Welcome to the Future of Weight Loss: Semaglutide Steals the Spotlight
Picture this: a treatment that rewires your appetite, turns down hunger cravings, and revs up fat burning—all while fitting neatly into your weekly routine. Enter Semaglutide, the 2025 sensation that’s revolutionizing rapid weight loss. If you’ve been anywhere near the health and wellness buzz this year, you’ve probably heard whispers about this injectable wonder. But what makes it tick? And why is everyone from doctors to fitness enthusiasts raving about it?
Why Semaglutide? The Science Behind the Skinny
Semaglutide is no ordinary weight loss drug. Originally developed for diabetes management, it’s a glucagon-like peptide-1 (GLP-1) receptor agonist that reduces appetite and improves blood sugar control. In 2025, it’s FDA-approved explicitly for weight management, offering a clinically proven path to shedding pounds fast and safely. The magic lies in its ability to slow gastric emptying and enhance satiety, making overeating a thing of the past.
Is This the Weight Loss Miracle We’ve Been Waiting For?
Let’s be honest: rapid weight loss often triggers skepticism. Could Semaglutide be the silver bullet, or is it just another fad? Clinical trials published in the New England Journal of Medicine reveal patients losing an average of 15% of their body weight within a few months, with sustained results over a year. That’s not snake oil; that’s science.
Injecting Confidence: How to Use Semaglutide Responsibly
But hold your horses—before you rush to self-inject, remember that Semaglutide’s effectiveness hinges on proper dosage and medical supervision. Weekly subcutaneous injections are the norm, gradually titrated to minimize side effects. Curious about the safe dosage guidelines or injection techniques? Check out doctor-supervised Semaglutide safe dosage guidelines for an in-depth look at how to maximize your fat-burning journey without the pitfalls.
Pairing Semaglutide with Lifestyle: The Dynamic Duo for Rapid Loss
Here’s a secret: Semaglutide works best when paired with smart lifestyle choices. Intermittent fasting, for example, complements its appetite-suppressing effects beautifully. To dive deeper into this synergy, explore this strategic weight loss duo for 2025. The combination can turbocharge your fat burn and keep those pounds off for good.
Got thoughts or experiences with Semaglutide? I’d love to hear your stories or questions—drop a comment below and let’s spark a conversation about the future of weight loss!
Exploring the Nuances: Tailoring Semaglutide for Individual Success
While Semaglutide shines as a breakthrough for many, it’s crucial to recognize that weight loss is not a one-size-fits-all journey. Factors like metabolic rate, lifestyle habits, and coexisting health conditions influence how individuals respond to this injectable medication. Customizing dosage schedules and complementary dietary plans under professional guidance can significantly enhance outcomes. For example, integrating expert-curated meal plans optimized for Semaglutide users can amplify fat-burning effects and support sustainable weight management. Learn more about crafting the best Semaglutide diet plans here.
Could Combining Semaglutide with Emerging Weight Loss Technologies Create the Ultimate Fat-Burning Regimen?
As the weight loss landscape evolves, emerging technologies such as continuous glucose monitors (CGMs) and personalized metabolic tracking promise to complement pharmacological aids like Semaglutide. These tools offer real-time feedback on how your body responds to different foods and fasting windows, potentially refining the effectiveness of Semaglutide treatments. For instance, pairing Semaglutide with intermittent fasting strategies tailored by metabolic data may unlock unprecedented fat loss acceleration. The interplay of technology and medicine invites exciting possibilities for personalized, rapid weight reduction.
Monitoring Side Effects: A Critical Aspect of Semaglutide Therapy
Despite its efficacy, Semaglutide can induce side effects ranging from mild nausea and gastrointestinal discomfort to rarer instances of pancreatitis or gallbladder issues. Continuous monitoring and patient education are vital to navigate these risks safely. A detailed review published by the National Center for Biotechnology Information (NCBI) underscores the importance of dose titration and vigilant observation to mitigate adverse reactions while maximizing therapeutic benefits.
