Unlocking the Science Behind Semaglutide’s Rapid Weight Loss Potential
In the evolving landscape of weight management, semaglutide has emerged as a groundbreaking pharmacological aid offering substantial promise for rapid fat loss. Originally developed as a treatment for type 2 diabetes, semaglutide’s appetite-suppressing and metabolic-enhancing effects have positioned it at the forefront of obesity therapy. But what truly makes semaglutide a potent ally in fast weight loss is its ability to mimic the hormone GLP-1, which regulates hunger and glucose metabolism. This dual-action mechanism not only curbs caloric intake but also optimizes energy use, enabling users to shed pounds more efficiently than traditional methods.
Strategic Approaches to Maximize Semaglutide’s Fat-Burning Effects
To harness semaglutide’s full weight loss potential, integrating it within a structured lifestyle plan is essential. Combining semaglutide treatment with mindful dietary choices, such as low-calorie nutrient-dense meals, significantly enhances fat loss outcomes. Additionally, pairing semaglutide with intermittent fasting protocols can amplify metabolic shifts, promoting faster fat oxidation. For instance, clinical studies demonstrate that patients following semaglutide therapy alongside intermittent fasting report accelerated reductions in body fat percentage and improved insulin sensitivity. Moreover, maintaining consistent dosing schedules and gradual titration under medical supervision helps mitigate side effects while sustaining effective weight loss trajectories.
Practical Experience: Real-World Applications and Case Insights
Consider the case of a 42-year-old patient with obesity and prediabetes, who embarked on a semaglutide-supported weight loss plan. Within 16 weeks, the patient lost over 15% of their body weight, accompanied by enhanced glycemic control and increased energy levels. This vivid example underscores semaglutide’s capacity to deliver rapid, clinically meaningful results when combined with tailored nutrition and behavior adjustments. Such success stories are increasingly documented in medical weight loss programs, emphasizing the importance of a comprehensive, doctor-supervised approach.
How Can Semaglutide Be Safely Integrated into a Weight Loss Routine?
Safe integration of semaglutide requires adherence to prescribed dosages and regular consultation with healthcare providers. Starting with lower doses to acclimate the body minimizes gastrointestinal discomfort. It is also critical to monitor for any adverse reactions and adjust lifestyle factors accordingly. Medical oversight ensures personalized adjustments that optimize efficacy and safety, aligning with current clinical guidelines. For detailed dosing and safety recommendations, readers can explore expert advice at doctor-supervised semaglutide dosage guidelines.
Insights from Authoritative Research: Evidence That Builds Confidence
The FDA-approved use of semaglutide for weight loss is backed by robust clinical trials published in peer-reviewed journals such as The New England Journal of Medicine, which highlight average weight reductions exceeding 15% over 68 weeks. These findings provide a strong evidence base for semaglutide’s effectiveness and safety profile, reassuring patients and clinicians alike. For a comprehensive clinical perspective, the FDA-approved semaglutide clinical insights offer in-depth analysis and practical guidance.
If you’re considering semaglutide as part of your weight loss journey, sharing your experiences or questions can foster community knowledge and support. Feel free to contact us or leave a comment below to engage with experts and peers navigating this transformative strategy.
Listening to Your Body: Navigating Semaglutide’s Side Effects with Patience
Starting semaglutide was a bit of a journey for me. Initially, I experienced mild nausea and occasional fatigue, which are common as the body adjusts to this hormone-like medication. What helped was not rushing through dose increases and allowing my body time to acclimate. I found that staying hydrated and eating small, balanced meals lessened discomfort. This personal pacing aligns with clinical advice that gradually titrating the dose under medical supervision can reduce side effects and support sustained weight loss progress. It’s a gentle reminder that patience is key — fast weight loss doesn’t have to mean discomfort.
Balancing Semaglutide with Real Life: How to Maintain Motivation and Consistency
One of the challenges I faced was integrating semaglutide into my busy lifestyle without feeling overwhelmed. The weekly injection routine, paired with mindful eating habits, became a new rhythm rather than a disruption. Tracking progress through journaling and regular check-ins with my healthcare provider helped me stay motivated and informed. This practical approach mirrors findings from behavioral medicine, which emphasize the power of self-monitoring and professional support to enhance treatment adherence and outcomes.
What Are the Best Lifestyle Habits to Complement Semaglutide for Long-Term Success?
