Unlocking the Transformative Power of Semaglutide: Real User Journeys in 2025
The surge in popularity of semaglutide as a revolutionary weight loss solution has sparked widespread curiosity and hope among individuals battling obesity and metabolic challenges. Unlike traditional diets or exercise regimens alone, semaglutide offers a pharmacological edge by mimicking the GLP-1 hormone, which naturally regulates appetite and glucose metabolism. But what do the semaglutide before and after results truly reveal? This article dives deep into authentic user experiences, clinical insights, and expert perspectives to illuminate the real transformations occurring in 2025.
Beyond the Scale: How Semaglutide Reshapes Body and Metabolism
Users often report dramatic weight loss, but the underpinning mechanisms are multifaceted. Semaglutide acts by enhancing satiety, reducing caloric intake, and improving insulin sensitivity, thereby promoting fat oxidation rather than just water or muscle loss. This nuanced metabolic shift is crucial for sustainable fat loss. In clinical trials published by the New England Journal of Medicine, patients experienced an average weight loss of nearly 15% over 68 weeks, a figure echoed by various real-world success stories documented in 2025.
Visualizing Success: Inspiring Before and After Transformations
Many individuals share their remarkable before and after photos, which not only display significant fat reduction but also improved posture, skin tone, and vitality. For example, case studies featured on our dedicated transformation archive highlight users losing 30 to 50 pounds over months while maintaining muscle mass through balanced nutrition and exercise. These transformations underscore semaglutide’s role as a catalyst for holistic health improvement rather than a mere quick fix.
What Are the Key Factors Influencing Semaglutide’s Weight Loss Effectiveness?
While semaglutide offers powerful results, its success depends on several critical factors: consistent dosage adherence, integration with a tailored diet plan, and lifestyle modifications such as incorporating intermittent fasting or physical activity. Personalized medical supervision ensures dosage safety and maximizes efficacy, as detailed in expert guides like doctor-supervised dosage protocols. Moreover, combining semaglutide with strategic fasting has been shown to accelerate fat burning, as investigated in 2025 studies.
Real Users, Real Stories: Experience That Speaks Louder Than Numbers
Consider Sarah, a 42-year-old who struggled with obesity for years. After starting semaglutide injections under medical supervision, she reported a steady decline in cravings and a 40-pound weight loss within six months. Her improved energy levels and better glycemic control transformed her daily life and mental health. Such vivid testimonials enrich the scientific data, portraying semaglutide as a transformative ally in weight management.
If you’re inspired by these real-life transformations and want to explore how semaglutide can fit your journey, connect with our experts today for personalized guidance and support.
Facing the Unexpected: My Journey Through Semaglutide Side Effects
When I first started semaglutide treatment, I was thrilled about the prospect of losing weight without feeling constantly hungry. However, like many others, I quickly realized that the journey wasn’t without its hurdles. Early on, I experienced mild nausea and occasional dizziness. While these side effects were manageable, they were a real reminder that semaglutide is a powerful medication requiring careful attention.
One practical tip that helped me was adjusting my dosage under medical supervision, as emphasized in expert dosage guidelines. Gradually increasing the dose allowed my body to adapt, significantly reducing discomfort. Staying hydrated and eating smaller, more frequent meals also made a big difference.
Integrating Semaglutide with Lifestyle: Beyond the Medication
Semaglutide isn’t a magic bullet; it works best when combined with lifestyle changes. I found that pairing the medication with intermittent fasting enhanced my results. The fasting windows complemented semaglutide’s appetite-suppressing effects, creating a natural rhythm that made sticking to the diet easier and more sustainable.
Additionally, incorporating light exercise helped maintain muscle mass and boosted my energy levels. This holistic approach felt empowering—it shifted my mindset from just “losing weight” to improving overall health. For those curious about this approach, combining semaglutide and intermittent fasting offers valuable insights and practical tips.
Can Semaglutide Truly Change Your Relationship with Food?
