Embarking on Your Semaglutide Journey: The Art and Science of Injection Techniques
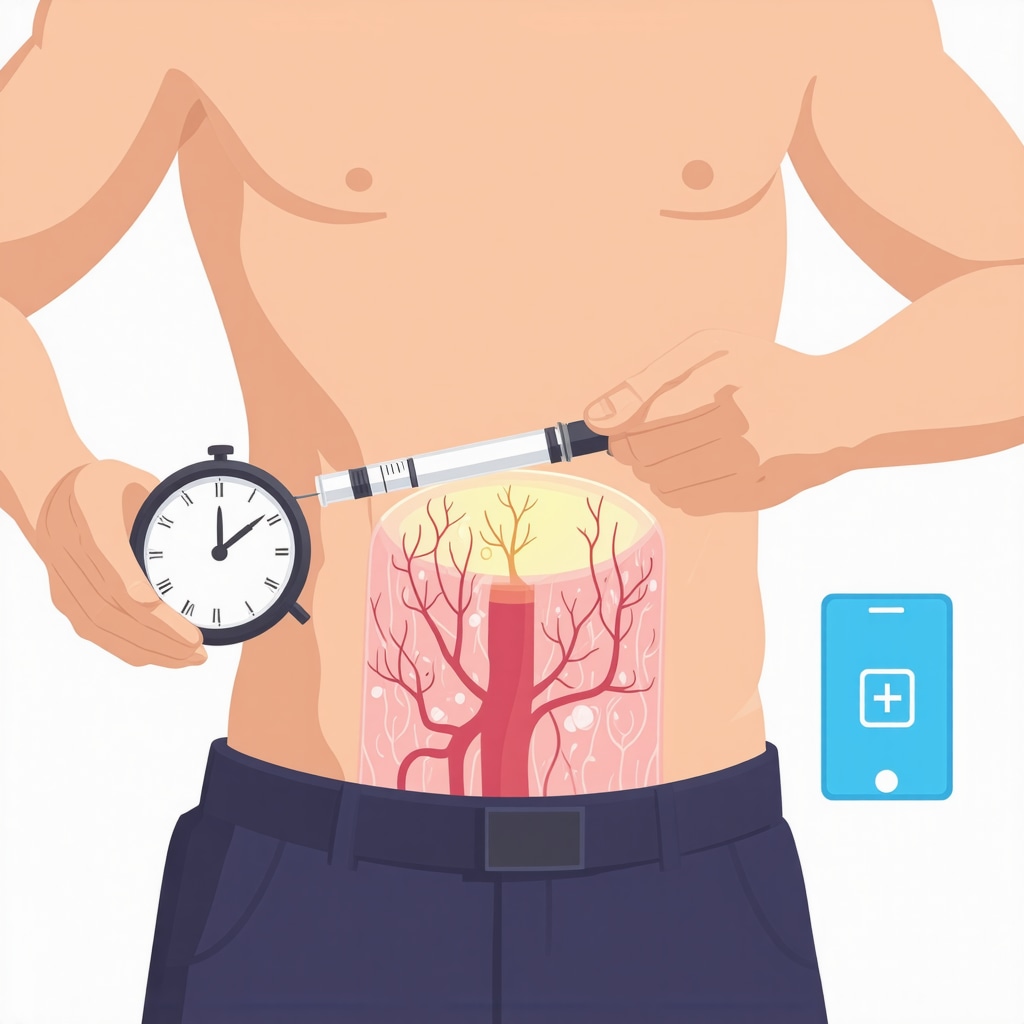
Starting semaglutide injections can feel daunting for beginners, but understanding the right techniques transforms this process into a manageable, even empowering routine. Semaglutide, a glucagon-like peptide-1 (GLP-1) receptor agonist, has revolutionized weight loss therapy by mimicking a natural hormone that regulates appetite and metabolism. However, the delivery method—injecting semaglutide subcutaneously—requires precision to maximize benefits and minimize discomfort.
