Unlocking the Secrets to Safe Semaglutide Injection Practices
Semaglutide injections have revolutionized weight management by offering a powerful, clinically approved option to support fat loss. However, the journey to effective and safe use demands more than simply administering the drug. Understanding the nuances of dosage, timing, and potential side effects is paramount for anyone considering this treatment. Drawing on clinical experience and evidence-based guidelines, this article dives deep into the safe usage and dosage parameters that maximize benefits while minimizing risks.
Decoding Semaglutide Dosage: Finding the Perfect Balance
One of the most critical factors in semaglutide therapy is dosage optimization. Starting doses typically begin at 0.25 mg once weekly, not for weight loss effect but to ease the body into the medication and reduce gastrointestinal side effects. Then, the dose is gradually increased every 4 weeks, commonly reaching 1 mg/week, with some patients requiring up to 2.4 mg/week for optimal results under strict medical supervision. This titration strategy exemplifies a precision approach to balancing efficacy and tolerability, as endorsed by leading endocrinology guidelines and clinical trials.
Experts emphasize never exceeding prescribed limits without physician oversight, as excessive doses can elevate risks such as pancreatitis or thyroid C-cell tumors. Understanding this balance ensures that patients reap maximum fat-burning benefits without compromising safety.
Mastering Injection Technique: The Art Behind Effective Administration
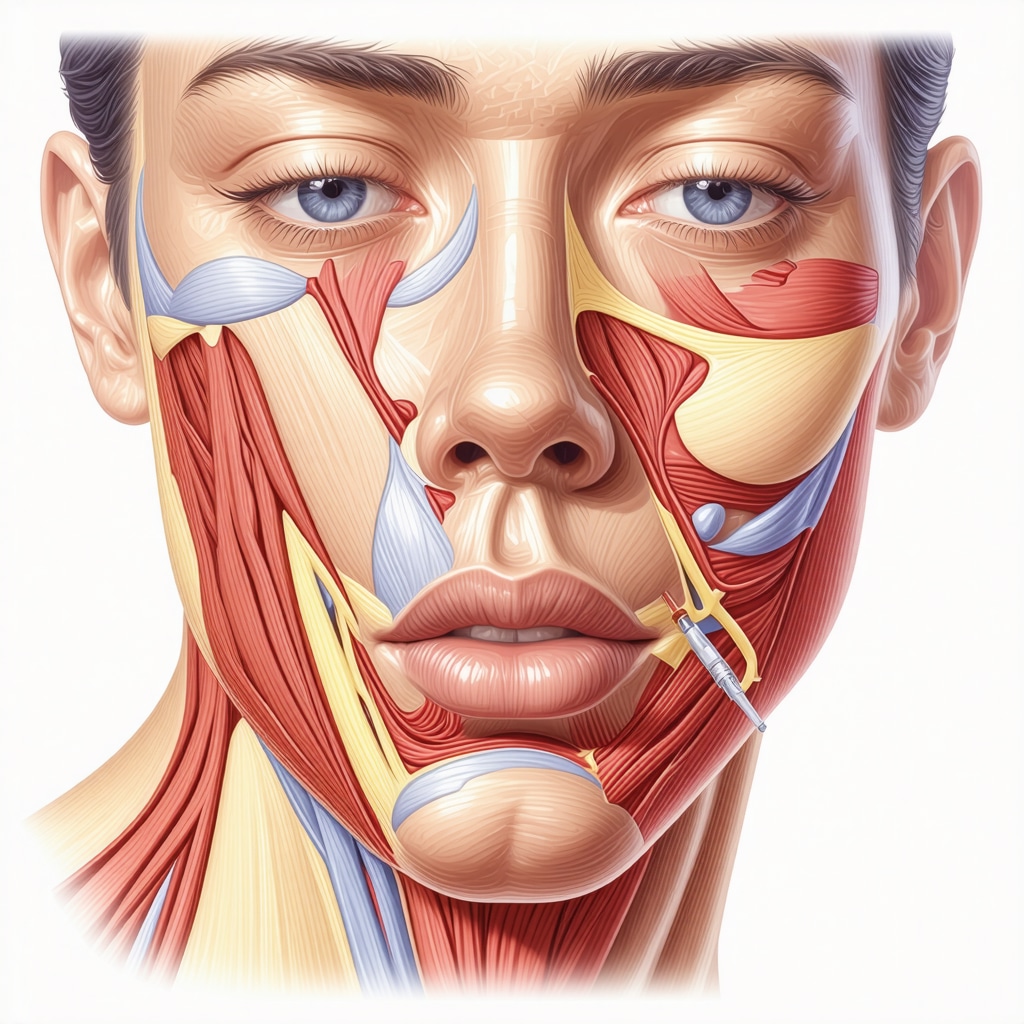
Proper injection technique is often underestimated yet is vital in safe semaglutide use. The subcutaneous injection should be administered into the abdomen, thigh, or upper arm, rotating sites weekly to prevent lipodystrophy. Using a new needle for each injection and following sterile protocols minimize infection risks. Patients are advised to avoid injecting into irritated or scarred skin.
