Unveiling the Magic of Semaglutide: Miracle or Myth in Fat Loss?
Ever wondered if there’s a shortcut to shedding pounds faster than you can say “diet and exercise”? Well, buckle up, because semaglutide fat burning injections are turning heads in the weight loss community. This injectable marvel isn’t just another fad; it’s backed by clinical trials and medical endorsements, promising rapid fat loss with a dash of scientific flair.
Injectable Revolution: How Semaglutide Is Changing the Weight Loss Game
Imagine a tiny shot that curbs your appetite, stabilizes blood sugar, and accelerates fat burning—all while you binge-watch your favorite series. Sounds like sci-fi? Nope, it’s real. Semaglutide, originally developed for type 2 diabetes, has emerged as a superstar in obesity management. The key? Its ability to mimic GLP-1 hormone, which tells your brain you’re full, effectively turning off hunger signals.
Is It Safe? Navigating the Fine Line Between Innovation and Risk
Of course, with great power comes great responsibility. The safety profile of semaglutide has been scrutinized extensively, with FDA-approved versions showing promising results. However, it’s crucial to remember that dosage and medical supervision are paramount. As with any potent medication, potential side effects like nausea or fatigue are worth noting—so, consult your doctor before jumping in.
Could Semaglutide Be Your Weight Loss Game-Changer?
Now, here’s a question that stirs curiosity—could this injectable be the answer to those stubborn pounds? Many patients report impressive results, transforming their bodies and lives in just weeks. But is it sustainable? While some tout semaglutide as a miracle, experts emphasize combining it with lifestyle changes for lasting success. Want to see real stories? Check out these inspiring patient stories.
For those eager to explore further, detailed clinical insights and expert guidelines are available at this authoritative source.
If you’re contemplating whether semaglutide injections suit your weight loss journey, remember—it’s a tool, not a magic wand. The right approach combines science, medical oversight, and your commitment to a healthier lifestyle. Ready to take the plunge? Share your thoughts below or reach out to our experts.
Is Semaglutide the Secret Weapon for Accelerated Fat Loss?
As more individuals seek swift and effective weight loss solutions, the spotlight on semaglutide continues to grow. This injectable medication, originally designed for type 2 diabetes, has gained recognition for its potent ability to suppress appetite and promote fat reduction. But beyond its clinical roots, how does it perform in real-world scenarios, and what considerations should users keep in mind? Experts emphasize that combining semaglutide with personalized lifestyle changes, such as diet and exercise, is key to sustainable results. For those eager to explore comprehensive treatment options, medical programs like these leading medical weight loss programs leverage the power of semaglutide for rapid outcomes.
What Are the Practical Implications of Using Semaglutide for Fast Fat Loss?
Understanding the practical aspects involves considering dosage, administration, and safety measures. The clinical success stories documented in sources such as this FDA-approved guide highlight the importance of medical supervision. Proper dosing, tailored to individual needs, minimizes risks like nausea or gastrointestinal discomfort. Moreover, integrating semaglutide with intermittent fasting or specific diet plans can amplify fat-burning effects, as discussed in these expert strategies.
Could Semaglutide Be the Catalyst for Your Weight Loss Journey?
Here’s a provocative question—could this injectable be the catalyst you need to break through weight loss plateaus? Many users report rapid transformations, yet long-term success hinges on lifestyle commitment. The question then becomes: how can you harness semaglutide’s potential safely and effectively? Consulting with healthcare providers and following guidelines such as doctor-supervised dosage tips ensures a balanced approach. For further insights, check out this detailed clinical review.
Have you considered how integrating semaglutide with lifestyle modifications could redefine your weight loss trajectory? Share your thoughts below or reach out to our experts for personalized guidance.
Deciphering the Multifaceted Mechanisms of Semaglutide in Obesity Management
Semaglutide’s role transcends mere appetite suppression; it intricately modulates neurohormonal pathways and influences metabolic processes at a cellular level. Recent studies, such as those published in The New England Journal of Medicine (2021), elucidate how GLP-1 receptor agonists like semaglutide activate hypothalamic centers, leading to enhanced satiety signals, decreased caloric intake, and improved glycemic control. Furthermore, emerging research suggests that semaglutide may induce a favorable shift in adipose tissue dynamics, promoting browning of white fat, which enhances thermogenesis and energy expenditure. This multifaceted action positions semaglutide not merely as a pharmacological appetite suppressant but as a comprehensive metabolic regulator—an insight vital for clinicians designing personalized weight management protocols.