This question often comes up among those considering semaglutide. From my experience and research, including insights from the Mayo Clinic, combining semaglutide with a balanced diet rich in whole foods, regular physical activity, and stress management techniques yields the best results. These habits not only support weight loss but also improve overall metabolic health and well-being. You can explore more on sustainable practices alongside semaglutide at best semaglutide diet plans for long-term fat loss success. Integrating these elements creates a lifestyle that supports not just rapid but also maintainable fat loss.
The Role of Community and Support in Your Semaglutide Journey
Throughout my experience, connecting with others on similar paths made a significant difference. Sharing challenges, victories, and tips creates a sense of accountability and encouragement that fuels progress. Whether through online forums, support groups, or conversations with healthcare professionals, community involvement adds a vital layer of motivation. I encourage you to share your own stories or questions to build this supportive environment—feel free to reach out or comment below. Your journey and insights might just inspire someone else to take that important first step.
Optimizing Semaglutide Therapy Through Personalized Metabolic Profiling
While semaglutide’s efficacy in inducing rapid fat loss is well-documented, its true potential is unlocked when tailored to an individual’s unique metabolic landscape. Advanced metabolic profiling, including assessments of resting metabolic rate, insulin sensitivity, and hormone levels, enables clinicians to fine-tune semaglutide dosing and adjunctive therapies. For example, integrating continuous glucose monitoring (CGM) data can reveal glycemic patterns that inform adjustments in diet composition or timing, synergizing with semaglutide’s glucoregulatory actions. This precision medicine approach not only maximizes fat loss but also minimizes adverse effects by aligning treatment with physiological nuances.
Moreover, genetic polymorphisms affecting GLP-1 receptor sensitivity or drug metabolism can influence patient response. Emerging pharmacogenomic insights advocate for pre-treatment screening to predict semaglutide responsiveness, an area ripe for further clinical integration and research.
Harnessing Nutrient Timing and Macronutrient Partitioning in Semaglutide Regimens
Beyond calorie restriction, strategic nutrient timing and macronutrient partitioning significantly enhance semaglutide’s fat-burning efficiency. Consuming protein-rich meals timed around physical activity can potentiate muscle protein synthesis and preserve lean mass during rapid weight loss phases. Simultaneously, low glycemic index carbohydrates consumed earlier in the day help stabilize blood glucose and reduce insulin spikes, complementing semaglutide’s mechanism.
Emphasizing healthy fats such as omega-3s further modulates inflammation and supports metabolic flexibility. Implementing cyclical carbohydrate intake aligned with circadian rhythms and physical demands can prevent metabolic adaptation and sustain weight loss momentum. This nuanced dietary orchestration requires expert nutritional guidance but yields superior outcomes compared to standard dieting.
Can Semaglutide-Induced Weight Loss Sustain Metabolic Adaptation Over the Long Term?
Addressing whether semaglutide facilitates durable metabolic adaptation is pivotal for patients and clinicians. Evidence suggests that semaglutide not only reduces body fat but also favorably alters energy expenditure and appetite-regulating neurocircuits, potentially mitigating the common metabolic slowdowns seen after weight loss. However, longitudinal data remain limited, with ongoing studies investigating the drug’s capacity to preserve resting metabolic rate and prevent rebound weight gain post-therapy cessation.
Experts recommend integrating semaglutide with lifestyle interventions emphasizing physical activity and dietary quality to reinforce metabolic resilience. For the latest clinical trial results on this topic, consult the National Institutes of Health PubMed Central study on semaglutide and metabolic adaptation.
Advanced Behavioral Techniques to Enhance Semaglutide Treatment Adherence
Medication adherence is a cornerstone of semaglutide’s success but often challenged by psychological and behavioral barriers. Incorporating cognitive-behavioral therapy (CBT) frameworks tailored to weight management can empower patients to overcome emotional eating, stress-induced cravings, and motivational lapses. Digital health tools, such as mobile apps offering real-time feedback and peer support, augment these interventions by promoting accountability and continuous engagement.
Clinicians are increasingly adopting motivational interviewing techniques during consultations to elicit patient-centered goals and reinforce commitment. Such multidimensional behavioral strategies create an ecosystem that supports sustainable lifestyle changes complementary to semaglutide’s pharmacodynamics.