How Can Patients Manage Side Effects While Maintaining Safe Dosage?
Common side effects include nausea, vomiting, and mild gastrointestinal discomfort, especially during dose escalation. These often subside as the body adjusts. Managing these symptoms involves adhering to the titration schedule, eating smaller meals, and staying hydrated. In rare cases, severe adverse reactions require discontinuation. Close communication with healthcare providers allows for timely adjustments and reassurance.
Integrating Semaglutide Into a Holistic Weight Loss Strategy
While semaglutide injections are a potent tool, their safety and efficacy are optimized when combined with lifestyle modifications such as balanced nutrition and regular exercise. Emerging evidence suggests synergistic benefits when semaglutide treatment is paired with intermittent fasting protocols for enhanced fat burn and metabolic health (learn more here).
Patients should always seek doctor-supervised programs to ensure comprehensive monitoring and personalized dose adjustments, as outlined in expert guidelines (doctor supervised semaglutide safe dosage guidelines).
For authoritative information on dosage and safety, the FDA Drug Safety Communication provides detailed insights on risks and monitoring.
Have you experienced semaglutide treatment or have questions about the best practices? Reach out to medical experts or share your story to enrich the community knowledge.
Listening to Your Body: Personal Reflections on Semaglutide Side Effects
When I first started semaglutide treatment, the nausea caught me off guard. It wasn’t debilitating, but enough to make me cautious about meal timing and portion sizes. I discovered that eating smaller, more frequent meals helped tremendously. Plus, staying well-hydrated became a daily ritual. Gradually, as my dose increased, my body adapted, and the side effects lessened significantly. I found that patience and close communication with my healthcare provider were key to navigating these early challenges.
In fact, a study published in The New England Journal of Medicine highlights how gradual dose escalation minimizes gastrointestinal symptoms, allowing patients to continue treatment comfortably over time. This aligns with my experience and underscores why following a medically supervised titration schedule is essential.
Why Rotating Injection Sites Changed My Semaglutide Experience
Initially, I didn’t pay much attention to where I injected the medication. Soon, I noticed some redness and mild tenderness at the injection sites. Learning about lipodystrophy—the localized loss or accumulation of fat tissue from repeated injections in the same spot—was eye-opening. Since then, I’ve made it a point to rotate between my abdomen, thighs, and upper arms weekly. This simple habit not only reduced skin irritation but also made the injections more comfortable and my treatment more sustainable.
Could Combining Lifestyle Changes with Semaglutide Be the Ultimate Game Changer?
This question has been on my mind throughout my journey. Semaglutide is powerful, no doubt, but pairing it with balanced nutrition and consistent exercise has amplified my results. Integrating intermittent fasting was another game changer for me—I noticed enhanced fat burning and improved energy levels. If you’re curious about how to combine semaglutide and intermittent fasting safely, there’s a wealth of practical tips and clinical insights available that I found invaluable (explore the strategic duo here).
Practical Tips That Made a Difference in My Semaglutide Journey
- Stick to your prescribed dosage and titration schedule: This minimizes side effects and maximizes fat loss.
- Rotate injection sites weekly: Protect your skin and ensure better absorption.
- Eat mindfully: Smaller meals, hydration, and nutrient-rich foods help your body adjust and support weight loss.
- Communicate openly with your healthcare provider: Adjustments might be needed to tailor treatment to your unique needs.
For those interested in a comprehensive, doctor-supervised approach, I recommend looking into medical programs that specialize in semaglutide treatment. These programs offer personalized dosing, monitoring, and lifestyle coaching that can significantly improve your experience and outcomes (learn more about medical weight loss programs with semaglutide).
Have you started semaglutide treatment or are considering it? What challenges or successes have you experienced? Feel free to share your story or ask questions. Your insights can help others navigating this journey.
Precision Injection Site Rotation: Minimizing Localized Tissue Complications in Semaglutide Therapy
The clinical importance of rotating injection sites transcends mere skin comfort; it is a critical factor in preserving subcutaneous tissue integrity and optimizing drug absorption kinetics. Repeated semaglutide injections at the same anatomical location can lead to lipohypertrophy or lipoatrophy, which not only cause cosmetic concerns but also impair insulin and drug uptake, diminishing therapeutic efficacy.