Integrating Semaglutide into Long-Term Wellness Plans
Weight loss success with Semaglutide is greatly enhanced when embedded within comprehensive wellness programs that emphasize behavior modification, nutritional education, and physical activity. Such holistic approaches help prevent weight regain and foster healthier lifestyle choices. Medical weight loss programs that combine Semaglutide with lifestyle coaching have demonstrated superior long-term effectiveness and patient satisfaction. Explore effective programs that harness Semaglutide’s full potential by visiting this resource.
If you’ve experienced Semaglutide treatment or have questions about optimizing your regimen, share your thoughts in the comments below or connect with experts via our contact page. Your insights could help others navigate their weight loss journeys more effectively.
Leveraging Metabolic Flexibility: The Next Frontier in Semaglutide Optimization
Beyond its appetite-suppressing prowess, Semaglutide’s real power emerges when integrated with metabolic flexibility strategies—a concept gaining traction among cutting-edge weight loss researchers. Metabolic flexibility refers to the body’s ability to efficiently switch between burning carbohydrates and fats for energy depending on availability. Enhancing this adaptability can drastically improve fat oxidation rates, maximizing Semaglutide’s fat-burning impact.
Recent studies suggest that individuals who cultivate metabolic flexibility through targeted nutritional timing, such as strategic carbohydrate cycling combined with Semaglutide therapy, experience accelerated reductions in adipose tissue. This synergy arises because Semaglutide slows gastric emptying and curbs hunger, while carb cycling trains muscles and mitochondria to preferentially utilize fat during fasting or low-carb phases. The result? A metabolic environment primed for sustained, rapid fat loss that transcends traditional calorie deficits.
How Can Patients Tailor Metabolic Flexibility Protocols While Using Semaglutide?
Individualized protocols should begin with comprehensive metabolic assessments, including indirect calorimetry and continuous glucose monitoring, to determine baseline substrate utilization patterns. Armed with this data, clinicians can design carb cycling schedules that align with patients’ unique energy demands and Semaglutide dosing regimens. For example, higher carbohydrate days may coincide with intense training sessions, while low-carb days support fasting periods enhanced by Semaglutide’s appetite regulation.