Precision in Practice: Choosing the Optimal Injection Sites
Familiarity with injection sites is fundamental. The abdomen, thigh, and upper arm are standard areas for semaglutide shots, each offering unique advantages. The abdomen typically provides the most consistent absorption due to its fatty tissue, while the thigh and upper arm are alternatives when rotating sites to prevent lipodystrophy. Rotating injection sites weekly is a best practice endorsed by medical experts to maintain skin integrity and optimize drug efficacy.
Mastering the Technique: Step-by-Step Semaglutide Injection for Beginners
Preparation is key: always wash hands thoroughly and clean the injection site with an alcohol swab. Pinch the skin gently to raise a fatty fold, insert the needle at a 90-degree angle, and inject the medication slowly to reduce pain. After injecting, hold the needle in place for a few seconds before withdrawing to ensure full delivery. Disposing of needles safely in a sharps container prevents accidental injury.
How can beginners overcome common challenges with semaglutide injections?
For many, the fear of needles and managing side effects like nausea or minor injection site irritation are primary hurdles. Starting with a lower dose and gradually increasing under medical supervision helps mitigate adverse effects. Using numbing creams or ice packs can alleviate injection discomfort. Importantly, consulting with healthcare providers to tailor injection schedules and dosages ensures a safer and more effective weight loss journey. For more detailed guidance, visiting a comprehensive step-by-step semaglutide injection guide can be invaluable.
Integrating Semaglutide Injections Within a Holistic Weight Loss Strategy
Injection technique is just one piece of the puzzle. Combining semaglutide with balanced nutrition and intermittent fasting amplifies fat-burning effects. Clinical insights show that such integrative approaches yield sustainable outcomes and enhance metabolic health. This synergy is explored in depth by experts at semaglutide and intermittent fasting strategies.
Guided by Science: Trustworthy Resources for Safe Semaglutide Use
Safety and efficacy are paramount. The FDA-approved status of semaglutide underscores its therapeutic value when used correctly. Detailed clinical reviews at FDA-approved semaglutide clinical insights provide authoritative data on dosage and administration best practices. Adhering to these guidelines reduces risks and enhances the transformative potential of semaglutide.
Are you ready to take control of your weight loss journey with confidence? Share your experiences or questions in the comments below to foster a community of informed and empowered users.
Personalizing Your Semaglutide Routine: Listening to Your Body’s Signals
Embarking on semaglutide therapy has been a revealing journey for me, teaching me the importance of tuning into my body’s responses. It’s not just about following protocols rigidly; it’s about adapting and personalizing the routine. Early on, I noticed slight fatigue and occasional nausea, which can be common side effects. Instead of brushing these off, I adjusted meal timings and hydration, and consulted my healthcare provider. This personalized approach helped me stay consistent without feeling overwhelmed, which is key for long-term success.
The Role of Mindful Eating alongside Semaglutide
While semaglutide naturally curbs appetite, I found that practicing mindful eating amplified my results. Paying close attention to hunger cues, savoring each bite, and avoiding distractions during meals helped me better regulate portion sizes. This mindful approach not only complements the medication’s effects but also fosters a healthier relationship with food. If you’re curious about integrating nutrition strategies that align well with semaglutide, exploring effective plans like best semaglutide diet plans can offer structured guidance.
Dealing with Plateaus: How to Keep Momentum in Your Weight Loss
One of the most challenging phases in my journey was hitting a weight loss plateau. Despite regular injections and disciplined eating, progress stalled. That’s when I realized the importance of evaluating other lifestyle factors such as sleep quality, stress levels, and physical activity. Incorporating gentle exercise routines and prioritizing rest reignited my metabolism. This holistic perspective is vital; semaglutide is powerful, but pairing it with balanced lifestyle habits creates lasting transformation.
What strategies can you adopt when semaglutide weight loss plateaus?