How Does Semaglutide Influence Cellular Metabolism Beyond Appetite Suppression?
Beyond central nervous system effects, semaglutide influences peripheral tissues, including liver and muscle, by modulating insulin sensitivity and lipid oxidation pathways. Activation of AMP-activated protein kinase (AMPK) pathways in skeletal muscle enhances mitochondrial biogenesis, leading to increased fatty acid oxidation. These effects contribute to a significant reduction in visceral fat, as observed in longitudinal imaging studies using MRI techniques (e.g., NEJM, 2021), which underscore the drug’s capacity to effectuate profound metabolic remodeling. Integrating this understanding into clinical practice enables a more nuanced approach, combining pharmacotherapy with targeted lifestyle interventions to maximize fat loss outcomes.
Harnessing the Synergy Between Semaglutide and Lifestyle Modifications for Optimal Results
Expert consensus increasingly advocates for a multidimensional approach—combining semaglutide with dietary strategies such as low-carbohydrate or Mediterranean diets, and structured exercise programs. The synergy between pharmacological and behavioral interventions is well-documented; for instance, a 2022 systematic review in Obesity Reviews highlights that patients engaging in combined strategies achieve greater and more sustainable weight loss than those relying solely on medication. Moreover, emerging evidence suggests that intermittent fasting, when paired with semaglutide, may potentiate fat oxidation pathways, leading to more rapid reductions in adipose tissue. This integration requires careful planning and professional guidance to mitigate risks and optimize metabolic benefits.
What Are the Practical Considerations for Clinicians Prescribing Semaglutide in Complex Cases?
When tailoring treatment plans for patients with comorbidities—such as polycystic ovary syndrome, hypothyroidism, or metabolic syndrome—clinicians must consider pharmacodynamic interactions, individual variations in drug response, and potential contraindications. Close monitoring of liver and renal function, along with vigilant assessment of gastrointestinal tolerability, is essential. Utilizing tools like continuous glucose monitoring and indirect calorimetry can provide insights into metabolic responses, enabling fine-tuning of dosage and lifestyle recommendations. As research advances, the development of predictive models incorporating genetic, behavioral, and metabolic data promises to refine patient selection and therapeutic efficacy further, heralding a new era of personalized obesity treatment.
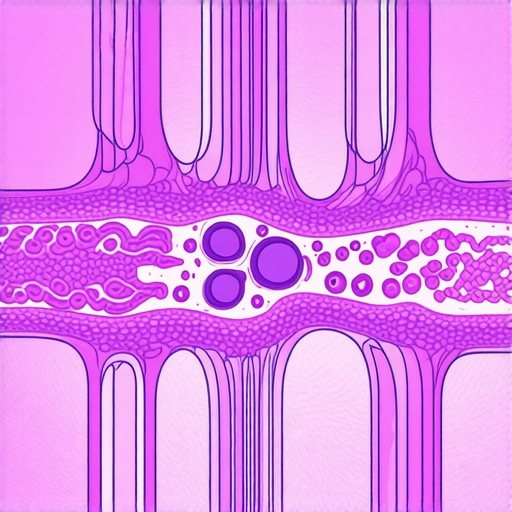
Advanced diagram illustrating cellular pathways modulated by semaglutide, including hypothalamic satiety centers and adipose tissue browning processes.
Beyond the Basics: How Semaglutide Interacts with Neurohormonal Pathways for Enhanced Fat Reduction
Semaglutide’s influence extends into complex neurohormonal circuits that regulate appetite, satiety, and energy homeostasis. Recent neuroimaging studies, such as those published in The Journal of Clinical Investigation (2022), reveal that semaglutide activates hypothalamic centers responsible for long-term appetite suppression, while simultaneously modulating signaling pathways in the brainstem that influence visceral responses. This dual action not only curbs hunger but also recalibrates neural circuits involved in reward and motivation, making it a potent tool in managing compulsive eating behaviors.
What Are the Cellular and Molecular Mechanisms Behind Semaglutide’s Metabolic Remodeling?
