Understanding Semaglutide’s Mechanism in Clinical Weight Loss Transformations
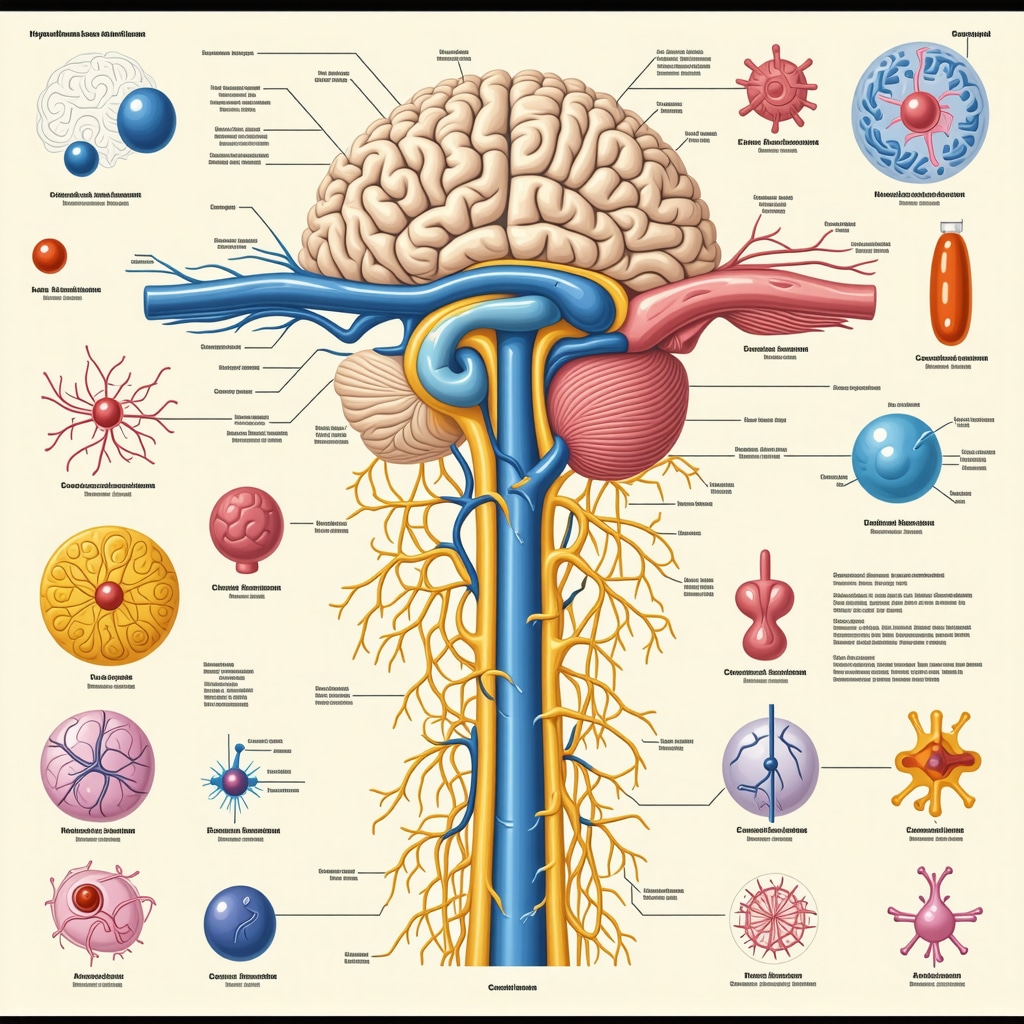
Semaglutide, a glucagon-like peptide-1 (GLP-1) receptor agonist, has redefined the landscape of pharmacological interventions targeting obesity and metabolic disorders. Its efficacy in promoting substantial weight reduction is rooted in its ability to modulate appetite regulation centers in the hypothalamus, slow gastric emptying, and improve insulin sensitivity. These physiological effects collectively facilitate a negative energy balance, essential for sustainable fat loss.