Additionally, integrating resistance training and high-intensity interval training (HIIT) can further augment mitochondrial efficiency and insulin sensitivity—two pillars of metabolic flexibility. Such multimodal approaches underscore that Semaglutide is not a standalone magic bullet but a catalyst for deeper metabolic reprogramming when combined with personalized lifestyle interventions.
Exploring the Molecular Mechanisms: Semaglutide’s Influence on Adipocyte Function and Energy Homeostasis
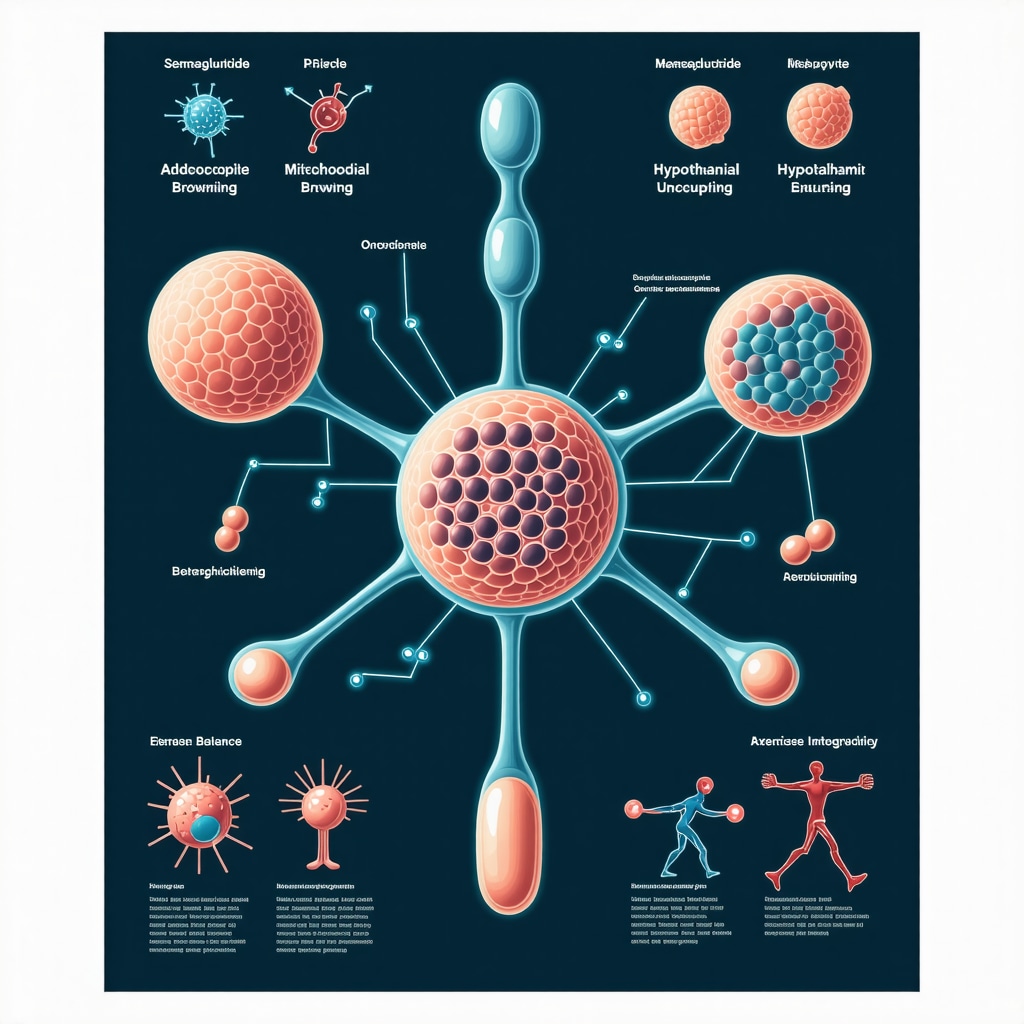
Diving deeper into the cellular level, Semaglutide’s GLP-1 receptor agonism modulates adipocyte biology in ways that extend beyond appetite suppression. Emerging research reveals that GLP-1 analogs promote browning of white adipose tissue—a process where energy-storing fat cells acquire thermogenic properties similar to brown fat. This browning increases basal metabolic rate by enhancing mitochondrial uncoupling, effectively turning fat into heat.
Moreover, Semaglutide influences central nervous system pathways that regulate energy homeostasis, particularly within the hypothalamus. By modulating neuropeptides involved in hunger and energy expenditure, it orchestrates a delicate balance between caloric intake and consumption. These insights provide a molecular rationale for observed sustained weight loss and improved metabolic profiles in Semaglutide users.
Could Semaglutide’s Effects on Adipose Tissue Browning Be Harnessed to Combat Metabolic Syndrome?
The potential of Semaglutide to induce adipose tissue browning opens intriguing therapeutic avenues for metabolic syndrome and related disorders. By elevating energy expenditure and improving insulin sensitivity, this mechanism could mitigate the core pathophysiology of metabolic syndrome beyond mere weight loss. Clinical trials focusing on biomarkers of thermogenesis and insulin resistance are underway to validate these hypotheses, promising a paradigm shift in obesity-related disease management.
Safety and Long-Term Considerations: Navigating the Complex Terrain of Chronic Semaglutide Use
While the benefits of Semaglutide are compelling, expert consensus emphasizes the necessity of vigilant long-term monitoring. Prolonged GLP-1 receptor activation may carry risks such as gastrointestinal disturbances, potential pancreatic effects, and rare but serious concerns regarding thyroid C-cell hyperplasia. Therefore, a multidisciplinary approach involving endocrinologists, dietitians, and primary care providers is essential to tailor therapy duration and mitigate risks.