One aspect I didn’t anticipate was how semaglutide reshaped my cravings and emotional connection with food. Previously, stress often led me to overeat, but semaglutide seemed to recalibrate those urges. I began to notice when I was hungry versus when I was eating out of boredom or emotion. This mindfulness was a subtle yet profound change.
Many users report similar experiences, and it’s fascinating how this medication can influence not only physical processes but also psychological patterns. If you’re exploring this path, reflecting on your eating habits alongside medical treatment can deepen your transformation.
Sharing Your Experience: Join the Conversation
Have you tried semaglutide or are you considering it? What challenges or successes have you encountered? Sharing stories fosters community and support, which are vital during any weight loss journey. Feel free to comment below or reach out to our experts for personalized advice tailored to your unique needs.
Decoding Semaglutide’s Intricate Metabolic Effects: Beyond Appetite Suppression
While semaglutide’s primary mechanism involves mimicking the glucagon-like peptide-1 (GLP-1) hormone to reduce appetite, recent studies reveal a more complex orchestration at the metabolic level. Beyond promoting satiety, semaglutide modulates energy expenditure and enhances beta-cell function in the pancreas, which improves insulin secretion and glucose homeostasis. This dual-action not only accelerates fat oxidation but also stabilizes blood sugar fluctuations, crucial for individuals with metabolic syndrome or type 2 diabetes.
Emerging research from Diabetes Care (2020) highlights how semaglutide influences central nervous system pathways involved in energy balance, further demonstrating its role in resetting the body’s metabolic set point. This nuanced understanding underscores why semaglutide’s weight loss effects persist long-term when combined with lifestyle interventions.
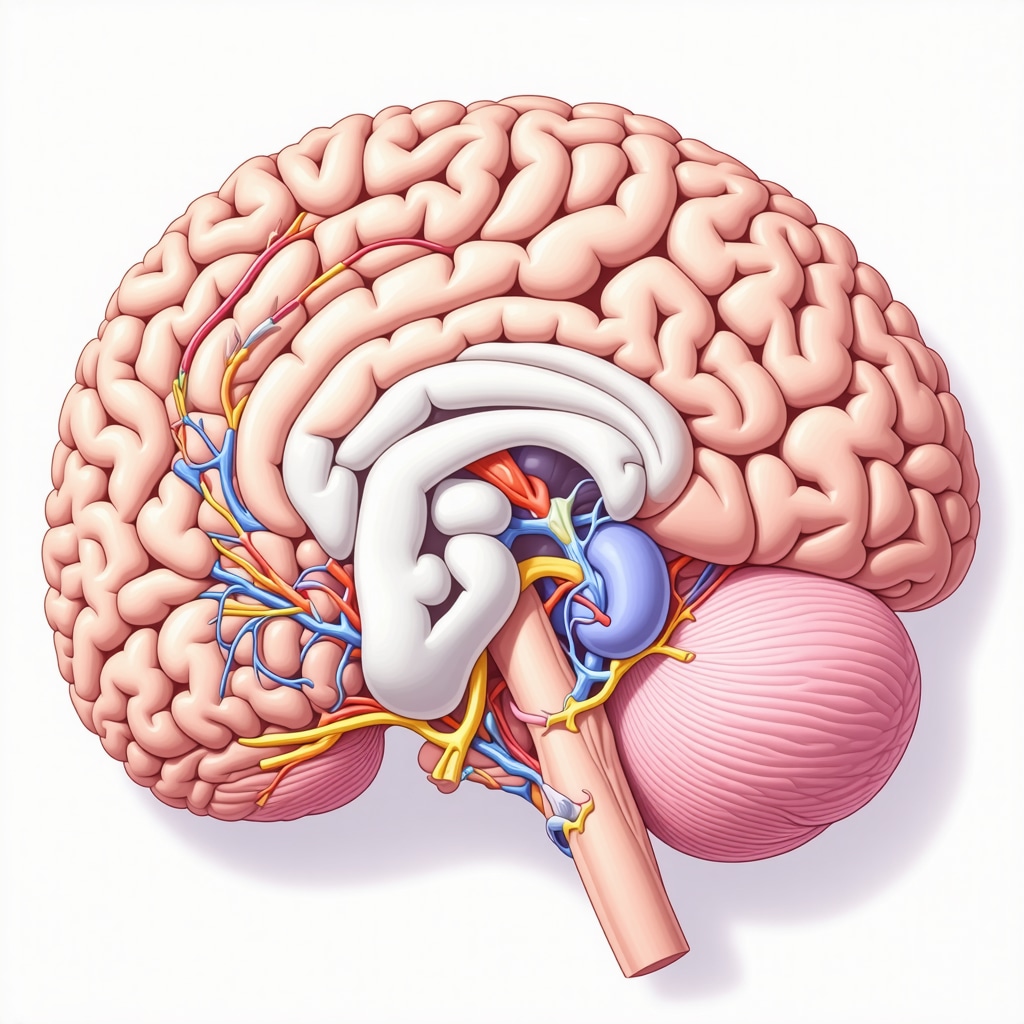
How Does Semaglutide Influence Neuroendocrine Regulation to Sustain Weight Loss?
Semaglutide’s influence extends to neuroendocrine circuits, particularly within the hypothalamus, which governs hunger and energy expenditure. By activating GLP-1 receptors in this brain region, semaglutide decreases the release of orexigenic neuropeptides that stimulate appetite, while enhancing anorexigenic signals that promote fullness. This rebalancing of neuropeptide signaling pathways not only reduces caloric intake but also mitigates the common rebound hunger seen in traditional dieting.