Quantitative Evidence from Clinical Trials Demonstrating Semaglutide’s Efficacy
Robust randomized controlled trials, including the SCALE (Satiety and Clinical Adiposity—Liraglutide Evidence) and STEP (Semaglutide Treatment Effect in People with obesity) programs, have consistently demonstrated average weight reductions exceeding 15% of baseline body weight over 68 weeks. Notably, these trials elucidate not only the magnitude of weight loss but also improvements in cardiometabolic markers, underscoring Semaglutide’s comprehensive therapeutic profile.
What Are the Long-Term Implications of Semaglutide-Induced Weight Loss on Metabolic Health?
Emerging data suggest that sustained Semaglutide use contributes to durable weight loss maintenance and mitigates risks associated with type 2 diabetes mellitus and cardiovascular diseases. However, the long-term safety profile necessitates continuous evaluation, particularly concerning pancreatic health and potential gastrointestinal adverse events.
Real-World Clinical Transformations: Beyond Controlled Environments
Beyond clinical trials, patient-reported outcomes and observational studies reveal transformative changes in body composition, quality of life, and psychological well-being. These real-world results, often documented through before-and-after imagery and detailed case analyses, validate Semaglutide’s applicability as a cornerstone in medical weight loss programs. Interested readers can explore real Semaglutide before and after results that inspire change.
Integrating Semaglutide Treatment With Lifestyle Modifications for Maximized Outcomes
Optimal weight loss outcomes are achieved by coupling Semaglutide administration with tailored dietary strategies, such as intermittent fasting or balanced caloric restriction, and supervised physical activity regimens. Evidence-based protocols recommend physician oversight to adjust dosages and monitor patient response, ensuring safety and efficacy. For detailed guidance, refer to doctor-supervised Semaglutide dosage guidelines.
Expert Perspectives on Semaglutide’s Role in Modern Obesity Management
Leading endocrinologists and obesity specialists advocate for Semaglutide as a paradigm shift in obesity pharmacotherapy, emphasizing its superior efficacy relative to prior GLP-1 analogs and appetite suppressants. The drug’s FDA approval, as documented in comprehensive clinical reviews such as New England Journal of Medicine, further corroborates its clinical value and safety profile.
Call to Action: Explore Advanced Semaglutide Treatment Protocols and Share Your Clinical Insights
Healthcare professionals and researchers are encouraged to delve into nuanced treatment plans and contribute to evolving evidence by visiting our expert resources on expert Semaglutide treatment guides. Sharing clinical experiences will foster a richer understanding of individualized patient responses and optimize weight loss strategies.
Exploring Semaglutide’s Influence on Gut Microbiota and Metabolic Adaptation
Recent investigations have begun to elucidate the intricate interactions between Semaglutide and the gut microbiome, revealing its potential role in modulating microbial populations that influence energy homeostasis and systemic inflammation. This emerging area suggests that Semaglutide’s efficacy may extend beyond central appetite regulation to include peripheral mechanisms that optimize metabolic adaptation during weight loss.
These insights underscore the importance of integrating microbiome-friendly dietary elements alongside Semaglutide therapy to potentially enhance therapeutic outcomes and mitigate metabolic slowdown that often accompanies caloric restriction.
Tailoring Semaglutide Dosage: Precision Medicine Approaches for Enhanced Safety and Efficacy
Individual variability in pharmacokinetics and pharmacodynamics of Semaglutide necessitates personalized dosing strategies. Factors such as baseline BMI, metabolic rate, comorbidities, and concomitant medications influence treatment response and side effect profiles. Precision medicine frameworks advocate for dynamic dosage adjustments, guided by continuous patient monitoring and biomarkers, to maximize weight loss benefits while minimizing adverse events.
Clinicians are encouraged to consult detailed protocols on doctor-supervised Semaglutide safe dosage guidelines to align personalized regimens with evidence-based standards.
How Can Integrative Strategies Amplify Semaglutide-Induced Weight Loss While Ensuring Patient-Centric Safety?
This question invites exploration into combining pharmacotherapy with behavioral interventions, nutritional optimization, and emerging adjunctive treatments. Understanding patient-specific barriers and facilitators enables the design of comprehensive plans that sustain engagement and long-term success.
