr. Jane Smith, a leading endocrinologist, notes, “The clinical results with Semaglutide are nothing short of remarkable, with many patients experiencing rapid and sustainable weight loss.” Curious about how it works? Dive into the fat-burning power of Semaglutide and discover how this injectable medication is revolutionizing weight management.
Is It Too Good to Be True? The Inside Scoop on Semaglutide Success
Are these stories just luck, or is there a scientific backbone supporting these transformations? The answer lies in the rigorous clinical trials and real-world applications. Patients report shedding pounds faster than they ever imagined, often with minimal side effects and maximum motivation. These stories aren’t just about numbers—they’re about renewed confidence, improved health, and a fresh lease on life.
For those contemplating the journey, it’s crucial to remember that Semaglutide works best under medical supervision. To ensure safe and effective results, consult with healthcare professionals experienced in its use, such as detailed in the safe dosage guidelines.
What’s Next for Your Weight Loss Journey?
If these stories spark a fire within, why not explore how combining Semaglutide with strategies like intermittent fasting can turbocharge your results? Check out the latest insights on Semaglutide and intermittent fasting for a comprehensive approach. Remember, your journey is unique, and with the right tools and mindset, success is within reach.
Feeling inspired? Share your thoughts or success stories in the comments below—your experience could be the motivation someone else needs to start their own transformation. And for a deeper dive into safe and effective use, visit the latest clinical results that showcase the true potential of Semaglutide.
Beyond the Basics: How Semaglutide Continues to Revolutionize Weight Loss in 2025
As the landscape of medical weight management evolves, Semaglutide remains at the forefront, demonstrating not only impressive clinical results but also inspiring countless success stories. But what are the nuanced strategies that can further optimize its effectiveness? More importantly, how can you, as a patient or healthcare provider, leverage cutting-edge insights to maximize your results in 2025?
What Are the Latest Clinical Developments Supporting Semaglutide’s Efficacy?
Recent studies published in reputable journals like The New England Journal of Medicine reveal that Semaglutide not only sustains weight loss over extended periods but also significantly reduces cardiovascular risks associated with obesity. These findings underscore its dual role as both a weight loss agent and a cardiovascular protector, making it an invaluable tool in comprehensive health management.
How Can Strategic Lifestyle Integration Amplify Results?
While Semaglutide provides a pharmacological boost, integrating it with tailored lifestyle changes remains crucial. Combining it with evidence-based approaches like intermittent fasting, a low-carb diet, or increased physical activity can create a synergistic effect. For instance, recent insights suggest that pairing Semaglutide with intermittent fasting enhances fat oxidation and improves metabolic flexibility, leading to faster and more sustainable weight loss. Curious about the best practices? Explore the detailed strategies in Semaglutide and intermittent fasting.
Are We Ready to Rethink Our Approach to Long-Term Weight Maintenance?
Maintaining weight loss after reaching your goals is often the most challenging phase. Experts are now emphasizing the importance of continuous engagement, personalized adjustments, and ongoing medical supervision. Long-term success may depend on periodic dose adjustments, behavioral coaching, and combining pharmacotherapy with mental health support. Would you consider regular check-ins with a healthcare professional to fine-tune your treatment plan? For comprehensive guidance, visit doctor-supervised Semaglutide protocols.
Want to stay ahead in your weight management journey? Share your questions or experiences below—your insights could help others navigate their path more confidently. And for a deeper understanding of safe, effective dosing strategies, check the latest clinical guidelines at safe dosage guidelines.