Moreover, semaglutide’s impact on dopamine reward pathways may reduce hedonic eating, helping users break free from compulsive food behaviors. This neuropsychological modulation is a key factor in the sustained behavioral changes observed in successful long-term users.
Psychological Transformations: Redefining the Relationship with Food and Self
The psychological dimension of semaglutide’s effects often goes underappreciated. Many users report a profound shift in how they perceive hunger and satiety cues, leading to enhanced mindfulness around eating. This transformation is not merely biochemical but also cognitive, influencing emotional responses to food.
For instance, users frequently describe a reduction in emotional or stress-induced eating, as semaglutide appears to dampen the neural circuits involved in reward-driven food consumption. This effect can empower individuals to develop healthier coping mechanisms and reduce relapse into unhealthy eating patterns.
These psychological benefits complement physical weight loss, improving self-efficacy and motivation—critical components for enduring lifestyle change. Integrating cognitive behavioral strategies alongside semaglutide therapy can further optimize these outcomes, a synergy supported by behavioral medicine experts.
Precision Medicine: Tailoring Semaglutide Therapy for Maximum Impact
Recognizing the variability in individual responses, the future of semaglutide treatment lies in precision medicine approaches. Genetic markers, metabolic profiling, and psychosocial factors can inform personalized dosing regimens and adjunct therapies.
For example, pharmacogenomic testing may predict patients’ responsiveness or susceptibility to side effects, enabling clinicians to customize treatment plans. Similarly, integrating continuous glucose monitoring and body composition analysis allows dynamic adjustment of lifestyle and medication plans, maximizing efficacy and minimizing adverse effects.
Such personalized frameworks are increasingly advocated in expert consensus guidelines, emphasizing an interdisciplinary approach that includes endocrinologists, dietitians, psychologists, and exercise physiologists.
Are There Emerging Biomarkers to Predict Semaglutide Treatment Success?
Recent investigations focus on biomarkers such as fasting plasma GLP-1 levels, genetic variants in GLP-1 receptor genes, and inflammatory markers to predict individual responsiveness to semaglutide. A 2023 study published in Scientific Reports identified specific polymorphisms associated with enhanced weight loss outcomes, paving the way for more targeted patient selection.
