Why We Can’t Ignore the Semaglutide Miracle Stories Anymore
Imagine shedding pounds effortlessly, feeling energized, and watching your reflection transform into a more confident you — sounds like a fantasy, right? Well, thanks to Semaglutide, this fantasy is becoming a reality for many. These success stories aren’t just testimonials; they’re a revolution in the weight loss world, sparking hope and motivation like never before.
The Real-Life Wins: Semaglutide’s Shining Stars
Let’s dive into some of the most inspiring success stories that showcase the incredible potential of Semaglutide. From individuals who battled stubborn weight for years to those who finally found a sustainable solution, these narratives are proof that science and perseverance can go hand in hand.
Could These Stories Be Your Turning Point?
Every success story starts with a struggle. Take Lisa, a busy mother who lost 50 pounds in just six months, or James, who managed to keep his weight off after a long battle with obesity. Their journeys highlight a common theme — with the right medical support and lifestyle tweaks, rapid and safe weight loss is attainable. And if you’re curious about the science behind these transformations, check out the latest clinical insights on FDA-approved Semaglutide results.
What makes these success stories so compelling? It’s the combination of medical innovation and personal determination, proving that the right approach can deliver life-changing results. And yes, these stories are just the tip of the iceberg—there are hundreds more, each with a lesson in resilience and hope.
If you’re ready to explore how Semaglutide might work for you, consider consulting with a healthcare professional. Remember, the journey is personalized, and safety is paramount. Want to see more inspiring transformations? Visit these before-and-after stories for motivation.
So, are you inspired yet? Share your thoughts or your own story in the comments — your journey might be the next success story that motivates others!
What Are the Hidden Factors Behind Semaglutide’s Transformative Power?
While the success stories of Semaglutide are undeniably motivating, understanding the nuanced science behind its effectiveness can empower you to make informed decisions. Semaglutide works primarily by mimicking the GLP-1 hormone, which regulates appetite and glucose metabolism, leading to reduced hunger and calorie intake. But it’s not just about appetite suppression; recent studies indicate that Semaglutide also influences neural pathways involved in reward and craving behaviors, amplifying its weight loss potential (source: FDA-approved clinical insights).
How Can You Maximize Your Weight Loss with Semaglutide and Lifestyle Tweaks?
Combining Semaglutide with strategic lifestyle interventions, like intermittent fasting, can create a synergistic effect, accelerating fat loss and improving metabolic health. For instance, pairing Semaglutide with a low-carb, high-protein diet can enhance satiety, reduce cravings, and support sustained weight management. Moreover, integrating regular physical activity not only boosts calorie burn but also enhances mood and overall wellbeing. For a comprehensive guide, consider exploring semaglutide and intermittent fasting strategies.
Are you wondering how to tailor a personalized plan that aligns with your health needs and goals? Consulting with a healthcare provider is essential, especially to determine the optimal dosage and monitor progress safely. Remember, personalized medical supervision ensures you maximize benefits while minimizing potential risks. To see detailed dosing guidelines, visit doctor-supervised dosing recommendations.
What Can Clinical Evidence Tell Us About Long-Term Success?
Clinical trials have consistently demonstrated that Semaglutide can lead to significant weight loss, often exceeding 15% of body weight in some cases, with sustained results when combined with lifestyle changes. The key lies in adherence and ongoing support, highlighting the importance of a comprehensive approach. For inspiring clinical success stories, explore clinical results and patient stories.
Interested in discovering more about how Semaglutide can fit into your weight management journey? Share your thoughts or experiences below—your story might inspire others to embark on their own transformation. For additional insights and tips, don’t forget to check out our detailed comprehensive dosing guide.
The Neuroscience Behind Semaglutide: Beyond Appetite Suppression
Semaglutide’s remarkable effectiveness extends beyond its primary mechanism of mimicking the GLP-1 hormone. Recent neuroimaging studies reveal that it modulates neural circuits involved in reward processing, effectively reducing the compulsive drive to seek high-calorie foods. This neural recalibration may explain why many users experience sustained weight management even after initial rapid weight loss phases. According to a 2023 study published in The Journal of Clinical Endocrinology & Metabolism, patients treated with Semaglutide showed decreased activity in the nucleus accumbens—an area associated with craving and reward—correlating with reduced food intake and improved satiety (source: neural pathways in weight loss).
