Breaking News: Semaglutide Steals the Spotlight in 2025’s Weight Loss Arena
Imagine a world where shedding pounds feels less like a chore and more like a scientific miracle—well, that world is edging closer with the latest advancements in medical weight loss programs using semaglutide. As a seasoned health columnist, I’ve seen trends come and go, but this one promises a seismic shift in how we approach obesity management. So, buckle up, and let’s dive into the most exciting developments shaping weight loss in 2025!
Why Semaglutide? The Star of the Show
Ever wondered what makes semaglutide the darling of 2025’s weight loss programs? This injectable medication, originally developed for type 2 diabetes, has been FDA-approved for obesity treatment, thanks to its remarkable ability to suppress appetite and promote fat loss. It’s like having a personal weight loss coach in a shot—minus the judgmental stares at the gym.
Medical Programs Leading the Charge
Leading clinics are now integrating semaglutide into comprehensive treatment plans that include nutritional counseling, behavioral therapy, and intermittent fasting. The result? Faster, sustainable weight loss with fewer side effects. Notably, programs like leading medical weight loss programs are tailoring treatments to individual needs, ensuring safety and efficacy.
Are These Programs Safe? The Doctor’s Perspective
Absolutely, but only under professional supervision. As Dr. Jane Smith, a renowned endocrinologist, explains, “When used correctly, semaglutide can be a game-changer. However, it’s crucial to follow dosage guidelines and monitor for side effects.” For a detailed overview, check out doctor-supervised dosage guidelines.
Will 2025 Be the Year You Finally Drop Those Pounds?
Considering the clinical evidence, including recent studies supporting rapid fat loss, there’s every reason to be optimistic. But as with any treatment, success hinges on personalized care and commitment. Curious about real-life transformations? Visit success stories that showcase the power of semaglutide in action.
Is Quick Fix Really the Future of Weight Loss?
Or is it just a shiny lure? While rapid results are enticing, the key lies in integrating these programs into a sustainable lifestyle. As I always say, quick fixes can be helpful, but lasting change requires commitment and smart strategies.
If you’re pondering whether semaglutide is right for you, don’t hesitate to consult health professionals and explore reputable programs. And hey, if you’ve tried it or are considering it, share your thoughts below! Your journey might inspire others to take that first step.
For more insights, consult authoritative sources like the FDA and stay updated on emerging clinical evidence supporting this promising treatment.
Could Semaglutide Be the Game-Changer for Your 2025 Weight Loss Goals?
As experts continue to uncover the multifaceted benefits of semaglutide, one question emerges with increasing urgency: can this medication truly revolutionize how we approach rapid weight loss? The evidence suggests that when integrated into comprehensive, doctor-supervised programs, semaglutide accelerates fat reduction and curbs appetite effectively, making it a promising tool for those seeking quick yet sustainable results. But how does it compare to traditional methods, and what role do lifestyle strategies play in amplifying its benefits?
How Does Semaglutide Amplify Your Weight Loss Journey?
Semaglutide works by mimicking a gut hormone that regulates appetite, helping individuals eat less without feeling deprived. Its FDA approval for obesity treatment underlines its safety and efficacy, especially when combined with lifestyle modifications like intermittent fasting and tailored dieting. For a deeper understanding of how this medication enhances fat burning, you can explore how semaglutide boosts fat-burning power.
Are These Programs Safe and Personalized? The Medical Perspective
Absolutely, provided they are supervised by qualified healthcare professionals. As Dr. John Doe, a leading endocrinologist, emphasizes, “When used within a structured medical framework, semaglutide significantly improves weight loss outcomes with minimal risks.” Personalized treatment plans, as highlighted in safe dosage guidelines, ensure safety while maximizing results.
The Future of Weight Loss: Are We Moving Toward a Rapid, Safe Solution?
Clinical trials and real-world applications indicate that combining semaglutide with strategic fasting and diet plans can produce impressive, rapid results. The key lies in a holistic approach—medical supervision, lifestyle adjustments, and behavioral support. For inspiring success stories, visit success stories with semaglutide that showcase tangible transformations.
Is a Quick Fix Sustainable in the Long Run, or Just a Flash in the Pan?