Regular biochemical panels, imaging where appropriate, and patient-reported outcomes should be standard components of follow-up protocols. Additionally, strategies to prevent weight regain post-therapy include gradual dose tapering combined with sustained behavioral interventions, ensuring that the metabolic gains achieved with Semaglutide translate into lifelong wellness.
For an authoritative review of Semaglutide’s long-term safety and efficacy, consult the comprehensive analysis by the Journal of Clinical Endocrinology & Metabolism, which synthesizes data from multiple phase 3 trials and real-world evidence.
As the science of weight loss advances, integrating pharmacological innovation like Semaglutide with personalized metabolic and behavioral strategies offers unprecedented promise. Stay tuned as we delve deeper into optimizing patient outcomes through novel combinatory approaches and emerging technologies.
Unlocking Semaglutide’s Full Potential: Beyond Basics to Metabolic Mastery
While Semaglutide’s appetite suppression and gastric emptying delays are well-known, the cutting-edge of weight loss science reveals its profound influence on metabolic flexibility and cellular energy pathways. Harnessing these mechanisms requires a nuanced understanding that bridges pharmacology, nutrition, and exercise physiology—opening doors for highly personalized, rapid-fat-loss protocols.
How Can Semaglutide Be Strategically Integrated with Metabolic Flexibility to Optimize Fat Loss?
Metabolic flexibility—the body’s capacity to switch efficiently between carbohydrate and fat oxidation—is emerging as a pivotal factor in maximizing Semaglutide’s fat-burning efficacy. Protocols that combine Semaglutide with intermittent fasting and carb cycling, aligned to individual metabolic assessments via continuous glucose monitoring (CGM), enable real-time tailoring of nutrition and dosing schedules. This precision approach not only accelerates adipose tissue reduction but also enhances insulin sensitivity and mitochondrial function. For those interested, our detailed guide on combining Semaglutide with intermittent fasting offers actionable insights to jumpstart this synergy.
Exercise modalities like HIIT and resistance training complement this metabolic reprogramming by boosting mitochondrial density and promoting fat oxidation, providing a comprehensive fat-loss ecosystem when paired with Semaglutide.
Decoding Semaglutide at the Molecular Level: Adipocyte Browning and Energy Homeostasis
Recent molecular research indicates that Semaglutide induces browning of white adipose tissue, converting energy-storing fat into metabolically active, thermogenic fat. This browning effect enhances basal metabolic rate through mitochondrial uncoupling proteins, increasing energy expenditure independent of physical activity. Additionally, Semaglutide’s central nervous system actions modulate hypothalamic neuropeptides, exquisitely balancing hunger signals and energy expenditure pathways.
These cellular and neuroendocrine mechanisms help explain the sustained weight loss and improved metabolic profiles observed clinically, elevating Semaglutide from mere appetite suppressant to a comprehensive metabolic modulator.
Could Targeting Adipose Tissue Browning with Semaglutide Revolutionize Metabolic Syndrome Management?
Emerging clinical trials, including those reviewed by the Journal of Translational Medicine, are investigating Semaglutide’s role in promoting adipose browning as a therapeutic avenue to combat metabolic syndrome. By increasing thermogenesis and insulin sensitivity, this mechanism offers a promising adjunct to traditional treatments, potentially reducing cardiovascular risks and improving glycemic control beyond weight reduction alone.
Expert Tips for Safe, Effective Semaglutide Use in Complex Clinical Scenarios
Given the intricate interplay of Semaglutide with metabolic pathways and individual variability, expert supervision is paramount. Careful titration of dosage, vigilant monitoring for gastrointestinal or pancreatic effects, and integration with personalized nutritional and exercise plans ensure both safety and efficacy. For comprehensive dosage and safety guidelines, refer to our doctor-supervised Semaglutide dosage guidelines.
Moreover, long-term success hinges on embedding Semaglutide therapy within holistic wellness programs that emphasize behavioral change and metabolic health optimization.
Have you explored these advanced Semaglutide strategies, or are you curious about tailoring your regimen to your unique metabolism? Share your experiences or questions below, or connect with our specialists through the contact page to deepen your weight loss journey with expert guidance.