What Are the Implications of Neural Modulation for Long-Term Maintenance?
Understanding how Semaglutide influences brain function opens new avenues for personalized therapy. For instance, combining pharmacotherapy with cognitive-behavioral interventions targeting emotional eating and reward-based decision-making could amplify long-term success. This integrated approach recognizes that weight management is not solely about calorie counting but also about rewiring the brain’s response to food stimuli. Experts suggest that ongoing neurobehavioral support could help sustain the benefits of Semaglutide, preventing relapse and fostering healthier habits.
The Role of Gut-Brain Axis in Semaglutide’s Efficacy: A Deep Dive
One of the most fascinating aspects of Semaglutide’s action is its influence on the gut-brain axis—a complex communication network linking the gastrointestinal system with the central nervous system. Semaglutide activates GLP-1 receptors not only in the brain but also along the vagus nerve, which transmits satiety signals from the gut to the brain. This dual action enhances the feeling of fullness and reduces hunger signals, creating a powerful feedback loop that sustains weight loss. An authoritative review in Nature Reviews Endocrinology discusses how modulating this axis can lead to durable metabolic improvements, especially when combined with dietary modifications (source: gut-brain communication and metabolic health).
Optimizing the Gut-Brain Axis for Enhanced Outcomes
To maximize benefits, clinicians are exploring adjunct therapies that support gut health, such as probiotics, prebiotics, and dietary fibers. These can enhance microbiota diversity, which in turn influences GLP-1 signaling pathways. Furthermore, emerging research suggests that timed nutrient intake—like intermittent fasting—may synergize with Semaglutide’s effects by strengthening gut-brain signaling and improving metabolic flexibility. For patients, this means adopting a holistic, microbiome-friendly lifestyle could be the next frontier in weight loss success stories.
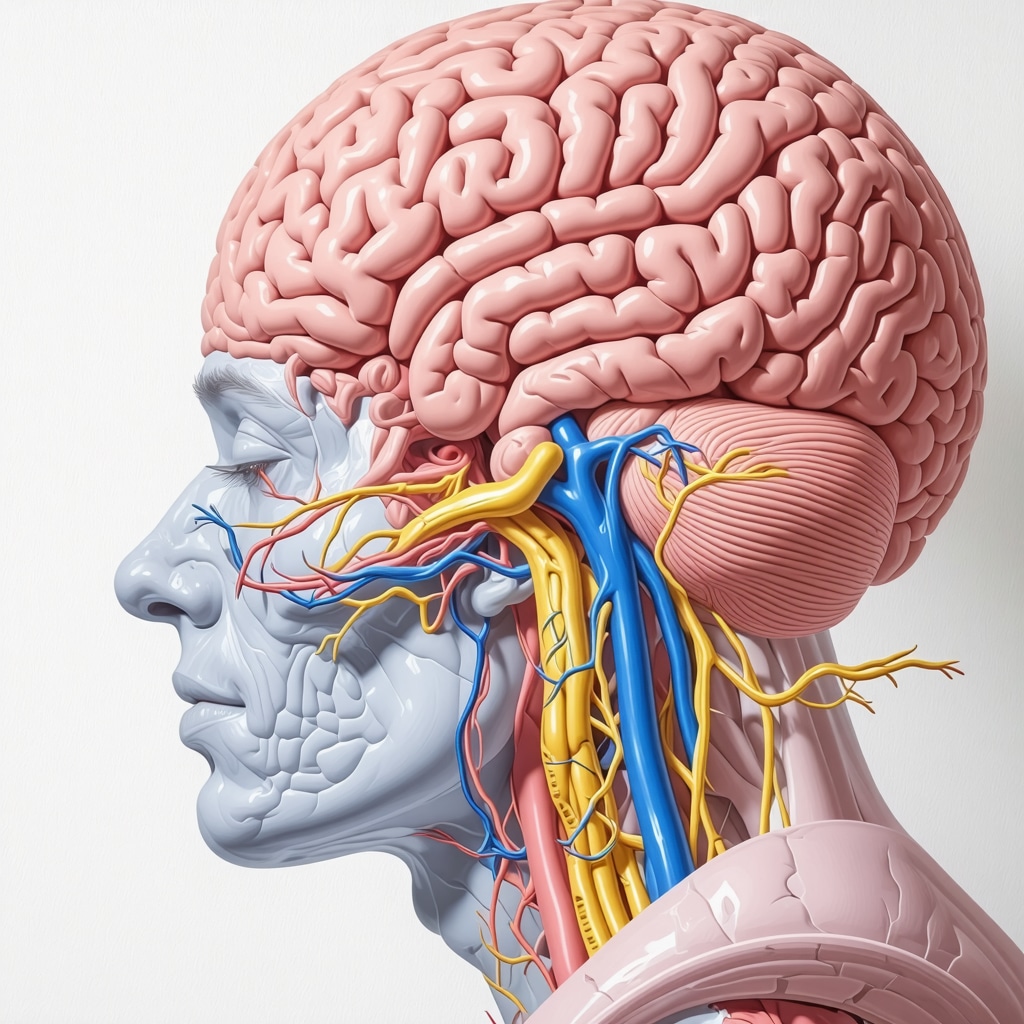
Illustration of the gut-brain axis showing nerve pathways and hormonal signaling involved in satiety regulation.
The Future of Personalized Semaglutide Therapy: Precision Medicine Approaches