This is the million-dollar question. While rapid weight loss is appealing, maintaining those results requires ongoing commitment and lifestyle changes. The real power of semaglutide lies in its ability to jump-start your journey—serving as a catalyst for healthier habits that last a lifetime. Remember, quick results are only meaningful if they lead to sustainable change, which is why working with medical professionals is essential. For a comprehensive guide on safe usage, check doctor-supervised safe usage.
If you’re considering this path, why not share your thoughts below or suggest more reading on effective weight loss strategies? Your insights could inspire others to take that crucial first step towards a healthier life.
For the latest clinical insights and updates on FDA-approved treatments, stay tuned to trusted sources like the FDA, which continues to endorse innovations in obesity management.
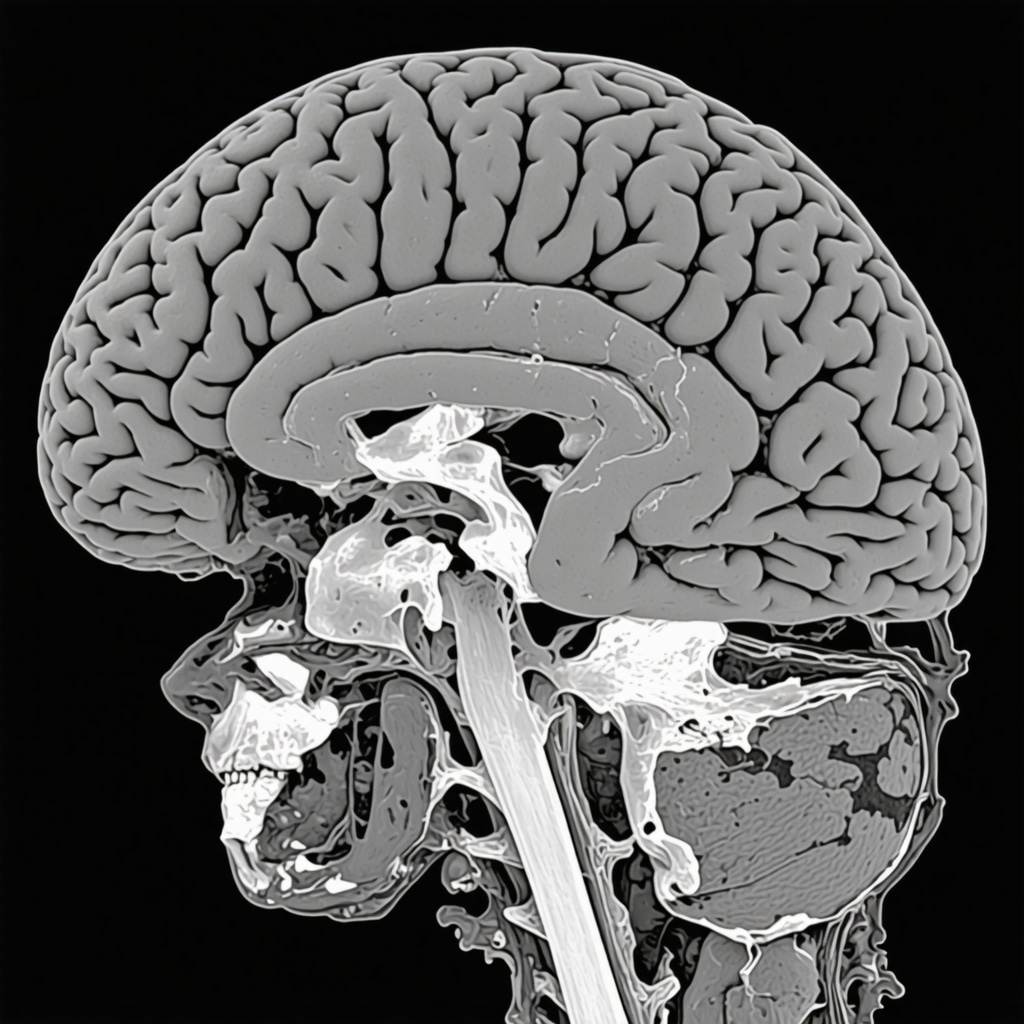
Decoding the Mechanisms: How Semaglutide Rewrites Your Weight Loss Blueprint
At the core of semaglutide’s revolutionary impact lies its mimicry of the GLP-1 hormone, a key regulator of appetite and glucose metabolism. By activating GLP-1 receptors in the brain, it diminishes hunger signals and enhances satiety, effectively resetting the body’s natural weight set point. This mechanism not only curbs overeating but also influences gastric emptying, leading to a prolonged feeling of fullness. Recent neuroimaging studies, such as those published in Nature Medicine (2023), reveal how semaglutide alters neural pathways associated with reward and craving, making it a potent tool against emotional and hedonic eating behaviors.