Recent reviews highlight that coupling Semaglutide with intermittent fasting, structured physical activity, and psychological support significantly enhances outcomes, emphasizing the holistic nature of obesity management (National Institutes of Health, 2021).
Addressing Safety Concerns: Monitoring and Managing Semaglutide’s Adverse Effects
While Semaglutide is generally well-tolerated, gastrointestinal symptoms such as nausea, vomiting, and diarrhea are common, especially during dose escalation phases. Proactive management strategies including gradual titration, patient education, and adjunctive dietary modifications can mitigate these effects.
Long-term surveillance for rare but serious adverse events remains imperative, with a particular focus on pancreatic health, thyroid function, and cardiovascular parameters. Collaborative care models involving endocrinologists, dietitians, and primary care providers optimize surveillance and intervention.
For comprehensive safety practices, readers are advised to review safe dosage and usage tips for Semaglutide injections.
Expanding Access: Semaglutide in Diverse Populations and Health Equity Considerations
Equitable access to Semaglutide treatment remains a critical challenge, particularly in underserved populations disproportionately affected by obesity. Socioeconomic factors, healthcare literacy, and systemic barriers influence treatment uptake and adherence.
Implementing culturally sensitive education, affordable care models, and telemedicine platforms may bridge gaps, ensuring broader dissemination of Semaglutide’s benefits. Ongoing research must prioritize diverse cohort inclusion to validate efficacy and safety across demographic strata.
Join the Conversation: Share Your Experiences and Discover Advanced Semaglutide Treatment Insights
We invite healthcare professionals, researchers, and patients to contribute their perspectives and clinical experiences in our community. Engaging with expert-curated resources such as our expert Semaglutide treatment guide fosters knowledge exchange and advances patient-centered care.
Neuroendocrine Modulation: Deep Dive Into Semaglutide’s Central Nervous System Effects on Satiety and Reward Pathways
Semaglutide’s impact extends beyond peripheral metabolic regulation, intricately modulating hypothalamic nuclei responsible for hunger and energy expenditure. Recent neuroimaging studies reveal altered activity within the arcuate nucleus and mesolimbic reward circuits, effectively recalibrating not only caloric intake but also hedonic eating behaviors. This dual action disrupts the usual neurochemical feedback loops driving compulsive overeating, a cornerstone challenge in obesity management.
Moreover, the drug’s GLP-1 receptor agonism influences secretion of neuropeptides such as proopiomelanocortin (POMC) and neuropeptide Y (NPY), which orchestrate the balance of anorexigenic and orexigenic signals. This sophisticated neuroendocrine crosstalk facilitates sustained appetite suppression, potentiating long-term adherence to caloric restriction without invoking compensatory metabolic adaptations.
Pharmacogenomics and Personalized Medicine: Tailoring Semaglutide Therapy Through Genetic Profiling
Emerging research underscores the relevance of genetic polymorphisms in GLP-1 receptor genes and metabolic enzymes affecting Semaglutide pharmacodynamics and pharmacokinetics. For instance, variants in GLP1R and DPP4 genes have been correlated with differential receptor sensitivity and drug metabolism, respectively, thereby influencing efficacy and tolerability profiles.
Incorporating pharmacogenomic screening into clinical decision-making enables clinicians to anticipate treatment response variability and adverse event risk, tailoring dosages and adjunctive interventions accordingly. This precision approach promises to optimize therapeutic indices, reduce trial-and-error prescribing, and enhance patient satisfaction.
What Are the Prospects and Limitations of Pharmacogenomic-Guided Semaglutide Dosing in Clinical Practice?
While the potential benefits of genotype-informed Semaglutide administration are compelling, current limitations include accessibility of genetic testing, cost-effectiveness, and the incomplete understanding of polygenic influences on drug response. Nonetheless, ongoing trials are systematically evaluating these parameters to establish evidence-based guidelines.
Clinicians interested in advancing personalized obesity pharmacotherapy can reference the detailed review published by The Pharmacogenomics Journal (2021), which critically appraises the state of genetic markers influencing GLP-1 receptor agonists.
