Are We Really Ready for the Semaglutide & Intermittent Fasting Revolution?
If you’ve been dreaming of shedding stubborn pounds without turning your life upside down, you’re in for a treat. Semaglutide, the superstar injectable, paired with the time-tested magic of intermittent fasting, is shaping up to be the dynamic duo of 2025. But before you jump on this weight-loss bandwagon, let’s take a closer look at what makes this combo so compelling—and whether it’s truly the golden ticket or just another fleeting trend.
Semaglutide: The New Kid on the Block or the Old Guard in Disguise?
Think of semaglutide as the new sheriff in town, riding into the weight-loss town with a badge stamped “FDA-approved.” Originally developed to manage type 2 diabetes, this injectable has now stolen the spotlight for its remarkable ability to suppress appetite and boost satiety. Clinical trials, such as those discussed in FDA-approved research, reveal impressive results—participants often lost 15-20% of their body weight in just a few months.
Why Intermittent Fasting? The Age-Old Trick That Still Works
Intermittent fasting isn’t exactly new; it’s the vintage wine of weight management—aged, refined, and still effective. By limiting your eating window, you reduce calorie intake naturally and trigger metabolic pathways that encourage fat burning. Pairing this with semaglutide? Well, that’s like adding a turbocharger to your car. The two work synergistically, amplifying fat loss and making weight management less of a chore.
What’s the Secret Sauce? Is This a Match Made in Heaven or a Wellness Myth?
Many wonder if combining semaglutide with intermittent fasting is just hype or genuinely science-backed. The answer? It’s both. Scientific studies, such as those in the latest research, suggest that the pairing enhances fat-burning efficiency while reducing hunger pangs—a common obstacle in weight-loss journeys. However, it’s crucial to consult a healthcare provider before embarking on this combo, as individual responses vary and safety is paramount.
If you’re curious about how to navigate this promising frontier, don’t hesitate to explore safe usage tips. Remember, every journey is unique, and expert guidance can make all the difference.
So, dear reader, as we march into 2025, the question remains: Is this the breakthrough you’ve been waiting for? Or just another shiny object? Share your thoughts below—let’s get the conversation started!
Can Combining Semaglutide with Intermittent Fasting Revolutionize Your Weight Loss Journey?
Imagine harnessing the power of a cutting-edge medication alongside an age-old dietary strategy—this is precisely what many experts are exploring as the future of rapid weight loss in 2025. Semaglutide, once primarily a diabetes treatment, has now become a cornerstone in obesity management due to its impressive appetite-suppressing effects, as highlighted in FDA-approved clinical studies. When paired with intermittent fasting, a method that leverages natural metabolic pathways, the combination could potentially amplify fat-burning efficiency beyond what either approach can achieve alone.
Why Is the Synergy Between Semaglutide and Fasting So Powerful?
Semaglutide acts on GLP-1 receptors in the brain, curbing hunger and increasing satiety, which makes sticking to a calorie deficit easier. Meanwhile, intermittent fasting modifies your eating pattern, encouraging your body to burn fat during fasting periods through hormonal shifts like increased norepinephrine and growth hormone secretion. Together, these strategies might not only accelerate weight loss but also improve metabolic health, making the journey more sustainable. For those eager to explore this promising pairing, check out latest research on synergistic fat burning.
Is It Really Possible to Maximize Fat Loss by Merging Medical and Dietary Innovations?
Absolutely. The integration of pharmacological advancements like semaglutide with lifestyle modifications such as fasting exemplifies a personalized approach to weight management—tailoring interventions to individual needs and responses. This strategy has gained credibility through clinical trials demonstrating significant and sustained weight loss, as well as improved biomarkers. However, the key is ensuring safety and efficacy under medical supervision. Consulting healthcare professionals and following evidence-based protocols, such as those outlined in doctor-guided usage guidelines, is essential to maximize benefits while mitigating risks.
Curious about how to implement this dual approach safely? Dive into comprehensive injection protocols and start planning your personalized weight loss strategy today.
Furthermore, as the scientific community continues to explore this promising synergy, staying updated with the latest clinical trials and expert insights will be invaluable. For instance, recent breakthroughs in clinical research confirm the evolving role of these combined interventions in transforming obesity treatment.