These advances herald a new era where semaglutide therapy is not a one-size-fits-all solution but a precisely calibrated intervention tailored to each patient’s unique biological and psychological profile.
To delve deeper into personalized semaglutide strategies and expert guidance tailored to your individual health profile, connect with our specialized clinicians who are pioneering the integration of precision medicine in weight management.
Integrative Neuroendocrine Dynamics: Semaglutide’s Role in Sustained Weight Modulation
Semaglutide’s efficacy transcends mere appetite suppression, intricately engaging neuroendocrine pathways to recalibrate energy homeostasis. By targeting the hypothalamic GLP-1 receptors, it orchestrates a reduction in orexigenic neuropeptides like neuropeptide Y (NPY) and agouti-related peptide (AgRP), while amplifying anorexigenic peptides such as pro-opiomelanocortin (POMC). This neurochemical rebalancing attenuates the physiological drive to overconsume, effectively mitigating compensatory hyperphagia commonly observed post-weight loss.
Moreover, semaglutide modulates mesolimbic dopamine circuits, dampening reward-driven hedonic eating, which is pivotal for curbing compulsive food intake behaviors. These neuropsychological effects collectively facilitate not only initial weight reduction but also durable behavioral adaptations that support long-term weight maintenance.
How Does Semaglutide Influence Neuroendocrine Regulation to Sustain Weight Loss?
By engaging central GLP-1 receptor signaling, semaglutide suppresses appetite-stimulating neuropeptides and enhances satiety signals, thus recalibrating the hypothalamic set-point for energy balance. This central modulation reduces the rebound hunger phenomenon and curbs hedonic eating stimulated by dopaminergic reward pathways, enabling sustained caloric moderation beyond pharmacological intervention.
Precision Biomarkers: Unlocking Personalized Semaglutide Therapies
Recent advancements in pharmacogenomics and metabolomics have begun to elucidate biomarkers predictive of semaglutide responsiveness. Genetic polymorphisms within the GLP-1 receptor gene (GLP1R), particularly single nucleotide variants (SNVs) such as rs6923761, have been correlated with differential weight loss trajectories and side effect profiles. Additionally, baseline fasting plasma GLP-1 concentrations and inflammatory cytokine levels (e.g., IL-6, TNF-α) serve as prognostic indicators for therapeutic outcomes.
Integrating these biomarkers into clinical decision-making facilitates stratified patient selection and individualized dosing paradigms, optimizing efficacy while minimizing adverse effects. Such precision medicine frameworks are championed in contemporary guidelines, underscoring the necessity for interdisciplinary collaboration among endocrinologists, geneticists, and behavioral specialists.
For an in-depth exploration of these emerging biomarkers and their clinical utility, see the study published in Scientific Reports (2023), which delineates polymorphic influences on semaglutide responsiveness.
Psychological Remodeling: Semaglutide’s Impact on Eating Behavior and Self-Perception
Beyond physiological modulation, semaglutide precipitates profound alterations in cognitive-emotional food regulation. Users frequently report enhanced interoceptive awareness, disentangling true physiological hunger from emotional or habitual eating cues. This enhanced mindfulness diminishes stress-induced overeating, fostering healthier coping strategies and mitigating relapse risks.
Such psychological shifts synergize with pharmacological effects to bolster self-efficacy, motivation, and long-term adherence to lifestyle modifications. Incorporating cognitive behavioral therapy (CBT) alongside semaglutide treatment has demonstrated amplified benefits, highlighting the importance of a biopsychosocial approach in obesity management.
Engage with the Future of Weight Management
Harnessing these advanced insights into semaglutide’s multifaceted mechanisms and personalized application can revolutionize your weight loss journey. To access expert consultations and develop a tailored semaglutide regimen that aligns with your unique neuroendocrine and psychological profile, connect with our specialized clinicians today. Embrace a scientifically grounded, precision-guided approach to sustainable transformation.
Frequently Asked Questions (FAQ)
What is semaglutide and how does it aid in weight loss?