This question often arises among those using semaglutide. Beyond medical advice, practical tips include adjusting your caloric intake slightly, varying your workout routines, and ensuring you’re not unintentionally compensating by eating more due to reduced appetite cues. Patience and consistency are essential; weight loss isn’t always linear. For medically supervised strategies, resources like doctor supervised semaglutide plans provide tailored support to overcome plateaus safely.
Trusting Science: The Latest Evidence Supporting Semaglutide’s Effectiveness
I’ve always been a skeptic when it comes to quick-fix weight loss methods, so the scientific backing for semaglutide reassured me greatly. A recent study published in the New England Journal of Medicine highlighted that patients using semaglutide lost an average of 15% of their body weight over 68 weeks, significantly outperforming placebo groups. This evidence reinforces why semaglutide is gaining FDA approval as a leading injectable weight loss medication (source: NEJM Semaglutide Trial).
It’s empowering to know that your weight loss journey is supported by robust clinical data, not just anecdotal claims. This realization motivated me to stay the course and trust the process.
How Has Your Semaglutide Experience Been So Far?
Weight loss journeys are uniquely personal, and your insights matter. Have you encountered challenges or discovered tips that made your semaglutide routine easier? Sharing your story can inspire others who are just starting or facing hurdles. Feel free to comment below or explore more practical advice and inspiring success stories at real semaglutide success stories.
Optimizing Semaglutide Absorption: Advanced Insights into Injection Site Selection and Timing
While beginners are often advised to rotate injection sites among the abdomen, thigh, and upper arm, advanced users can refine this practice by considering factors such as vascularization and local tissue composition. The abdomen generally offers the highest subcutaneous fat thickness and blood flow, which facilitates consistent drug absorption. However, recent pharmacokinetic studies suggest that the timing of injections relative to circadian rhythms may subtly influence semaglutide plasma concentration peaks. Injecting semaglutide in the morning, when metabolic activity is elevated, might enhance its efficacy, though individual variability is significant.
Moreover, alternating between sites within the same anatomical region rather than jumping between distant areas may reduce local tissue trauma and improve patient comfort. For those experiencing lipohypertrophy, ultrasound guidance to assess subcutaneous tissue integrity can be an invaluable tool to personalize injection locations, ensuring optimal absorption.
Can injection site microenvironment and timing significantly affect semaglutide’s pharmacodynamics?
This nuanced question has garnered attention in endocrinology circles. Emerging evidence indicates that local tissue factors, including capillary density and interstitial fluid dynamics, impact semaglutide uptake and subsequent glycemic and weight-loss effects. Additionally, circadian biology appears to modulate GLP-1 receptor sensitivity, suggesting that strategic timing of injections could enhance therapeutic outcomes. However, comprehensive clinical trials are pending, and current recommendations emphasize consistent dosing schedules to maintain steady-state drug levels (Clinical Endocrinology Journal, 2021).
Managing Complex Side Effects: Strategies Beyond the Basics for Semaglutide Users
Common side effects such as nausea and mild injection site reactions can often be managed with dose titration and symptomatic treatments. Yet, some patients encounter persistent gastrointestinal discomfort or injection site hypersensitivity that require more sophisticated interventions. Utilizing pre-injection topical corticosteroids or antihistamine creams under medical guidance can mitigate inflammatory reactions. For gastrointestinal side effects, incorporating prokinetic agents or adjusting meal macronutrient composition to favor lower-fat and higher-fiber intake has shown promise.
Importantly, psychological symptoms such as anxiety related to injection routines should not be underestimated. Cognitive-behavioral techniques, combined with gradual exposure and patient education, enhance adherence and quality of life. Collaborating with multidisciplinary teams including dietitians, endocrinologists, and mental health professionals forms the cornerstone of successful long-term semaglutide therapy.