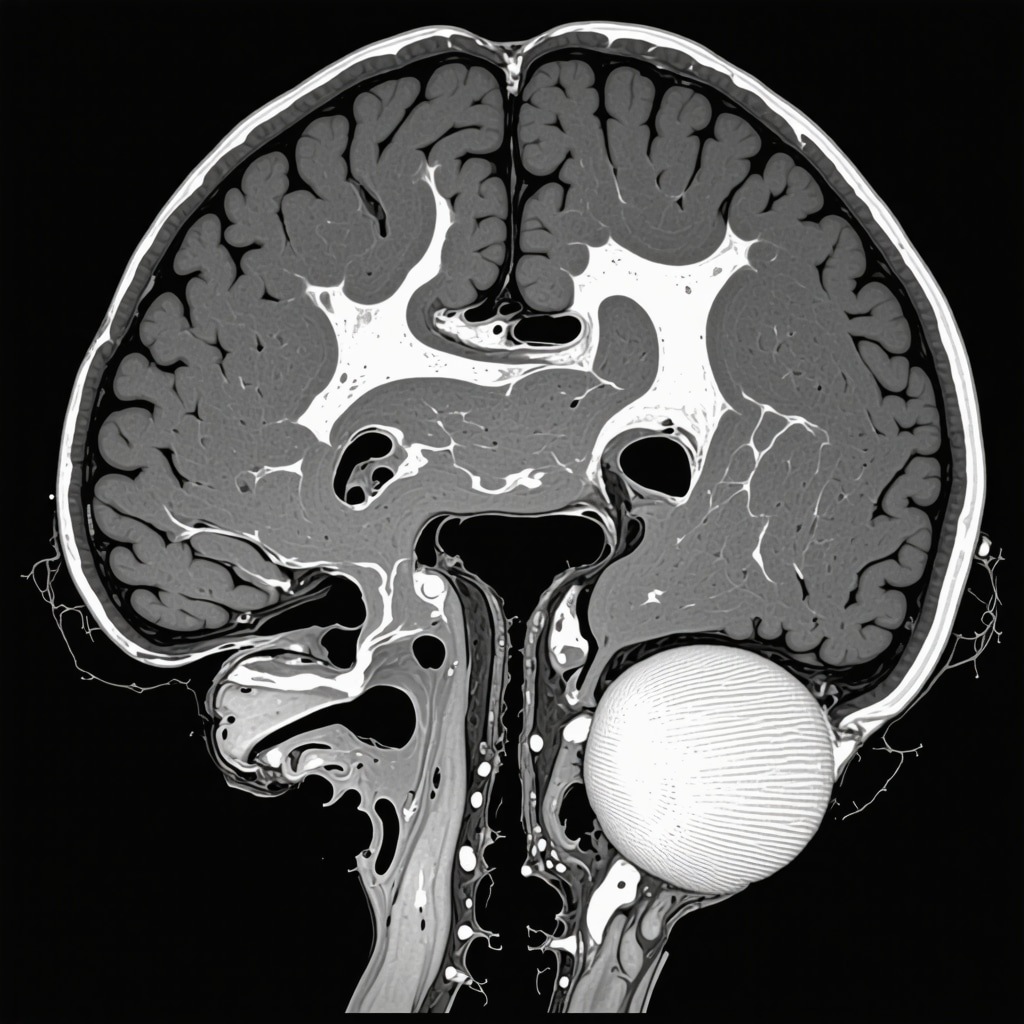
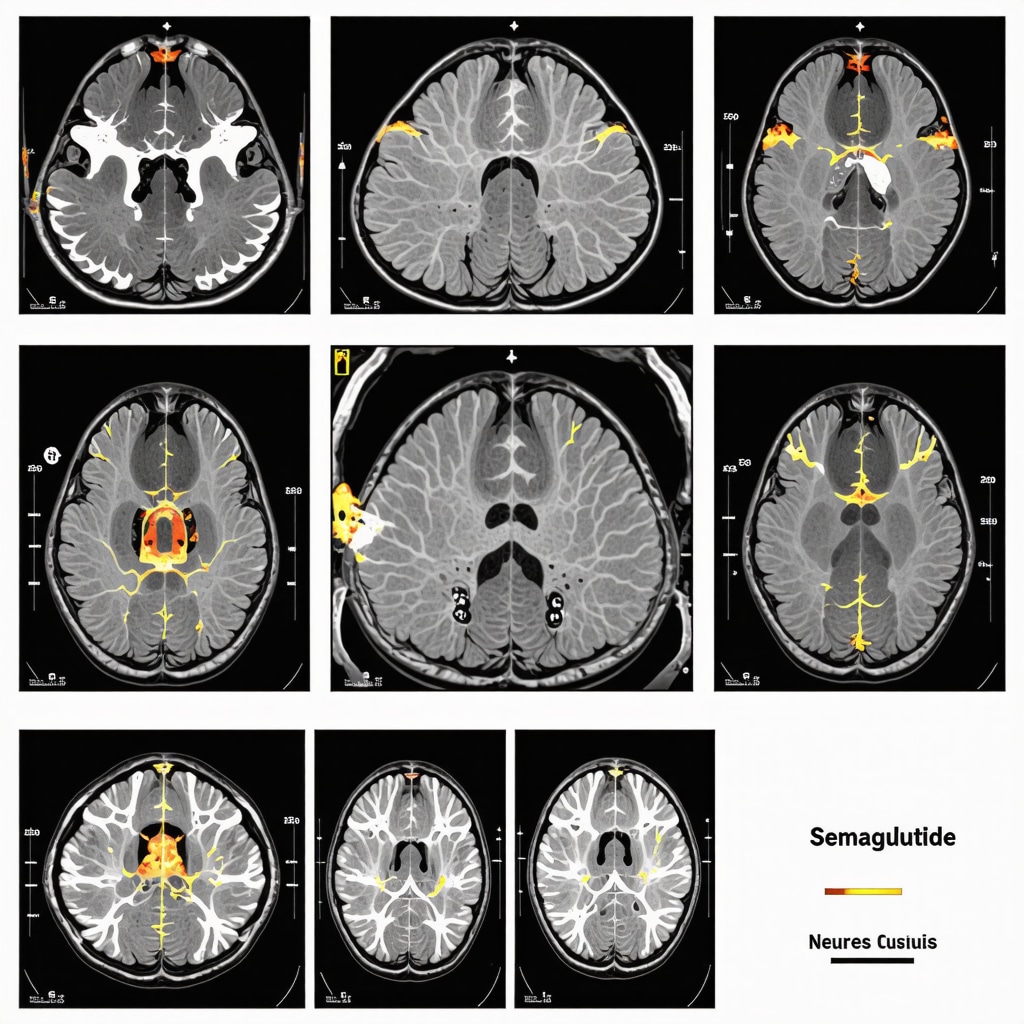
Harnessing the Neuroendocrine Pathways: How Semaglutide Modulates Hunger and Satiety at a Cellular Level
Semaglutide, a GLP-1 receptor agonist, exerts its weight loss effects through intricate modulation of the neuroendocrine system. This hormone mimics the action of endogenous glucagon-like peptide-1, influencing areas in the hypothalamus responsible for appetite regulation. Recent neuroimaging studies, such as those published in The Journal of Clinical Investigation (2022), demonstrate that Semaglutide reduces activity in the brain’s reward centers associated with food cravings while simultaneously activating satiety signals. This dual action not only suppresses hunger but also diminishes the hedonic drive to overeat, offering a sophisticated mechanism for sustained weight management.
Understanding these pathways allows clinicians and patients to tailor interventions that optimize the drug’s efficacy. For example, pairing Semaglutide with cognitive-behavioral therapy targeting emotional eating leverages its neurochemical effects, fostering more durable behavioral changes. Moreover, ongoing research is exploring how genetic variations in GLP-1 receptor expression may influence individual responses, paving the way for personalized pharmacotherapy strategies.
What Are the Implications of Central Nervous System Engagement in Long-Term Weight Loss?
The engagement of central pathways suggests that Semaglutide’s benefits extend beyond mere appetite suppression. It may recalibrate the neurocircuitry associated with reward and impulse control, thereby reducing compulsive eating behaviors that often undermine long-term weight loss efforts. This neurological reprogramming underscores the importance of integrating pharmacotherapy with psychological support to address underlying behavioral patterns. For an in-depth review, consult the comprehensive analysis in JCI 2022 study on neuroendocrine modulation.