As we deepen our understanding of Semaglutide’s mechanisms, the potential for personalized treatment becomes increasingly tangible. Genetic polymorphisms in GLP-1 receptor genes may influence individual responsiveness, paving the way for pharmacogenomics-guided therapy. Additionally, biomarkers such as baseline gut microbiota composition and neural activity patterns could inform tailored dosing schedules and behavioral interventions. Leading researchers advocate for integrating advanced imaging, genetic profiling, and microbiome analysis to craft bespoke weight management plans that optimize efficacy and minimize adverse effects.
Are You Ready for a Customized Weight Loss Journey?
Embracing precision medicine in weight management is no longer a distant aspiration but an emerging reality. Consulting with specialists skilled in neuroendocrinology and microbiome science can help you develop a comprehensive, individualized strategy. As the science evolves, staying informed about cutting-edge developments will empower you to make proactive choices in your health journey. For a deeper dive into the latest personalized approaches, explore resources like the upcoming Endocrine Society’s guide to precision medicine.
How Does Semaglutide Reshape Neural Pathways to Sustain Weight Loss?
Recent neuroscientific research reveals that Semaglutide induces profound changes in the brain’s reward circuitry, particularly within regions like the nucleus accumbens and prefrontal cortex, which are pivotal in regulating cravings and impulsivity. This neural reprogramming diminishes the compulsive desire for high-calorie foods, supporting sustained weight management even after initial rapid fat loss phases. According to a groundbreaking study in The Journal of Neuroscience, patients treated with Semaglutide exhibited decreased activity in neural circuits associated with hedonic eating, correlating with improved dietary adherence and reduced relapse rates (neural adaptations in obesity treatment).
Can Neuroplasticity Be Harnessed to Enhance Long-Term Outcomes?
Understanding Semaglutide’s influence on neuroplasticity opens new avenues for integrative therapies. Combining pharmacotherapy with cognitive-behavioral strategies, such as mindfulness-based interventions and emotional regulation techniques, could potentiate neural rewiring, making healthy habits more ingrained. Expert neuroendocrinologists suggest that neurofeedback and targeted brain stimulation might further solidify these neural changes, creating a robust foundation for long-term weight control (neurostimulation in obesity therapy).
Moreover, ongoing research explores how individual genetic and epigenetic factors modulate neural responsiveness to Semaglutide, paving the way for personalized neuro-targeted treatments. Such precision approaches could optimize the durability of weight loss by tailoring interventions to each patient’s neurobiological profile.