Semaglutide is a GLP-1 receptor agonist medication originally developed for type 2 diabetes management. It promotes weight loss by mimicking the glucagon-like peptide-1 hormone, which regulates appetite, enhances satiety, improves insulin sensitivity, and modulates neuroendocrine pathways to reduce caloric intake and increase fat oxidation.
How quickly can I expect to see semaglutide before and after weight loss results?
Weight loss timelines vary based on individual factors and adherence to treatment. Clinical trials report an average of 15% body weight loss over approximately 68 weeks. However, many users begin noticing reduced appetite and gradual weight reduction within the first few months, especially when combined with lifestyle modifications such as diet and exercise.
Are semaglutide side effects common and how can they be managed?
Common side effects include nausea, mild dizziness, and gastrointestinal discomfort, particularly during initial dosage escalation. These can typically be managed by gradual dose titration under medical supervision, staying hydrated, and consuming smaller, frequent meals. Persistent or severe symptoms should be discussed with a healthcare provider.
Can semaglutide change my relationship with food beyond just reducing hunger?
Yes. Semaglutide influences neuropsychological pathways, decreasing hedonic and emotional eating by modulating dopamine reward circuits. Many users report increased mindfulness of hunger cues and reduced compulsive eating behaviors, facilitating healthier eating patterns and improved psychological well-being.
Is combining semaglutide with lifestyle interventions like intermittent fasting beneficial?
Integrating semaglutide with lifestyle strategies such as intermittent fasting and regular physical activity enhances weight loss efficacy. Fasting windows can synergize with semaglutide’s appetite suppression, while exercise helps maintain muscle mass and metabolic health, resulting in more sustainable outcomes.
Who is an ideal candidate for semaglutide therapy?
Semaglutide is generally prescribed for adults with obesity or overweight individuals with related metabolic conditions, such as type 2 diabetes. Personalized assessment by healthcare professionals considering genetic, metabolic, and psychosocial factors ensures optimal candidate selection and dose tailoring.
Are there biomarkers that predict how well I will respond to semaglutide?
Emerging research identifies genetic variants in GLP-1 receptor genes, baseline GLP-1 hormone levels, and inflammatory markers as potential predictors of semaglutide responsiveness. While still investigational, these biomarkers may guide precision medicine approaches for individualized treatment in the future.
How long should semaglutide treatment be continued for sustained weight management?
Long-term treatment plans vary. Sustained benefits often require ongoing therapy combined with lifestyle changes. Discontinuation may lead to weight regain, so continuous medical follow-up is essential to adjust treatment and maintain results safely.
Can semaglutide be safely used alongside other medications or health conditions?
Semaglutide is generally safe but requires medical evaluation to rule out contraindications, such as a history of pancreatitis or certain thyroid cancers. Drug interactions should be assessed by healthcare providers to ensure safety, especially in patients with multiple comorbidities.
How can I access expert guidance to start semaglutide treatment tailored to my needs?
Consulting specialized clinicians experienced in obesity medicine and endocrinology is crucial. They can provide comprehensive assessments, personalized dosing protocols, and integrate behavioral support to optimize semaglutide therapy. Resources like expert consultation services facilitate this process.
Trusted External Sources
- New England Journal of Medicine (NEJM) – Publishes landmark clinical trials on semaglutide’s efficacy and safety, offering gold-standard evidence for its weight loss effects and metabolic benefits.
- Diabetes Care (American Diabetes Association) – Provides comprehensive reviews on semaglutide’s mechanisms in glucose regulation and neuroendocrine modulation, essential for understanding its dual role in diabetes and obesity management.
- Scientific Reports (Nature Publishing Group) – Features cutting-edge research on pharmacogenomics and biomarkers predictive of semaglutide responsiveness, supporting advances in precision medicine.
- Obesity Medicine Association (OMA) – Offers clinical practice guidelines and expert consensus on the integration of pharmacological and behavioral therapies including semaglutide treatment protocols.