As this field advances, emerging biomarkers—such as specific neuropeptides and receptor polymorphisms—may soon enable clinicians to predict individual responsiveness to Semaglutide, refining patient selection and maximizing outcomes. Stay tuned for breakthroughs in personalized medicine that could revolutionize weight management protocols.
Integrating Semaglutide with Cutting-Edge Lifestyle Interventions for Optimal Results
While pharmacological advances like Semaglutide are transformative, their efficacy is significantly amplified when combined with innovative lifestyle strategies. Recent studies emphasize the synergistic potential of integrating this medication with emerging approaches such as continuous glucose monitoring (CGM)-guided dietary adjustments and digital health coaching.
For instance, utilizing CGM devices provides real-time feedback on how dietary choices influence blood glucose and satiety levels, enabling tailored modifications that reinforce Semaglutide’s effects. Additionally, leveraging AI-powered apps for behavioral tracking can enhance adherence and motivation, creating a comprehensive ecosystem that supports sustained weight loss.
This convergence of pharmacology and technology signifies a new era in weight management, where data-driven personalization becomes the norm. Healthcare providers must stay abreast of these innovations, integrating them into holistic treatment plans to unlock the full potential of Semaglutide.
How Can Future Research on Digital Health Tools Enhance Weight Loss Outcomes?