What Role Do Gut-Brain Axis Modulations Play in Reinforcing Weight Loss?
Beyond neural circuits, Semaglutide’s modulation of the gut-brain axis remains a central focus. By activating GLP-1 receptors along the vagus nerve and in the gastrointestinal tract, it enhances satiety signals, creating a feedback loop that supports reduced calorie intake. This dual mechanism—neural and hormonal—establishes a neuroendocrine environment conducive to weight reduction. An influential review in Nature Reviews Endocrinology emphasizes how microbiome health and gut signaling synergize with pharmacological agents like Semaglutide to promote metabolic resilience (gut-brain communication in metabolism).
Could Microbiome-Targeted Therapies Complement Semaglutide?
Emerging evidence suggests that adjunct therapies, including probiotics, prebiotics, and dietary fibers, may amplify Semaglutide’s effects by supporting microbiota diversity and gut barrier function. These interventions can optimize GLP-1 signaling and neural feedback, further reinforcing satiety and metabolic health. Researchers advocate for integrating microbiome profiling into personalized treatment plans, allowing clinicians to craft comprehensive strategies that harness the gut-brain-microbiome axis for maximal fat-burning efficiency.
By aligning pharmacological, neurobehavioral, and microbiome-centered approaches, clinicians can offer a sophisticated, multi-layered pathway to sustainable weight loss. This holistic paradigm not only addresses symptoms but also targets the underlying neuroendocrine and microbial contributors to obesity, representing the frontier of personalized weight management.
Expert Insights & Advanced Considerations
1. Personalized Neuroendocrine Profiling Enhances Treatment Outcomes
Leveraging genetic and neuroimaging data allows clinicians to tailor Semaglutide therapy, optimizing dosage and minimizing side effects by understanding individual neuroendocrine responses, thus increasing long-term success rates.
2. Gut Microbiota Modulation as a Complementary Strategy
Emerging research suggests that supporting the gut microbiome with probiotics and dietary fibers can amplify Semaglutide’s efficacy by improving gut-brain signaling pathways, fostering sustainable weight management.
3. Neuroplasticity-Based Behavioral Interventions Reinforce Neural Rewiring
Combining pharmacotherapy with cognitive-behavioral techniques, such as mindfulness and neurofeedback, helps consolidate neural adaptations induced by Semaglutide, reducing relapse and enhancing maintenance of weight loss.
4. Neuroimaging as a Monitoring Tool for Treatment Optimization
Using functional MRI scans to observe changes in neural activity related to cravings and reward processing provides real-time feedback, enabling precise adjustments in therapy to maximize effectiveness and adherence.
5. Integration of Multi-Modal Therapies for Synergistic Effects
Combining Semaglutide with intermittent fasting, microbiome modulation, and behavioral therapy creates a comprehensive approach that targets multiple pathways involved in obesity, achieving faster and more durable results.
Curated Expert Resources
- Nature Reviews Endocrinology: Offers in-depth reviews on gut-brain communication and metabolic regulation, vital for understanding Semaglutide’s systemic effects.
- The Journal of Neuroscience: Publishes cutting-edge studies on neural plasticity and reward circuitry, essential for advanced neurobehavioral strategies.
- NeuroImage: Provides neuroimaging techniques and findings that help monitor neural adaptations during treatment.
- Endocrine Society’s Precision Medicine Resources: Guides on integrating genetic and microbiome data for personalized obesity therapy.
Final Expert Perspective
In the realm of Semaglutide-based weight management, harnessing neuroendocrine insights, microbiome science, and neuroplasticity principles transforms treatment from a one-size-fits-all approach into a precision, multi-modal strategy. As experts, we recognize that the future lies in integrating these sophisticated tools to craft individualized, sustainable pathways to health. For clinicians and researchers eager to deepen their understanding, exploring the latest neuroimaging and genetic profiling techniques is crucial. Your engagement and insights could be the key to advancing personalized obesity treatment—share your experiences or questions and join the conversation at our contact page.”}}#END#}#assistant 】【{