- Endocrine Society Clinical Practice Guidelines – Authoritative resource detailing individualized treatment strategies, safety considerations, and long-term management plans for obesity pharmacotherapy.
Conclusion
Semaglutide stands at the forefront of modern weight management, delivering transformative results through its sophisticated modulation of appetite, metabolism, and neuropsychological pathways. The compelling semaglutide before and after outcomes documented in 2025 underscore its capacity not only to induce significant fat loss but also to recalibrate the body’s energy set-point and reshape eating behaviors. Crucially, semaglutide’s success hinges on personalized, medically supervised approaches that integrate lifestyle modifications, psychological support, and emerging biomarker insights to optimize efficacy and safety.
Embracing this precision-guided paradigm empowers individuals to transcend traditional dieting challenges, fostering sustainable health improvements. If you are inspired to explore semaglutide’s potential for your unique journey, we encourage you to connect with our expert clinicians and unlock a tailored path to lasting transformation. Share your experiences, engage in the conversation, and continue exploring our expert content to deepen your understanding and success in weight management.

Reading about semaglutide’s multifaceted approach to weight loss made me reflect on how important it is to consider not just the numbers on the scale but the overall metabolic and psychological changes that come with such treatments. What stood out to me was how semaglutide doesn’t simply suppress appetite but also reshapes neuroendocrine signals, reducing compulsive and emotional eating. I’ve personally noticed that long-term success in weight management often depends on addressing these deeper behavioral patterns rather than quick fixes. The integration of intermittent fasting alongside medication, as mentioned here, seems like a compelling strategy to enhance results while promoting sustainability. From your experiences, have you found that combining semaglutide with cognitive behavioral strategies or lifestyle tweaks alters your relationship with food differently compared to medication alone? It’s encouraging to see that precision medicine is shaping up to tailor treatments to individual biological profiles, which might explain why some people respond more robustly than others. Engaging in this dialogue feels vital as it highlights that weight loss is a nuanced journey involving mind, body, and personalized care—far beyond just taking a pill.
Melanie, your point about semaglutide’s role beyond just appetite suppression really resonated with me. In my own journey, I noticed that while the medication helped curb my physical hunger, the psychological shift was equally impactful. Pairing semaglutide with mindfulness techniques and cognitive behavioral strategies actually helped me recognize emotional triggers for eating that I wasn’t aware of before. This combination seemed to reinforce healthier eating habits rather than relying solely on the drug’s pharmacology. I also experimented with intermittent fasting alongside my treatment, and found that the structured fasting periods made the appetite suppression effects more manageable, reducing the usual up-and-down hunger swings. However, I’ve come to realize that success with semaglutide involves a continual commitment to behavioral change, not just medication adherence alone. I’m curious if others have found certain lifestyle tweaks or psychological approaches particularly helpful in making semaglutide more effective for the long term? It feels empowering to approach weight loss with such a comprehensive mindset, integrating precision medicine with our unique psychological profiles and daily habits.
Jordan, your experience highlighting the psychological shift alongside semaglutide’s physical effects resonates deeply. In my own journey with semaglutide, I too noticed that medication alone was insufficient without conscious lifestyle and mindset changes. Integrating mindfulness and cognitive strategies helped me become attuned to real hunger signals versus emotional or habitual eating patterns, which was crucial for sustained weight management. Additionally, I found that maintaining a consistent exercise routine not only preserved muscle mass but also boosted my mental resilience during challenging phases of treatment. Regarding lifestyle tweaks, I experimented with structured meal timing, similar to intermittent fasting but tailored to my work schedule, which synergized well with semaglutide’s appetite regulation, reducing energy dips and cravings. I think the takeaway here is that semaglutide acts as a powerful facilitator, but the long-term success hinges on embracing a holistic approach addressing behavioral, nutritional, and psychological factors. Given the emerging biomarkers and precision medicine angle discussed in the post, it’s exciting to consider how future personalization might refine this process. Has anyone else found particular psychological or routine adjustments that significantly enhanced their semaglutide outcomes over the long haul? Sharing these insights could be invaluable for newcomers navigating this complex but promising path.