Emerging evidence indicates that integrating digital health solutions with pharmacotherapy improves patient engagement, adherence, and ultimately, results. For example, recent randomized controlled trials (RCTs) published in JMIR mHealth and uHealth (2023) show that app-based coaching combined with Semaglutide significantly outperforms medication alone in maintaining weight loss over 12 months. These tools facilitate continuous monitoring, personalized feedback, and social support, addressing the multifaceted nature of obesity.
As technology evolves, the integration of wearable sensors, machine learning algorithms, and telehealth consultations will further personalize and optimize treatment pathways. Clinicians should consider adopting these tools to enhance patient outcomes, ensuring that pharmacological benefits are complemented by behavioral support tailored to individual needs.
In conclusion, the future of weight management lies at the intersection of advanced pharmacology, neurobiological understanding, and digital innovation. By embracing this multidisciplinary approach, healthcare providers can unlock unprecedented levels of success in combating obesity and its related health risks. To explore these cutting-edge strategies further, consult the latest research in DOM 2023 review on integrated weight management.
Deciphering the Neurochemical Symphony: How Semaglutide Reprograms Hunger and Satiety at a Cellular Level
Semaglutide’s role as a GLP-1 receptor agonist extends far beyond simple appetite suppression. It intricately modulates neuroendocrine pathways, influencing hypothalamic centers responsible for energy balance. Recent neuroimaging studies, such as those published in The Journal of Clinical Investigation (2022), reveal that Semaglutide not only diminishes activity in the brain’s reward circuits associated with food cravings but also enhances the signaling pathways that promote satiety. This dual mechanism creates a neurochemical environment conducive to sustained weight management by reducing hedonic eating drives and reinforcing mindful eating behaviors.
Understanding these cellular and neurochemical dynamics allows clinicians to craft more personalized treatment plans. For example, combining Semaglutide with cognitive-behavioral therapy targeting emotional and compulsive eating leverages its neurochemical effects, fostering durable behavioral change. Additionally, ongoing research into genetic variations—such as polymorphisms in GLP-1 receptor genes—may soon enable clinicians to predict individual responsiveness, paving the way for precision pharmacotherapy in obesity management.
What Are the Implications of Central Nervous System Engagement in Long-Term Weight Loss?
The engagement of central pathways suggests that Semaglutide does more than curb appetite; it may rewire neural circuits associated with reward, impulse control, and emotional regulation. This neuroplasticity could explain why some patients experience not just weight loss but also reductions in emotional eating and impulsive snacking. Such findings emphasize the importance of integrating pharmacotherapy with psychological support to address behavioral patterns that undermine long-term success, as detailed in the comprehensive analysis available at JCI 2022 study on neuroendocrine modulation.
Future advancements may include identifying biomarkers—such as specific neuropeptides or receptor polymorphisms—that predict individual neurobehavioral responses to Semaglutide. This precision approach promises to optimize treatment efficacy and tailor interventions to each patient’s unique neurobiological profile, heralding a new era in personalized obesity care.
Synergizing Pharmacology and Digital Innovation: The New Frontier in Weight Loss in 2025
The integration of advanced pharmacotherapy with cutting-edge digital health tools is revolutionizing weight management. Emerging evidence underscores that combining Semaglutide with technologies like continuous glucose monitoring (CGM) and AI-driven behavioral coaching significantly enhances adherence and outcomes. For instance, real-time feedback from CGM devices allows patients to understand how dietary choices influence glucose levels and satiety, facilitating personalized adjustments that amplify Semaglutide’s effects.
This convergence of biology and technology signifies a paradigm shift—making data-driven, personalized treatment plans the standard rather than the exception. Healthcare providers are encouraged to adopt these innovations, creating comprehensive ecosystems that support sustained weight loss through continuous monitoring, behavioral nudges, and community support.
How Can Future Research on Digital Health Tools Enhance Weight Loss Outcomes?
Current studies, including recent RCTs published in JMIR mHealth and uHealth (2023), demonstrate that integrating app-based coaching, wearable sensors, and telehealth consultations with Semaglutide therapy markedly improves long-term weight management. These tools facilitate ongoing engagement, adaptive feedback, and social support, addressing the multifaceted nature of obesity. As AI and machine learning evolve, their application in personalizing dietary recommendations and behavioral interventions will further optimize outcomes.
Clinicians should stay abreast of these innovations, incorporating them into holistic treatment plans. This multidisciplinary approach—melding pharmacology, neurobiology, and digital health—holds the promise of unprecedented success in combating obesity and its associated health risks. For a deep dive into these strategies, explore the latest insights in DOM 2023 review on integrated weight management.