Recent histopathological studies have demonstrated that lipohypertrophy results from adipocyte hypertrophy and fibrotic changes triggered by chronic local exposure to GLP-1 receptor agonists. Therefore, a systematic rotation protocol—alternating between the abdomen, lateral thighs, and upper arms on a weekly basis—is recommended. This approach mitigates inflammatory responses and supports consistent pharmacodynamics.
What Are the Best Practices for Injection Site Rotation to Prevent Lipodystrophy?
Experts advise mapping out injection zones within each site, ensuring injections are spaced at least 1 inch apart. Utilizing injection diaries or mobile apps can assist patients in maintaining an effective rotation schedule. Additionally, proper needle length and angle (typically 90 degrees for subcutaneous injections) are essential to avoid intramuscular administration, which can alter absorption rates and increase discomfort.
Training patients on correct injection technique, including site inspection prior to administration, empowers them to identify early signs of tissue changes and seek medical advice promptly. This proactive strategy enhances long-term treatment adherence and outcomes.
Individualized Dosage Titration Protocols: Leveraging Pharmacogenomics and Clinical Monitoring
While the standardized titration schedule serves as a foundational guideline, emerging research is illuminating the role of pharmacogenomic factors in semaglutide metabolism and patient response variability. Polymorphisms in genes encoding GLP-1 receptors and downstream signaling pathways may influence both efficacy and side effect profiles.
In clinical practice, integrating pharmacogenomic testing with traditional monitoring—such as glycemic markers, weight trajectory, and adverse event reporting—enables truly personalized dosage adjustments. For example, patients exhibiting heightened gastrointestinal sensitivity might benefit from a slower titration pace or adjunctive therapies to mitigate nausea.
Moreover, a multidisciplinary team approach involving endocrinologists, dietitians, and pharmacologists can optimize therapeutic regimens. Such collaboration ensures dosage escalation aligns with metabolic improvements while minimizing risks.
Exploring the Intersection of Semaglutide and Gut Microbiota: Implications for Side Effect Management and Weight Loss Efficiency
Cutting-edge studies have begun to explore how semaglutide’s modulation of appetite and glucose metabolism might interact with the gut microbiome composition. Alterations in microbial diversity and short-chain fatty acid production could partly explain variability in gastrointestinal side effects and weight loss success.
Interventions such as prebiotic supplementation and dietary modifications targeting microbiota balance are under investigation as adjuncts to semaglutide therapy. These strategies may enhance tolerability and potentiate metabolic benefits, representing a frontier of personalized medicine in obesity treatment (Suez et al., 2020, Nature Communications).
Understanding these complex interactions requires ongoing research but offers promising avenues to refine semaglutide protocols beyond conventional paradigms.
Next Steps in Expert-Guided Semaglutide Use: Continuous Monitoring and Adaptive Treatment Models
Given the multifaceted nature of semaglutide therapy, embracing continuous glucose monitoring (CGM) and digital health tools can provide real-time feedback on metabolic responses. This data-driven approach facilitates dynamic dose adjustments and early identification of adverse effects.
Clinicians are encouraged to integrate patient-reported outcomes with biometric data, fostering shared decision-making that enhances adherence and satisfaction. As semaglutide use expands, developing robust registries and leveraging artificial intelligence for predictive analytics will further personalize treatment.
If you’re navigating semaglutide therapy or considering its initiation, consulting with specialists who utilize these advanced monitoring techniques can significantly elevate your treatment experience. Connect with our expert medical team to explore personalized dosage strategies and comprehensive support tailored to your unique metabolic profile.
Harnessing Precision Medicine: Tailoring Semaglutide Therapy Beyond Standard Protocols
In the evolving landscape of GLP-1 receptor agonist therapies, semaglutide stands out not only for its efficacy but also for the necessity of individualized treatment paradigms. Moving beyond one-size-fits-all dosing, clinicians increasingly leverage pharmacogenomic insights and patient-specific metabolic markers to refine titration schedules, thus enhancing both safety and therapeutic impact. Such precision medicine approaches are revolutionizing how semaglutide is integrated into personalized obesity management plans.
Decoding Injection Site Microenvironment: Implications for Absorption and Patient Comfort
The microenvironment of injection sites—comprising local blood flow, adipose tissue characteristics, and inflammatory status—significantly influences semaglutide bioavailability. Emerging evidence highlights that subtle differences in subcutaneous tissue can alter drug pharmacokinetics. Expert practitioners recommend not only rotating injection sites but also assessing tissue quality and avoiding areas with compromised circulation or fibrosis to optimize drug uptake and minimize discomfort.