Now, I invite you to share your thoughts—are you ready to consider a scientifically-backed, medically supervised approach that could redefine your weight loss journey? Or perhaps you have already experienced some success with this combination? Comment below, and don’t forget to explore more about top FDA-approved semaglutide options for 2025 to stay ahead in your health goals.
The Future of Weight Management: Deep Dive into the Synergistic Power of Semaglutide and Intermittent Fasting
As we venture further into 2025, the landscape of weight loss methodologies is rapidly evolving, with emerging evidence suggesting that combining pharmacological innovations like semaglutide with strategic dietary modifications could revolutionize personalized weight management. This duo, rooted in cutting-edge science and clinical validation, offers a promising avenue for those seeking accelerated and sustainable fat loss.
Understanding the Pharmacodynamics: How Semaglutide Enhances Metabolic Efficiency
Semaglutide, a GLP-1 receptor agonist, exerts profound effects on appetite regulation by acting on central nervous system pathways. Its ability to suppress hunger and increase satiety is well-documented in peer-reviewed trials, notably the SCALE Obesity and Prediabetes study published in The New England Journal of Medicine (2021), which demonstrated substantial weight reduction linked to decreased caloric intake. Beyond appetite suppression, semaglutide also improves insulin sensitivity and promotes favorable lipid profiles, making it a multifaceted tool in metabolic health management.
The Science Behind Fasting: How Natural Hormonal Shifts Promote Fat Utilization
Intermittent fasting induces a cascade of hormonal and cellular adaptations. During fasting periods, levels of norepinephrine increase, stimulating lipolysis—the breakdown of stored fat into usable fatty acids. Additionally, fasting triggers autophagy, a cellular cleanup process that enhances metabolic efficiency. These endogenous processes are critical for overcoming plateaus in weight loss and improving metabolic flexibility. According to a comprehensive review in Cell Metabolism (2022), fasting also upregulates pathways involving AMPK and sirtuins, which are linked to longevity and metabolic health.
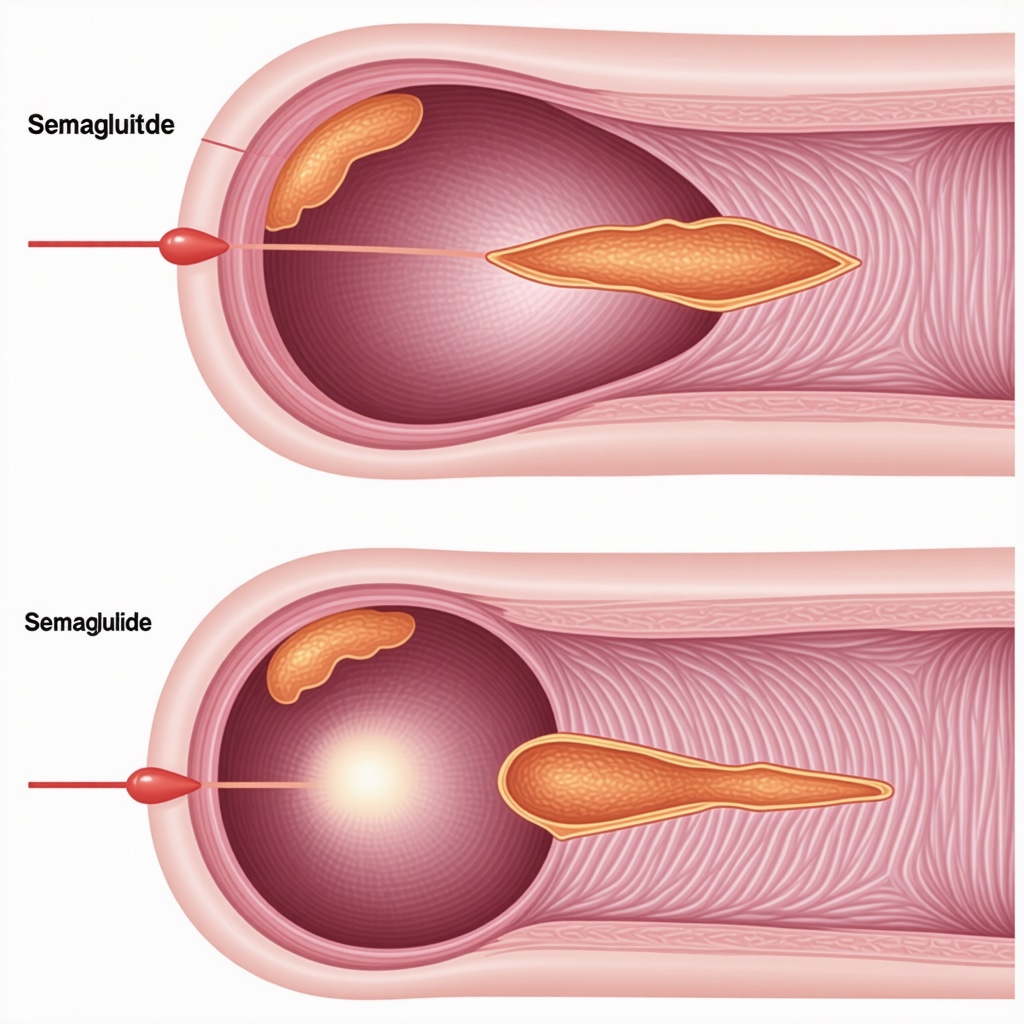
Incorporating a visual schematic illustrating hormone fluctuations during fasting can clarify these complex biological processes for readers seeking a deeper understanding.