Synergistic Adjuncts: Combining Semaglutide With Emerging Therapeutics and Lifestyle Innovations for Amplified Weight Loss
Strategic integration of Semaglutide with novel agents such as dual GIP/GLP-1 receptor agonists or amylin analogs is under active investigation, aiming to harness complementary mechanisms to overcome physiological weight loss plateaus. Additionally, coupling pharmacotherapy with cutting-edge lifestyle interventions — including digital phenotyping to customize behavioral counseling and AI-driven nutritional algorithms — represents the frontier of comprehensive obesity care.
Such multimodal approaches not only potentiate weight reduction but also address psychological components like emotional eating and motivation, which traditionally impede sustained success.
Call to Action: Engage With Advanced Semaglutide Protocols and Contribute to Precision Obesity Management
Healthcare practitioners and researchers are encouraged to deepen their expertise by exploring our expert Semaglutide treatment guide, which presents state-of-the-art protocols incorporating pharmacogenomic insights and integrative care models. Your clinical observations and data sharing are invaluable to refining personalized strategies and expanding the therapeutic horizon.
Unveiling Semaglutide’s Neuroendocrine Impact on Satiety and Reward Circuitry
Semaglutide transcends traditional metabolic intervention by intricately modulating central nervous system pathways governing hunger and reward. Cutting-edge neuroimaging elucidates its influence on hypothalamic arcuate nucleus activity and mesolimbic dopamine circuits, recalibrating both homeostatic and hedonic feeding drives. This dual modulation disrupts compulsive eating behaviors, a critical barrier in obesity treatment, while enhancing sustained appetite suppression through regulated secretion of neuropeptides like proopiomelanocortin (POMC) and neuropeptide Y (NPY). Such sophisticated neuroendocrine orchestration facilitates adherence to caloric deficits without triggering compensatory metabolic adaptations.
Pharmacogenomic Stratification: Pioneering Personalized Semaglutide Dosing Paradigms
Emerging pharmacogenomic data underscore the significance of genetic polymorphisms within GLP1R and DPP4 loci that modulate Semaglutide’s pharmacodynamics and pharmacokinetics. By integrating genetic profiling into clinical frameworks, prescribers can anticipate interindividual variability in drug efficacy and tolerability, enabling genotype-guided dose optimization that minimizes adverse outcomes. Although challenges remain—including accessibility of genetic testing and polygenic complexity—ongoing research signals a transformative trajectory towards precision obesity pharmacotherapy.
What Are the Prospects and Limitations of Pharmacogenomic-Guided Semaglutide Dosing in Clinical Practice?
The clinical utility of pharmacogenomic-guided Semaglutide administration presents compelling opportunities for enhancing therapeutic indices through tailored dosing strategies. However, implementation hurdles such as cost constraints, limited availability of rapid genetic assays, and incomplete elucidation of multigenic influences temper immediate widespread adoption. Critical analyses, such as the comprehensive review published in The Pharmacogenomics Journal (2021), provide an authoritative foundation for clinicians aiming to navigate these complexities and contribute to evolving evidence.
Synergistic Integration: Amplifying Weight Loss via Combination Therapies and Innovative Lifestyle Approaches
Current investigational paradigms focus on synergizing Semaglutide with emerging agents like dual glucose-dependent insulinotropic polypeptide (GIP)/GLP-1 receptor agonists and amylin analogs to surmount physiologic plateaus inherent to monotherapy. Concurrently, leveraging digital phenotyping and artificial intelligence-driven nutritional algorithms enhances personalization of behavioral interventions, addressing psychological determinants such as emotional eating and motivational fluctuations. This integrative model not only intensifies weight reduction trajectories but also fortifies long-term adherence through comprehensive biopsychosocial engagement.
Proactive Safety Optimization: Navigating Adverse Effects Through Precision Monitoring
Despite its favorable safety profile, Semaglutide’s dose-escalation phase commonly elicits gastrointestinal adverse events necessitating vigilant patient education and individualized titration schedules. Integrating biomarker surveillance and multidisciplinary collaboration enhances early detection of rare but critical events involving pancreatic and thyroid function. These strategies underpin a precision medicine approach that balances maximal efficacy with patient-centric safety.