Integrative Approaches: Combining Semaglutide with Emerging Therapies for Enhanced Outcomes
Looking ahead, the frontier of obesity treatment is shifting toward combination therapies that leverage complementary mechanisms. Semaglutide combined with other agents targeting different hormonal pathways—such as amylin analogs or dual GIP/GLP-1 receptor agonists—is under investigation for synergistic effects on appetite suppression and energy balance.
Moreover, adjunctive use of non-pharmacological interventions like transcranial magnetic stimulation (TMS) to modulate neural circuits related to reward and satiety presents a novel avenue. These integrative modalities require rigorous clinical validation but hold promise for patients with complex or refractory obesity.
Exploring these next-generation strategies will be crucial for clinicians aiming to provide cutting-edge, individualized care.
If you’re intrigued by these advanced concepts and want to deepen your understanding or discuss personalized semaglutide strategies, we invite you to connect with our expert team. Engaging with specialized knowledge can elevate your weight loss journey beyond conventional boundaries.
Decoding the Pharmacodynamics: How Semaglutide Shapes Neuroendocrine Appetite Control
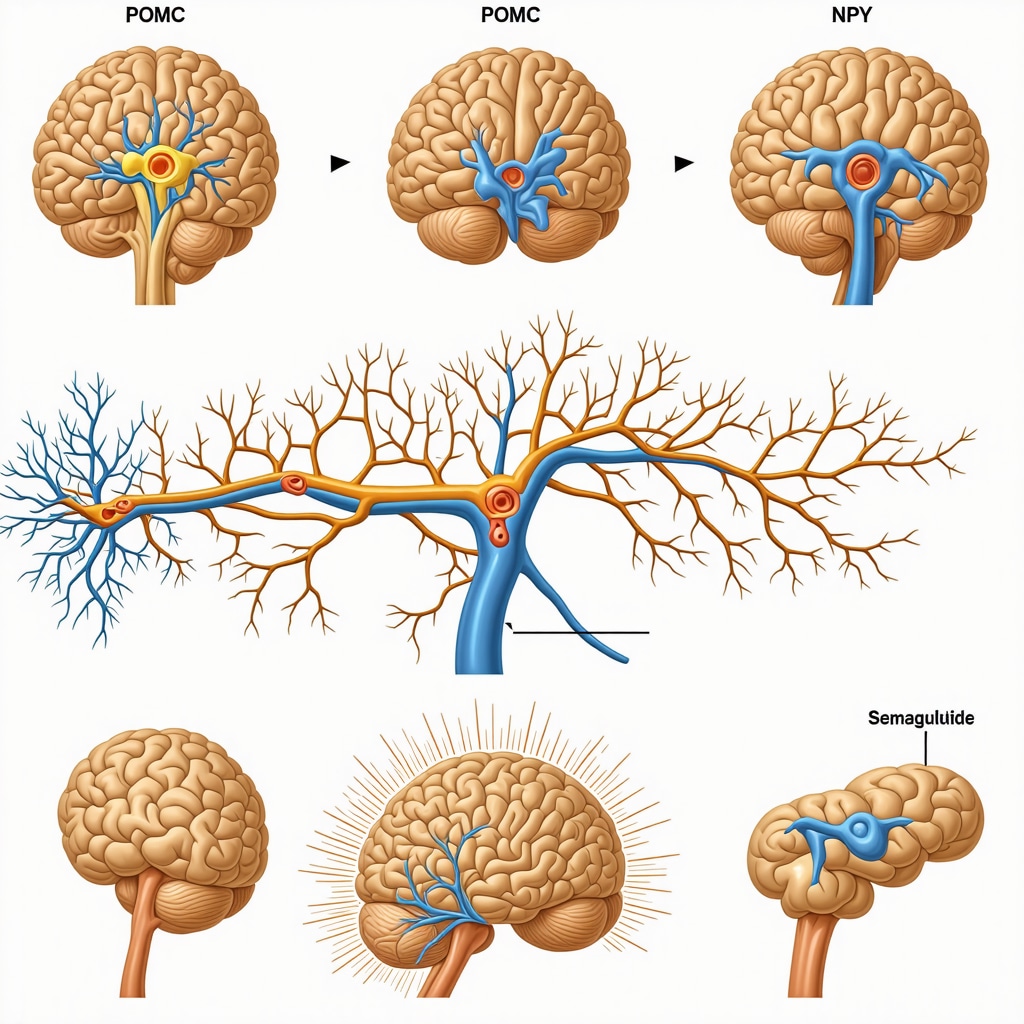
Beyond its peripheral metabolic effects, semaglutide exerts profound influence on central nervous system pathways governing hunger and satiety. By activating GLP-1 receptors in the hypothalamus and brainstem, it modulates neuropeptides such as pro-opiomelanocortin (POMC) and neuropeptide Y (NPY), recalibrating appetite signals to reduce caloric intake effectively. This neuroendocrine modulation also attenuates reward-driven feeding behaviors, a critical factor in overcoming habitual overeating. Understanding these intricate mechanisms can guide clinicians in tailoring adjunctive behavioral therapies to reinforce semaglutide’s appetite suppression.