How Can Advanced Monitoring Improve Semaglutide Dose Adjustments and Side Effect Management?
Advanced monitoring tools such as continuous glucose monitors (CGM) and digital patient-reported outcome platforms empower clinicians to dynamically adjust semaglutide dosing. Real-time glycemic trends and symptom tracking facilitate early detection of adverse effects and allow for rapid, data-driven titration modifications. This proactive strategy enhances adherence and mitigates risks, particularly in patients with complex metabolic profiles or comorbid conditions.
Integrating Cutting-Edge Research: Gut Microbiome Modulation as a Semaglutide Adjunct
Recent studies illuminate the bidirectional relationship between semaglutide therapy and gut microbiota composition. Modulating microbial diversity through targeted prebiotics or dietary interventions shows promise in reducing gastrointestinal side effects and potentiating weight loss efficacy. These findings herald a new frontier where microbiome-centric adjunct therapies complement pharmacological treatment, tailoring semaglutide regimens to individual microbial signatures (Suez et al., 2020, Nature Communications).
Implementing Digital Health Solutions: The Future of Personalized Semaglutide Therapy
Digital health innovations, including mobile injection trackers and AI-driven dose optimization algorithms, are transforming semaglutide administration. These tools facilitate precise injection site rotation, adherence monitoring, and personalized dose escalation, ensuring patients experience maximal benefit with minimal side effects. Such integrative platforms enable a collaborative treatment model between patients and healthcare providers, fostering sustained engagement and improved outcomes.
For clinicians and patients seeking a sophisticated, evidence-based approach to semaglutide therapy, embracing these advanced methodologies is indispensable. Engage with our expert team today to explore tailored dosing strategies and innovative support systems designed to elevate your treatment journey.
Frequently Asked Questions (FAQ)
What is the recommended starting dose of semaglutide for weight management?
The typical initiation dose of semaglutide is 0.25 mg once weekly. This low dose is primarily to mitigate gastrointestinal side effects and acclimate the body, not for immediate weight loss. Dosage is gradually increased every 4 weeks under medical supervision to reach an effective therapeutic dose, often 1 mg weekly or higher depending on individual response.
How important is rotating injection sites during semaglutide therapy?
Rotating injection sites is essential to prevent lipodystrophy, which includes localized fat tissue changes like lipohypertrophy or lipoatrophy. These can impair drug absorption and cause discomfort. Experts recommend rotating among the abdomen, thighs, and upper arms weekly, spacing injections at least 1 inch apart within each site to maintain tissue health and consistent drug uptake.
Can semaglutide be safely combined with intermittent fasting?
Emerging evidence supports combining semaglutide with intermittent fasting as a strategic approach to enhance fat burning and metabolic health. However, this should be done under professional guidance to ensure safety, avoid hypoglycemia, and tailor dosing schedules appropriately. Clinical monitoring is key to optimizing this combination.
What are common side effects and how can they be managed?
Common side effects include nausea, vomiting, and mild gastrointestinal discomfort, predominantly during dose escalation. Management strategies include adhering to prescribed titration schedules, consuming smaller, frequent meals, staying hydrated, and communicating with healthcare providers for dose adjustments or supportive therapies.
How does pharmacogenomics influence semaglutide dosing?
Pharmacogenomic variations in GLP-1 receptor genes and related pathways can affect individual responses to semaglutide, influencing efficacy and side effect profiles. Incorporating genetic testing alongside clinical monitoring enables personalized dose titration, optimizing therapeutic outcomes and minimizing adverse events.
What role does the gut microbiome play in semaglutide therapy?
Semaglutide may modulate gut microbiota composition, affecting appetite regulation and metabolic responses. Adjusting the microbiome through prebiotic supplementation or dietary changes could potentially reduce gastrointestinal side effects and improve weight loss efficacy, representing an area of ongoing research and personalized treatment innovation.
Are there digital tools to assist with semaglutide therapy management?
Yes, mobile apps and digital platforms can track injection sites, monitor adherence, and support personalized dose adjustments. Advanced tools like continuous glucose monitors provide real-time metabolic data, enabling clinicians and patients to optimize therapy dynamically and improve safety and effectiveness.
What should patients do if they experience severe side effects?
Severe adverse reactions such as persistent vomiting, signs of pancreatitis, or allergic reactions require immediate medical attention. Patients should promptly notify their healthcare provider to evaluate the need for dose modification or discontinuation and receive appropriate care.
How can patients ensure long-term success with semaglutide treatment?