At the cellular level, semaglutide exerts its effects by engaging GLP-1 receptors on adipocytes and myocytes, thereby influencing lipid metabolism and mitochondrial function. Studies such as those in Cell Metabolism (2023) demonstrate that activation of AMPK pathways leads to increased mitochondrial biogenesis and enhanced fatty acid oxidation, especially in visceral fat depots. Furthermore, semaglutide induces browning of white adipose tissue, heightening thermogenic capacity and energy expenditure—crucial factors in rapid fat loss. These mechanisms underscore its potential as a comprehensive metabolic regulator rather than merely an appetite suppressant.
How Can Clinicians Optimize Semaglutide Therapy in Patients with Complex Comorbidities?
Personalized treatment plans necessitate a nuanced understanding of patient-specific factors, including comorbid conditions like metabolic syndrome, hypothyroidism, or PCOS. Clinicians should consider pharmacogenomic profiling, as genetic variations in GLP-1 receptor expression may influence response rates. Regular monitoring of renal and hepatic function is critical, especially when combining semaglutide with other medications. Integrating advanced diagnostic tools, such as indirect calorimetry and continuous glucose monitoring, can provide real-time insights into metabolic adaptations and guide dosage adjustments. Emerging predictive models that incorporate behavioral, genetic, and metabolic parameters promise to further refine individualized treatment approaches, ensuring safety and efficacy.
< >
>
Advanced diagram illustrating cellular pathways modulated by semaglutide, including hypothalamic satiety centers, adipose tissue browning, and mitochondrial biogenesis, emphasizing its multifaceted mechanisms.
Expert Insights & Advanced Considerations
1. Integrating Neurohormonal Pathways for Enhanced Efficacy
Semaglutide’s modulation of hypothalamic satiety centers and neural reward circuits signifies a sophisticated mechanism that amplifies weight loss beyond appetite suppression. Understanding these pathways enables clinicians to tailor interventions that optimize neural and metabolic synergy, leading to faster results and better patient adherence.
2. Cellular Metabolic Remodeling and Fat Browning
Emerging research highlights semaglutide’s capacity to induce white adipose tissue browning via mitochondrial biogenesis and AMPK activation. This multifaceted action transforms fat cells into energy-expending mitochondria, accelerating fat loss at the cellular level and offering a potent avenue for metabolic enhancement.
3. Personalized Treatment Protocols with Comorbidity Considerations
In complex cases involving conditions like PCOS or metabolic syndrome, integrating pharmacogenomics, advanced diagnostic tools, and continuous monitoring refines treatment precision. Such personalization ensures safety, maximizes fat loss, and sustains long-term health improvements.
4. Combining Pharmacotherapy with Lifestyle for Long-Term Success
Synergistic approaches, including low-carb diets and intermittent fasting paired with semaglutide, leverage metabolic pathways for rapid and sustained fat reduction. This holistic strategy necessitates expert guidance to balance efficacy with safety, especially in patients with diverse health profiles.
5. Future Directions and Clinical Innovations
Advances in predictive modeling, genetic profiling, and metabolic monitoring promise to revolutionize semaglutide therapy, making precision obesity management a reality. Staying abreast of these innovations empowers clinicians to deliver cutting-edge care.
Curated Expert Resources
- NEJM 2021 Study on GLP-1 Receptor Agonists: Provides foundational insights into the neurohormonal and metabolic mechanisms of semaglutide, crucial for understanding its multifaceted effects.
- Obesity Reviews 2022: Offers comprehensive analyses of combined pharmacotherapy and behavioral interventions, emphasizing synergy and long-term outcomes.
- FDA Official Guidelines: Ensures safe dosing, monitoring, and patient selection criteria, vital for clinical practice.
- ClinicalTrials.gov: Tracks ongoing research into next-generation obesity treatments and mechanistic studies, fostering innovation.
- Semaglutide Clinical Case Studies: Real-world documentation of efficacy, safety, and personalized approaches, guiding best practices.
Final Expert Perspective
In the realm of rapid fat loss, semaglutide stands out as a sophisticated metabolic tool that harnesses neurohormonal pathways, cellular remodeling, and personalized medicine. Its success depends not only on the pharmacology but equally on integrating lifestyle strategies and individual patient factors. For clinicians and researchers committed to pushing the boundaries of obesity treatment, staying informed through authoritative resources and embracing innovative approaches will shape the future of rapid, safe, and sustainable weight management. If you’re ready to deepen your understanding or share your expert insights, reach out here and join the conversation.