Expert Insights & Advanced Considerations
Strategic Integration of Metabolic Flexibility Amplifies Semaglutide’s Fat-Burning Efficacy
Maximizing Semaglutide’s impact requires more than just the medication itself. Incorporating metabolic flexibility protocols—such as personalized carb cycling and continuous glucose monitoring—can optimize substrate utilization, enabling the body to switch efficiently between fats and carbohydrates for fuel. This approach leverages Semaglutide’s appetite suppression synergistically with metabolic adaptability, accelerating adipose tissue loss beyond traditional calorie restriction methods.
Adipose Tissue Browning: A Molecular Game-Changer in Weight Management
Beyond appetite regulation, Semaglutide promotes the browning of white adipose tissue, enhancing thermogenesis and basal metabolic rate. This molecular mechanism transforms energy-storing fat into metabolically active fat, increasing energy expenditure independent of physical activity. Understanding and harnessing this process could revolutionize therapeutic strategies for metabolic syndrome and obesity, positioning Semaglutide as a metabolic modulator rather than solely an appetite suppressant.
Holistic Wellness Programs Are Essential for Sustainable Results
Long-term weight management success with Semaglutide depends heavily on embedding the medication within comprehensive wellness frameworks. These programs combine behavioral modification, nutritional education, and exercise regimens tailored to individual metabolic profiles. Such multidisciplinary approaches mitigate risks like weight regain post-therapy and ensure that metabolic improvements are sustained, emphasizing that Semaglutide is a catalyst within a broader lifestyle transformation.
Vigilant Monitoring Mitigates Risks in Complex Clinical Scenarios
Although Semaglutide is generally safe, chronic use necessitates careful monitoring to detect and manage potential gastrointestinal, pancreatic, or rare thyroid-related adverse effects. Expert-guided dosage titration and ongoing clinical assessments are critical to balancing efficacy with safety, particularly in patients with comorbidities or those on prolonged treatment courses.
Emerging Technologies Offer a New Frontier in Personalized Semaglutide Therapy
The integration of continuous metabolic tracking devices and AI-driven nutritional analytics presents exciting opportunities to refine Semaglutide dosing and dietary strategies in real-time. These technologies can tailor fasting protocols and macronutrient distributions to individual responses, potentially unlocking unprecedented rapid and sustainable fat loss outcomes.
Curated Expert Resources
- New England Journal of Medicine – Semaglutide Clinical Trials: A foundational source offering comprehensive peer-reviewed data on efficacy and safety, critical for understanding Semaglutide’s clinical profile.
- Doctor-Supervised Semaglutide Safe Dosage Guidelines: Essential for healthcare providers and patients seeking medically approved administration protocols to optimize outcomes and minimize side effects.
- Strategic Weight Loss Duo: Semaglutide and Intermittent Fasting: Explores the synergistic effects of combining pharmacotherapy with lifestyle interventions to accelerate fat burning.
- Journal of Clinical Endocrinology & Metabolism: Offers in-depth analyses of long-term safety data and metabolic effects, informing best practices in chronic Semaglutide use.
- Effective Medical Weight Loss Programs Combining Semaglutide and Lifestyle: Highlights multidisciplinary approaches that enhance therapeutic success and patient adherence.
Final Expert Perspective
Semaglutide stands at the forefront of rapid weight loss interventions in 2025, not merely as an appetite suppressant but as a sophisticated metabolic modulator. Its ability to induce adipose tissue browning, when combined with metabolic flexibility strategies and personalized lifestyle programs, transforms the landscape of obesity management. However, its full potential is unlocked only through expert supervision, vigilant monitoring, and integration with cutting-edge technologies that tailor therapy to individual metabolic nuances.
For those ready to elevate their understanding and application of Semaglutide, exploring the interplay between pharmacology, nutrition, and exercise is paramount. Delve deeper into optimizing your fat-burning journey by visiting our detailed guide on combining Semaglutide with intermittent fasting and consider connecting with specialists via our contact page to tailor your approach with expert insights.