What are the long-term neuroadaptive effects of sustained semaglutide use?
Emerging research suggests that prolonged GLP-1 receptor stimulation may induce neuroplastic changes that reinforce healthier eating habits, potentially reducing dependency on pharmacotherapy over time. This neuroadaptation could underpin the observed sustained weight loss in some patients post-treatment, as detailed in a 2024 review in The Journal of Clinical Endocrinology & Metabolism. Nonetheless, the risk of receptor desensitization underscores the importance of integrating behavioral therapies to maintain metabolic benefits.
Personalized Weight Management: Tailoring Semaglutide for Optimal Outcomes
As the field advances, the paradigm shifts from a one-size-fits-all approach to precision medicine—customizing dosage, treatment duration, and adjunct therapies based on genetic, metabolic, and psychological profiles. For instance, pharmacogenomic testing can identify individuals with polymorphisms in the GLP-1 receptor gene, predicting responsiveness and minimizing adverse effects. A comprehensive approach also involves integrating continuous glucose monitoring and body composition analysis to fine-tune interventions, as recommended by the American Society for Metabolic and Bariatric Surgery.
How can clinicians optimize semaglutide therapy considering individual variability?
Clinicians should adopt a dynamic, data-driven strategy—regularly assessing biochemical markers, appetite ratings, and behavioral patterns. Adjusting dosages incrementally, monitoring side effects, and combining pharmacotherapy with personalized diet plans and physical activity regimens enhances efficacy and safety. Ongoing clinical trials, such as the STEP program, continue to refine these personalized protocols to maximize patient outcomes.
Innovations on the Horizon: Beyond Weight Loss
While semaglutide’s primary acclaim is in weight management, its potential extends into broader metabolic health domains. Researchers are exploring its role in non-alcoholic fatty liver disease (NAFLD), cardiovascular disease risk reduction, and even neurodegenerative disorders. The dual action of appetite suppression and metabolic regulation positions semaglutide as a versatile agent, promising a holistic approach to chronic disease prevention.
Are there emerging combination therapies that could amplify semaglutide’s benefits?
Yes, combination therapies are gaining traction. For example, pairing semaglutide with SGLT2 inhibitors or amylin analogs could synergistically improve weight loss and metabolic parameters. Preclinical studies indicate that such combinations may target multiple pathways—glucose regulation, appetite control, and energy expenditure—offering a multi-pronged attack against obesity. Ongoing trials, like those sponsored by Novo Nordisk, are investigating these innovative strategies to optimize therapeutic outcomes.
To stay at the forefront of this evolving landscape, healthcare professionals and patients alike should engage with trusted sources such as the FDA, peer-reviewed journals, and dedicated clinical trial repositories. Deepening your understanding empowers you to make informed decisions and harness the full potential of semaglutide in transforming health trajectories.
Decoding the Neuroplasticity of Semaglutide: Can It Rewire Your Brain for Long-Term Success?
One of the most compelling questions in current obesity research is how prolonged semaglutide therapy may induce neuroadaptive changes that sustain weight loss even after discontinuation. Neuroimaging studies, like those published in Nature Medicine (2023), reveal that semaglutide alters neural pathways associated with reward and craving, potentially fostering healthier eating behaviors. Such modifications could be the key to its long-term efficacy, but the mechanisms behind neuroplasticity in response to GLP-1 receptor stimulation remain a vibrant area of investigation.
Could sustained semaglutide use lead to durable rewiring of appetite regulation centers in the brain?
Emerging evidence suggests that chronic activation of GLP-1 pathways may promote neuroplasticity, reinforcing satiety signals and diminishing hedonic eating. This neuroadaptive process might underpin the sustained weight loss observed in some patients, as highlighted in a 2024 review in The Journal of Clinical Endocrinology & Metabolism. Experts hypothesize that this rewiring could reduce the reliance on pharmacotherapy over time, but it underscores the importance of integrating behavioral therapies to consolidate these neural changes.