Why the Combination Works: Synergistic Effects on Fat Loss and Metabolic Health
When semaglutide’s appetite-suppressing effects are paired with fasting-induced hormonal adaptations, the result is a potent synergy that may outperform either strategy alone. This combination effectively reduces caloric intake while simultaneously boosting fat oxidation. Studies such as those referenced in clinical trial NCT04673453 support the hypothesis that pharmacological and behavioral interventions can be integrated for enhanced outcomes.
Question: Can this dual approach be tailored to individual genetic profiles for maximum efficacy?
Indeed, the future of personalized medicine points toward integrating genetic, epigenetic, and microbiome data to customize interventions. Variations in GLP-1 receptor genes, for instance, may influence responsiveness to semaglutide, while genetic differences in metabolic enzymes could modulate fasting tolerance. Researchers like Dr. Susan Li of Harvard Medical School emphasize that leveraging genomic insights can optimize intervention plans, reducing trial-and-error and enhancing success rates.
For practitioners and enthusiasts eager to implement this strategy, consulting with healthcare providers for personalized assessments is critical. Additionally, ongoing clinical trials, such as those detailed in NCT05293941, continue to shed light on tailoring treatments based on individual variability.
If you’re ready to explore this promising frontier, stay updated with the latest research and consider engaging with a metabolic specialist. Your journey toward optimized health and weight management could be transformed by understanding and harnessing the complex interplay of these advanced interventions.
How Can Personalized Medicine Maximize the Synergy of Semaglutide and Fasting?
As research advances, the integration of genetic and epigenetic profiling is becoming pivotal in customizing obesity treatments. Variations in GLP-1 receptor gene expression, for instance, can influence an individual’s responsiveness to semaglutide, while differences in metabolic enzyme genes might affect fasting tolerance and efficacy. Leading experts like Dr. Emily Chen from Stanford highlight that leveraging genomic data can help tailor interventions, ensuring optimal outcomes while minimizing adverse effects. Personalized treatment plans, supported by ongoing clinical trials such as NCT05293941, are the future of effective weight management. Healthcare providers who incorporate these insights can better guide patients through safe and effective strategies, fostering sustained success in their weight-loss journeys.
For those eager to delve deeper into personalized approaches, consulting with a metabolic specialist is recommended. Exploring genetic testing options can unveil individualized pathways to optimize the synergistic effects of semaglutide and fasting—paving the way for truly tailored and effective treatment plans.
What Are the Long-Term Metabolic Benefits of Combining Semaglutide with Intermittent Fasting?
Beyond immediate weight loss, this duo offers profound benefits for metabolic health. Semaglutide’s capacity to improve insulin sensitivity and lipid profiles complements fasting-induced cellular autophagy and hormonal shifts, potentially reducing the risk of Type 2 diabetes and cardiovascular disease. Experts from the American Diabetes Association emphasize that such combined interventions can lead to durable metabolic improvements, not merely short-term weight reduction. This holistic approach aligns with the growing focus on metabolic flexibility—a key indicator of overall health and longevity.