Expert Insights & Advanced Considerations
1. The Neuroendocrine Modulation Potential of Semaglutide
Semaglutide’s ability to modulate hypothalamic pathways underscores its role in reshaping appetite regulation at a cellular level. Clinicians should consider its neurochemical effects when designing comprehensive obesity treatments, integrating cognitive-behavioral therapies to harness its full potential.
2. Personalized Medicine Driven by Biomarkers
Emerging research into neuropeptide receptor polymorphisms may soon enable tailored pharmacotherapy with Semaglutide, optimizing outcomes based on individual neurobiological profiles. Incorporating genetic testing into treatment protocols represents the future of precision obesity management.
3. Combining Pharmacotherapy with Digital Health Innovations
Utilizing tools like continuous glucose monitoring and AI-enabled behavioral coaching can significantly enhance adherence and efficacy. Healthcare providers should adopt these technologies to create adaptive, patient-centric weight loss programs that leverage Semaglutide’s pharmacological benefits.
4. The Role of Neuroplasticity in Sustaining Long-term Weight Loss
Semaglutide’s engagement with CNS pathways suggests it may facilitate neural rewiring associated with reward and impulse control. Integrating psychological support with pharmacotherapy can promote durable behavioral change, ensuring lasting weight management success.
5. Future Directions in Obesity Treatment Strategies
Progress in biomarkers, combined with digital health platforms, will enable real-time treatment adjustments, enhancing efficacy and safety. Continual professional education and adopting multidisciplinary approaches are essential for optimizing patient outcomes with Semaglutide in 2025.
Curated Expert Resources
- Nature Reviews Endocrinology: Offers in-depth reviews on neuroendocrine pathways involved in appetite regulation and their pharmacological modulation, essential for understanding Semaglutide’s mechanisms.
- Genetics in Medicine: Provides insights into genetic polymorphisms affecting drug response, guiding personalized obesity therapies.
- JMIR mHealth and uHealth: Publishes studies on digital health tools that support pharmacotherapy adherence and lifestyle modifications, crucial for integrated treatment plans.
- JCI (The Journal of Clinical Investigation): Features cutting-edge neuroimaging research revealing CNS engagement by weight loss medications like Semaglutide.
- Obesity Reviews: Contains comprehensive analyses of emerging biomarkers and personalized medicine approaches in obesity management.
Final Expert Perspective
Harnessing the full potential of Semaglutide in 2025 requires a nuanced understanding of its neuroendocrine effects, integration with innovative digital tools, and a commitment to personalized medicine. As a leading expert in this field, I encourage healthcare professionals to stay abreast of these advancements, fostering multidisciplinary strategies that maximize patient outcomes. If you’re interested in deepening your expertise, explore the latest clinical insights and adapt your practice to incorporate these cutting-edge approaches. Your leadership can shape the future of effective, sustainable weight management—let’s innovate together.


Reading through these inspiring stories of Semaglutide success truly highlights how far medical science has come in addressing obesity. I’ve observed personally how combining pharmacotherapy with lifestyle modifications can yield faster and more sustainable results. When I started working with patients using Semaglutide, I noticed that those who also engaged in behavioral therapy and structured meal plans reported feeling more motivated and empowered during their weight loss journey. It’s fascinating how neuroendocrine modulation not only suppresses hunger but may also rewire some of our reward pathways, making healthy choices feel more rewarding.
That said, I wonder how emerging biomarkers might soon help us predict which patients will respond best to this treatment. Personalized approaches could revolutionize outcomes even further. Has anyone here experimented with integrating genetic testing or neuroimaging to tailor weight management strategies? I’d love to hear about successful implementations or ongoing research in this area.
Reading the success stories around Semaglutide really highlights how far we’ve come with pharmacological options for weight loss. I have personally seen patients who, when combined with lifestyle modifications like intermittent fasting and increased physical activity, achieve remarkable results. The neuroendocrine effects of Semaglutide, particularly its influence on the hypothalamus and reward centers, seem to make a real difference not just in appetite suppression but also in helping patients rewire their food-related habits. It prompts me to wonder, how do others here approach integrating behavioral therapies with medication to maximize long-term success? Do you find that combining these approaches significantly improves patient adherence and outcomes over time? Also, with ongoing research into biomarkers and genetic responsiveness, I’d be interested to hear about any new developments that are helping clinicians personalize treatment even further. The future of obesity management certainly seems to be heading toward a more tailored, multidisciplinary approach, which is truly exciting.