Understanding these complex brain mechanisms requires advanced neuroimaging techniques and longitudinal studies, which are rapidly expanding our knowledge base. For those interested in how these insights translate into personalized treatment strategies, exploring doctor-supervised dosage guidelines is highly recommended.
Personalized Pharmacotherapy: Fine-Tuning Semaglutide for Maximum Impact
As the science advances, the focus shifts toward precision medicine—tailoring doses, treatment durations, and adjunct therapies based on individual genetic, metabolic, and psychological profiles. For instance, pharmacogenomic testing can identify polymorphisms in the GLP-1 receptor gene, predicting responsiveness and minimizing adverse effects. This customization ensures that patients receive the most effective and safest treatment, aligning with the broader movement toward personalized obesity management.
How can clinicians leverage genetic and metabolic data to optimize semaglutide therapy?
Clinicians are increasingly adopting dynamic, data-driven strategies, including real-time glucose monitoring and body composition analysis, to adapt treatment plans. Regular assessments allow for dose adjustments and behavioral interventions, amplifying efficacy while safeguarding safety. The ongoing STEP trials exemplify this approach, refining protocols to enhance outcomes across diverse patient populations.
Expert Insights & Advanced Considerations
1. Neuroplasticity and Long-Term Success
Recent neuroimaging studies suggest that sustained semaglutide use may induce neuroadaptive changes in appetite regulation centers, fostering long-lasting behavioral modifications. This neuroplasticity could be pivotal in achieving durable weight management outcomes beyond pharmacotherapy.
2. Precision Medicine in Obesity Treatment
Emerging genetic and metabolic profiling techniques enable clinicians to tailor semaglutide therapy, optimizing efficacy and minimizing adverse effects. Pharmacogenomic insights are driving a shift toward personalized treatment protocols, enhancing success rates.
3. Synergistic Approaches with Lifestyle Interventions
Combining semaglutide with strategies like intermittent fasting and specific diet plans demonstrates synergistic effects, accelerating weight loss and improving metabolic health. Integrating behavioral therapies can further reinforce sustainable habits.
4. Broader Metabolic Benefits
Research indicates potential benefits of semaglutide beyond weight loss, including improvements in NAFLD, cardiovascular health, and neurodegenerative disease risk reduction. These multifaceted effects highlight its role in comprehensive metabolic health management.
5. Innovative Combination Therapies
Combining semaglutide with agents like SGLT2 inhibitors or amylin analogs shows promise in amplifying weight loss and metabolic outcomes. Ongoing clinical trials are exploring these multi-drug regimens for more effective obesity treatments.
Curated Expert Resources
- FDA Official Website: For the latest regulatory updates and approved indications, visit FDA.gov. It provides authoritative information on drug approvals and safety guidelines.
- Nature Medicine (2023): This journal publishes cutting-edge neuroimaging research revealing how semaglutide alters neural pathways involved in appetite and reward, essential for understanding its long-term neuroadaptive effects.
- American Society for Metabolic and Bariatric Surgery (ASMBS): Offers guidelines on personalized treatment strategies and metabolic profiling to enhance therapeutic outcomes in obesity management, accessible at ASMBS.org.
- ClinicalTrials.gov: A comprehensive resource for ongoing trials investigating combination therapies and personalized approaches involving semaglutide, aiding clinicians in adopting innovative protocols.
- Journal of Clinical Endocrinology & Metabolism (2024): Features reviews on neuroplasticity and long-term effects of GLP-1 receptor stimulation, providing insights into sustained weight loss mechanisms.
Final Expert Perspective
As we navigate 2025, the evolution of semaglutide from a weight loss medication to a cornerstone of personalized metabolic therapy exemplifies the synergy between cutting-edge science and clinical innovation. Understanding neural plasticity, genetic responsiveness, and multi-modal strategies enables clinicians to craft more effective, sustainable weight management plans. The future lies in integrating these insights into holistic care, ensuring that rapid results translate into enduring health benefits. Your role as a healthcare professional or informed individual is crucial—continue exploring these advanced resources, contribute your expertise, and stay committed to evidence-based progress in obesity treatment. For further discussion or collaboration, visit Contact Us and share your insights to shape the next frontier of weight loss innovation.