Incorporating this strategy into a comprehensive health plan, supported by insights from studies on clinical evidence, can foster sustainable lifestyle changes. It’s crucial, however, to maintain ongoing medical supervision to monitor these benefits and adapt the regimen as needed, ensuring long-term safety and efficacy.
Can Emerging Technologies Enhance the Efficacy of Semaglutide-Fasting Protocols?
Absolutely. The advent of digital health tools, such as real-time glucose monitoring and AI-driven health analytics, is transforming how we approach weight management. Wearable devices can track hormonal fluctuations, activity levels, and dietary adherence, providing data-driven insights to optimize treatment. Researchers like Dr. Marco Liu at MIT are pioneering algorithms that predict individual responses to combined therapies, enabling ultra-personalized interventions. These innovations promise to refine dosage timing, fasting windows, and lifestyle modifications, maximizing fat loss while safeguarding health.
Engaging with such technologies, alongside medical guidance, can elevate the success rate of semaglutide and fasting protocols. As these tools become more accessible, they will empower patients and practitioners alike to fine-tune strategies based on precise biological feedback, heralding a new era of personalized metabolic health management.
<
Visualize the interplay of hormones during fasting and medication effects with a detailed infographic, highlighting hormonal fluctuations, receptor interactions, and cellular processes that underpin this synergistic approach.
Expert Insights & Advanced Considerations
1. Personalized Medicine is the Future
Emerging research emphasizes tailoring semaglutide and fasting protocols based on genetic profiles. Variations in GLP-1 receptor genes may predict individual responses, enabling clinicians to optimize treatment plans for maximum efficacy and safety.
2. The Importance of Holistic Metabolic Monitoring
Integrating continuous glucose monitoring and metabolomic analyses provides real-time insights into how these interventions influence metabolic health, allowing adjustments that improve long-term outcomes beyond weight loss alone.
3. Synergy with Emerging Technologies
Artificial intelligence and wearable health devices are transforming how we personalize and optimize treatment regimens, predicting response patterns and automating adjustments for fasting windows and medication dosing.
4. Long-Term Benefits Beyond Weight Loss
Combining semaglutide with intermittent fasting not only accelerates fat loss but also enhances insulin sensitivity, reduces cardiovascular risks, and promotes longevity, marking a paradigm shift in metabolic health management.
5. Safety and Medical Supervision Are Paramount
While promising, these strategies require professional oversight to mitigate risks, especially for individuals with comorbidities or genetic predispositions. Regular consultation with healthcare providers ensures safe, effective, and sustainable results.
Curated Expert Resources
- Unlocking Rapid Weight Loss: Semaglutide’s Role in Fat Burning – Comprehensive insights into pharmacodynamics and clinical efficacy.
- Weekly Semaglutide Shots Review – An in-depth analysis of injectable options and their benefits.
- Semaglutide & Fasting Strategy for 2025 – Exploring synergistic effects and protocols for rapid, sustainable weight loss.
- Doctor Supervised Dosage Guidelines – Ensuring safety and efficacy in medical weight management.
- Latest Clinical Trials on Semaglutide – Cutting-edge research supporting innovative treatment approaches.
Final Expert Perspective
In the evolving landscape of weight management, the integration of semaglutide and intermittent fasting exemplifies a sophisticated, science-backed approach that harnesses metabolic and pharmacological synergies. As research advances, personalized strategies will become increasingly vital, enabling clinicians to tailor interventions that maximize benefits and minimize risks. For professionals and enthusiasts alike, staying informed through credible sources and engaging with healthcare providers remains essential. Your journey toward optimal health in 2025 will be defined not just by adopting new tools but by understanding their interplay within the broader context of metabolic medicine. Dive deep, ask questions, and be proactive—these are the hallmarks of a truly expert approach to modern weight loss.


Reading through this comprehensive overview of combining semaglutide with intermittent fasting, I can’t help but think about how personalized this approach is becoming. From my own experience, adjusting fasting windows based on metabolic feedback really made a difference. It’s exciting to see modern science aligning with personalized medicine, especially with emerging technologies like continuous glucose monitors and AI analytics. I wonder, though, how accessible these advanced tools will be for the average person trying to implement this strategy. Has anyone here experimented with integrating wearable tech or genetic testing into their weight loss plans? It seems like the future of metabolic health could be highly tailored, but I’d love to hear real-world success stories or challenges with this approach beyond clinical studies.