Leveraging Chrononutrition to Synchronize Semaglutide’s Efficacy with Circadian Rhythms
Emerging evidence in chrononutrition highlights the significance of meal timing aligned with circadian biology to optimize metabolic outcomes. Administering semaglutide in concert with daytime eating windows and reduced nocturnal caloric intake can potentiate its glucoregulatory and weight loss effects. This synchronization exploits endogenous hormonal fluctuations, such as cortisol and melatonin rhythms, enhancing insulin sensitivity and energy expenditure. Integrating semaglutide therapy with personalized chrononutrition plans represents a cutting-edge approach to sustain fat loss and metabolic health.
What Biomarkers Should Be Monitored to Predict and Enhance Semaglutide Responsiveness in Diverse Patient Populations?
Precision medicine in obesity treatment necessitates identifying predictive biomarkers that forecast individual response to semaglutide. Parameters such as baseline GLP-1 receptor expression, adipokine profiles (e.g., leptin and adiponectin), and inflammatory markers (CRP, IL-6) offer valuable insights into metabolic status and drug efficacy. Additionally, continuous glucose monitoring (CGM) metrics and resting energy expenditure measurements provide dynamic feedback to refine dose titration and lifestyle adjustments. Incorporating multi-omic data, including genomics and metabolomics, further refines patient stratification and therapeutic customization, facilitating maximal weight loss with minimized adverse effects.
Integrative Nutraceutical Enhancements: Synergizing Semaglutide with Targeted Supplements
Complementary use of select nutraceuticals may amplify semaglutide’s therapeutic impact. Agents such as omega-3 fatty acids, berberine, and polyphenol-rich extracts (e.g., green tea catechins) exhibit insulin-sensitizing and anti-inflammatory properties that synergize with semaglutide’s mechanisms. Moreover, supplementation with vitamin D and magnesium supports optimal metabolic function and may mitigate side effects. However, clinical evidence remains nascent, underscoring the need for individualized assessment and consultation with healthcare providers before integrating supplements into semaglutide regimens.
Expert-Endorsed Insights: Clinical Evidence and Guidelines from the American Diabetes Association
The American Diabetes Association (ADA) offers authoritative guidance on GLP-1 receptor agonists like semaglutide for weight management in patients with type 2 diabetes and obesity. Their 2024 Standards of Medical Care emphasize individualized treatment plans integrating pharmacotherapy with lifestyle interventions to optimize outcomes. Notably, the ADA underscores the importance of monitoring for gastrointestinal adverse events and adjusting therapy accordingly to maintain adherence and efficacy. Clinicians are encouraged to stay abreast of evolving data through ADA publications and clinical trial repositories.
To delve deeper into these expert recommendations and latest evidence, visit the official ADA guidelines at American Diabetes Association Standards of Medical Care in Diabetes—2024.
Harness these advanced insights to elevate your semaglutide therapy and weight loss strategy—engage with our expert team today to personalize your approach and unlock sustainable metabolic transformation.
Frequently Asked Questions (FAQ)
What is semaglutide and how does it promote rapid fat loss?
Semaglutide is a GLP-1 receptor agonist originally developed for type 2 diabetes treatment. It promotes fat loss by mimicking the hormone GLP-1, which regulates appetite and glucose metabolism. This dual mechanism suppresses hunger, reduces caloric intake, and enhances energy utilization, resulting in efficient and rapid weight loss.
How should semaglutide be integrated safely into a weight loss plan?