Success relies on following prescribed dosing schedules, rotating injection sites, integrating lifestyle modifications including nutrition and exercise, maintaining open communication with healthcare teams, and utilizing advanced monitoring tools when available to tailor therapy effectively.
Is semaglutide therapy suitable for everyone?
Semaglutide is not appropriate for individuals with a history of medullary thyroid carcinoma, multiple endocrine neoplasia syndrome type 2, or certain other conditions. A thorough medical evaluation by an endocrinologist or specialist is necessary to determine suitability and customize treatment plans.
Trusted External Sources
- U.S. Food and Drug Administration (FDA) Drug Safety Communication: Provides authoritative safety warnings, risk assessments, and official prescribing information for semaglutide, critical for understanding regulatory guidelines and monitoring requirements.
- The New England Journal of Medicine (NEJM): Publishes pivotal clinical trials and mechanistic studies on semaglutide’s efficacy, dosing protocols, and side effect profiles, offering cutting-edge evidence for clinical practice.
- American Diabetes Association (ADA) Standards of Medical Care: Offers expert consensus on GLP-1 receptor agonist use including semaglutide, with recommendations on dosage titration, patient selection, and integration with lifestyle interventions.
- Nature Communications – Microbiome Research (Suez et al., 2020): Explores the interaction between GLP-1 therapies and gut microbiota, providing insight into adjunctive treatments and personalized medicine approaches.
- Endocrinology and Metabolism Clinics of North America: Features comprehensive reviews on injection site management, pharmacogenomics, and evolving monitoring technologies relevant to semaglutide therapy.
Conclusion
Semaglutide injections represent a transformative advancement in weight management, offering potent efficacy when used with precision and care. Safely maximizing its benefits hinges on individualized dosage titration, meticulous injection site rotation, and proactive side effect management. Integrating semaglutide into a holistic strategy that includes lifestyle modifications and emerging adjuncts like intermittent fasting and microbiome support further amplifies outcomes. Cutting-edge digital health tools and pharmacogenomic insights are paving the way toward truly personalized semaglutide therapy, enhancing both safety and effectiveness. Patients and clinicians alike should embrace these expert-informed practices and innovations to unlock semaglutide’s full potential in combating obesity. Engage with healthcare professionals, share experiences, and explore related expert content to deepen your understanding and success with semaglutide treatment.


This post really highlights how critical it is to approach semaglutide therapy with a personalized mindset, especially around dosage titration and injection technique. From what I’ve seen in my own experience helping a family member, patience in gradually increasing the dose makes a world of difference in tolerability. The nausea can be discouraging, but sticking to smaller, more frequent meals and rotating injection sites as suggested truly helped mitigate discomfort. What stood out to me was the emphasis on not exceeding doses without healthcare oversight — a point that I feel many might underestimate given how tempting it can be to push for faster results. It’s equally interesting to consider the role the gut microbiome might play in these side effects, as the post touched on. I wonder if incorporating dietary prebiotics alongside semaglutide could become a standard adjunct to improve outcomes down the line. For readers who have been on semaglutide, how have you managed these initial side effects, and have you noticed any shifts in effectiveness when combining the treatment with lifestyle changes or dietary adjustments? Sharing these practical insights could be really valuable for others just starting this journey.
This article offers a comprehensive overview of the importance of injection technique and site rotation in semaglutide therapy. From personal experience working with patients, I have seen how neglecting site rotation can lead to lipohypertrophy, which not only affects the cosmetic aspect but also impairs drug absorption. I’ve found that incorporating detailed site mapping and keeping an injection diary significantly helps patients adhere to rotation schedules and monitor tissue health. It’s interesting to note how emerging research on tissue microenvironment can influence absorption and long-term efficacy.
What strategies have others found effective to educate and motivate patients to consistently rotate injection sites, especially in busy or less-motivated populations? Also, how do you handle cases where tissue fibrosis begins to develop despite guidance? Sharing such experiences could help refine best practices for sustaining treatment success and minimizing tissue complications.
Reading through this comprehensive guide, I really appreciate the emphasis on gradual dose escalation and meticulous injection site rotation. In my practice, I’ve noticed that patients often underestimate the importance of rotating sites, leading to lipohypertrophy which can hinder absorption. Using a visual map or keeping a dedicated diary has been quite effective in encouraging consistency.
What are others’ thoughts on integrating new digital tools, like mobile apps, to help patients track their injection sites and monitor tissue changes over time? I’ve found that tech solutions really improve compliance and early detection of issues. Also, considering emerging research on the microenvironment’s role, have any practitioners experimented with specific techniques or products to improve tissue health before injections? Looking forward to hearing diverse strategies—sharing our experiences can really help refine best practices for long-term management of injection-related complications.