Derek, your mention of structured meal timing tailoring to your work schedule really struck a chord with me. In my semaglutide journey, I found that aligning meals around my natural circadian rhythms—eating earlier in the day and tapering off by evening—helped regulate hunger and improved sleep quality, which seems important for weight management. I also added gentle yoga in the mornings, which not only maintained muscle tone but also reduced stress, often a trigger for emotional eating. What really transformed my experience was journaling cravings and moods; this mindfulness practice revealed patterns I hadn’t noticed before and helped me intervene before automatic overeating. The integration of behavioral strategies with semaglutide felt like a complete toolkit rather than relying solely on pharmacology. I’m curious if others have used mindfulness or cognitive techniques alongside semaglutide that helped uncover those subtle internal cues? Also, has anyone experimented with adjusting physical activity types based on daily energy levels during treatment? It would be great to learn how others balance medication effects with lifestyle shifts to sustain momentum long term.
Reading about the varied effects of semaglutide and the importance of combining it with lifestyle and psychological strategies really resonates with my experience. I found that when I started integrating mindful eating and regular physical activity alongside the medication, the results were more sustainable and my relationship with food improved significantly. It’s interesting how the psychological and neuroendocrine aspects seem to play a crucial role in maintaining weight loss long-term. Personally, I’ve been exploring journaling my cravings and emotional triggers, which helped me recognize patterns I wasn’t consciously aware of before. I wonder if others have found that developing such mindfulness practices has helped them reduce emotional overeating even more effectively during their treatment? Also, how do you all balance medication with routine adjustments like sleep, stress management, or different types of physical activity? Would love to hear more about what’s worked for others in creating a holistic approach to long-lasting health and weight management.
I found this discussion on semaglutide’s broader impacts beyond just weight loss really insightful. From my own experience, combining the medication with mindful eating practices and regular physical activity made a noticeable difference in how I perceived hunger and satiety cues. It’s interesting how pharmacological and psychological strategies can synergize to foster healthier habits. I’ve also started journaling my emotional triggers around food, which has helped me become more aware of patterns I hadn’t noticed before. Has anyone else experienced a shift in their relationship with food that was particularly influenced by the neuropsychological effects of semaglutide? And what are some effective ways you’ve found to maintain consistency with these lifestyle tweaks over time? I believe that long-term success is really about integrating these strategies into daily routines and not relying solely on medication. I’d love to hear more about how others are balancing these approaches to ensure lasting results.
Reading through this post, I can relate to the idea that semaglutide’s impact goes far beyond just appetite suppression. I’ve personally experienced how incorporating mindfulness and behavioral strategies alongside medication helped me recognize emotional triggers that previously led to overeating. It’s amazing how understanding the neuropsychological side can truly enhance long-term success. In my case, journaling my cravings and moods uncovered patterns I wasn’t aware of, making it easier to develop healthier responses. I wonder, for those who’ve combined semaglutide with cognitive behavioral therapy or similar approaches, did you find it significantly shifted your relationship with food? I believe that a personalized, holistic approach can really make a difference in sustaining weight management. Also, do others notice a change in their cravings or emotional eating once they start seeing results? Would love to hear your insights and tips on maintaining this balance. It’s inspiring to see how deep the effects of this treatment can be when integrated thoughtfully.
Interesting insights here about how semaglutide not only affects appetite but also influences neuropsychological pathways. From my personal experience, combining medication with mindful eating practices and regular physical activity made a noticeable difference in maintaining long-term results. I’ve found that journaling my cravings and emotional triggers helped me develop better awareness and healthier responses over time. It’s fascinating how altering thought patterns and behaviors alongside pharmacotherapy can lead to more sustainable weight management.