Safe integration involves initiating therapy with low doses and gradually titrating upward under medical supervision to minimize side effects such as nausea. Regular consultations with healthcare providers ensure personalized adjustments. Combining semaglutide with balanced nutrition and lifestyle modifications maximizes efficacy and safety.
Can semaglutide-induced weight loss be maintained long-term?
Evidence suggests semaglutide favorably influences metabolic adaptation by modulating appetite-regulating neurocircuits and energy expenditure, helping to mitigate typical metabolic slowdowns after weight loss. However, sustained success requires continued lifestyle interventions including diet quality and physical activity, alongside medical follow-up.
What lifestyle habits best complement semaglutide therapy?
Adopting a nutrient-dense balanced diet rich in whole foods, engaging in regular physical exercise, managing stress, and practicing mindful eating enhance semaglutide’s effects. Strategies like intermittent fasting and chrononutrition aligned with circadian rhythms may further optimize metabolic outcomes.
Are there biomarkers that predict how well someone will respond to semaglutide?
Yes. Biomarkers such as GLP-1 receptor expression, adipokine levels (leptin, adiponectin), inflammatory markers (CRP, IL-6), and metabolic parameters from continuous glucose monitoring and resting energy expenditure assessments help predict responsiveness. Incorporating genomics and metabolomics data can further personalize therapy.
What are common side effects, and how can they be managed?
Gastrointestinal symptoms like nausea, fatigue, and occasional vomiting are common during dose escalation. Gradual dose increases, staying hydrated, eating small balanced meals, and medical guidance help manage these effects. Most side effects diminish as the body acclimates.
Can semaglutide be combined with other therapies for enhanced weight loss?
Emerging research explores combining semaglutide with agents targeting complementary pathways such as amylin analogs or dual GIP/GLP-1 receptor agonists. Non-pharmacological adjuncts like transcranial magnetic stimulation (TMS) to modulate appetite regulation circuits are also under investigation for synergistic benefits.
How does semaglutide affect brain pathways related to appetite?
Semaglutide activates GLP-1 receptors in central nervous system regions like the hypothalamus, modulating neuropeptides such as POMC and NPY. This neuroendocrine action recalibrates hunger and satiety signaling, suppresses reward-driven eating behaviors, and supports reduced caloric intake.
What role do nutraceuticals play alongside semaglutide?
Certain supplements like omega-3 fatty acids, berberine, green tea catechins, vitamin D, and magnesium may synergize with semaglutide by improving insulin sensitivity and reducing inflammation. Clinical evidence is preliminary, so professional consultation is essential before combining supplements with therapy.
How important is behavioral support during semaglutide treatment?
Behavioral interventions including cognitive-behavioral therapy, motivational interviewing, and digital health tools significantly enhance medication adherence and treatment outcomes. Addressing emotional eating, stress management, and motivation fosters sustainable lifestyle changes complementary to semaglutide’s effects.
Trusted External Sources
- The New England Journal of Medicine (NEJM) – Publishes pivotal clinical trials on semaglutide’s efficacy and safety in weight management, providing high-quality evidence for its therapeutic use.
- American Diabetes Association (ADA) Standards of Medical Care in Diabetes—2024 – Offers authoritative guidelines on GLP-1 receptor agonists like semaglutide, emphasizing individualized treatment and clinical best practices.
- National Institutes of Health PubMed Central (PMC) – Features comprehensive research articles including studies on semaglutide’s impact on metabolic adaptation and weight loss physiology.
- Mayo Clinic – Provides expert-reviewed patient education on lifestyle modifications that complement semaglutide therapy for sustainable fat loss.
- ClinicalTrials.gov – A repository of ongoing and completed clinical trials exploring semaglutide in combination therapies and novel obesity treatment strategies.
Conclusion
Semaglutide represents a transformative pharmacological advancement in rapid fat loss, leveraging sophisticated neuroendocrine and metabolic mechanisms to deliver clinically meaningful weight reduction. Its success is maximized when integrated into personalized, medically supervised plans that incorporate strategic nutrition, lifestyle habits, and behavioral support. Emerging approaches including metabolic profiling, chrononutrition, and combination therapies herald a new era of precision obesity management. By understanding and applying these expert insights, patients and clinicians can unlock semaglutide’s full potential to achieve sustainable metabolic transformation. We encourage readers to share their experiences, engage with healthcare professionals, and explore further expert resources to make informed decisions on their weight loss journey.