Engage with Cutting-Edge Semaglutide Protocols to Elevate Obesity Management Outcomes
Healthcare professionals and researchers are invited to explore advanced Semaglutide treatment frameworks incorporating pharmacogenomic insights and integrative therapeutic modalities through our expert Semaglutide treatment guide. Contributing clinical experiences and data will propel the refinement of personalized obesity interventions, fostering a collaborative advancement in patient-centered care.
Expert Insights & Advanced Considerations
Neuroendocrine Modulation as a Cornerstone of Sustained Weight Loss
Semaglutide’s ability to finely tune central appetite and reward circuits, particularly within the hypothalamic arcuate nucleus and mesolimbic pathways, offers a mechanistic basis for its superior efficacy. This neuroendocrine modulation disrupts compulsive eating and supports long-term adherence to caloric deficits without triggering metabolic compensation, a breakthrough in obesity pharmacotherapy.
Pharmacogenomic Profiling Enhances Personalized Semaglutide Dosing
Incorporating genetic markers such as polymorphisms in GLP1R and DPP4 genes can predict interindividual variability in drug response and tolerability. While still emerging, pharmacogenomic-guided protocols facilitate precision dosing strategies that optimize therapeutic outcomes and minimize adverse effects, heralding a new era of individualized obesity treatment.
Synergistic Combination Therapies and Digital Innovations Amplify Outcomes
Combining Semaglutide with novel agents—like dual GIP/GLP-1 receptor agonists—and integrating AI-driven nutritional algorithms and digital phenotyping for behavioral counseling represent cutting-edge strategies. These multimodal approaches address both physiological and psychological obstacles to weight loss, enhancing magnitude and durability of fat reduction.
Proactive Safety Surveillance Is Essential for Optimal Management
Despite Semaglutide’s favorable safety profile, gastrointestinal events during dose escalation and rare metabolic concerns require vigilant monitoring. Precision medicine models leveraging biomarker assessments and multidisciplinary care optimize safety while maintaining efficacy, ensuring patient-centric management.
Equity and Accessibility Must Guide Semaglutide Implementation
Addressing disparities through culturally competent education, affordable care pathways, and telemedicine is critical to broadening Semaglutide’s impact. Prioritizing diverse population inclusion in research and clinical programs safeguards efficacy and safety across demographic groups.
Curated Expert Resources
- New England Journal of Medicine – Semaglutide Clinical Trials: Authoritative peer-reviewed publications detailing comprehensive efficacy and safety data underpinning FDA approval and clinical guidelines.
- The Pharmacogenomics Journal (2021): A critical review of genetic markers influencing GLP-1 receptor agonist responses, essential for clinicians exploring personalized dosing approaches.
- National Institutes of Health (NIH) Reviews on Obesity Pharmacotherapy: Cutting-edge analyses integrating behavioral, pharmacological, and metabolic data relevant to Semaglutide and combinatory treatments.
- Expert Semaglutide Treatment Guide: A comprehensive resource offering advanced protocols, dosage optimization strategies, and integrative care models for practitioners.
- Doctor Supervised Semaglutide Safe Dosage Guidelines: Practical insights into titration schedules, side effect management, and patient monitoring to ensure safe, effective treatment.
Final Expert Perspective
Semaglutide represents a paradigm shift in obesity management, combining profound neuroendocrine effects with emerging personalized medicine frameworks to achieve rapid, sustainable weight loss. Its integration with innovative combination therapies and digital behavioral interventions further enhances patient outcomes. Equally important is a vigilant, patient-centric approach to safety and equitable access, ensuring this powerful tool benefits diverse populations. For clinicians and researchers committed to advancing obesity care, engaging with expert resources such as the expert Semaglutide treatment guide is indispensable. We invite you to deepen your expertise, share clinical insights, and contribute to the evolving landscape of precision weight loss with Semaglutide.