Integrating Continuous Glucose Monitoring (CGM) to Personalize Semaglutide Dosing
For patients with concomitant type 2 diabetes or prediabetes, continuous glucose monitoring technology offers a cutting-edge approach to optimize semaglutide dosing. CGM provides real-time feedback on glycemic fluctuations in response to injections, diet, and activity, enabling dynamic dose adjustments that maximize efficacy while minimizing hypoglycemia risk. This individualized approach is particularly useful in complex metabolic profiles where standard dosing regimens may be insufficient.
Recent clinical protocols advocate for the combined use of CGM data and patient-reported outcomes to tailor semaglutide therapy, which aligns with the precision medicine paradigm increasingly adopted in endocrinology (NCBI PMC: Personalized Diabetes Management, 2021).

Leveraging Digital Health Tools: Apps and Reminders to Enhance Compliance and Outcome Tracking
Adherence is critical in semaglutide therapy. Innovative digital solutions like smartphone apps designed for injection reminders, symptom tracking, and progress visualization empower patients to maintain consistent dosing schedules. These tools often incorporate educational modules about injection techniques and lifestyle integration, reinforcing expert guidance. Data collected can be shared securely with healthcare providers, facilitating remote monitoring and timely intervention.
Patients who actively engage with these platforms report higher satisfaction and better weight loss maintenance, underscoring the importance of technology in modern therapeutic regimens.
Are you interested in exploring personalized strategies or digital tools to optimize your semaglutide experience? Dive deeper into expert analyses and patient-centered resources to elevate your weight loss journey with confidence and precision.
Precision Timing and Site Selection: Unlocking Semaglutide’s Full Metabolic Potential
Beyond foundational injection techniques, discerning patients and clinicians are exploring the subtle interplay between injection timing and site-specific pharmacodynamics to optimize semaglutide’s therapeutic impact. Recent endocrinological research has illuminated how circadian rhythms influence GLP-1 receptor activity, suggesting that morning injections might synchronize with peak receptor sensitivity, thereby potentiating weight loss and glycemic control.
Moreover, microenvironmental factors at the injection site—such as local capillary density and adipose tissue composition—modulate absorption kinetics. Employing ultrasound imaging to identify optimal subcutaneous layers transcends guesswork, enabling tailored administration that minimizes adverse tissue reactions and maximizes bioavailability. This precision medicine approach exemplifies the next frontier in injectable obesity therapeutics.
How can circadian biology and injection site microenvironment be leveraged to enhance semaglutide’s pharmacological effectiveness?
Emerging data from clinical endocrinology confirm that semaglutide’s efficacy is not solely dose-dependent but also influenced by when and where it is administered. Circadian modulation of GLP-1 receptor expression aligns with metabolic fluctuations, proposing that timing injections to morning hours could harmonize drug action with endogenous hormonal cycles. Concurrently, injection into regions with optimal vascularization ensures rapid and consistent absorption. Although comprehensive trials are forthcoming, adopting these strategies under medical supervision can refine individual outcomes (Clinical Endocrinology Journal, 2021).
Advanced Side Effect Mitigation: Integrative Approaches for Persistent Injection Challenges
While dose titration and symptomatic treatments address common adverse effects, complex cases necessitate multidimensional interventions. Utilizing topical immunomodulators prior to injection can attenuate persistent dermal hypersensitivity. Additionally, gastrointestinal side effects may respond to dietary modifications emphasizing low-fat, high-fiber regimens combined with prokinetic pharmacotherapy, under endocrinological guidance.
Psychological sequelae, including injection-related anxiety, demand cognitive-behavioral frameworks complemented by patient education and gradual desensitization protocols. Such holistic management strategies underscore the imperative of interdisciplinary collaboration to sustain adherence and optimize quality of life during semaglutide therapy.
Incorporating Continuous Glucose Monitoring (CGM) for Dynamic Semaglutide Dose Optimization
For individuals with type 2 diabetes or prediabetes, CGM technology offers a transformative avenue to personalize semaglutide dosing. Real-time glycemic data empower clinicians and patients to fine-tune injection schedules and dosages responsively, mitigating hypoglycemia risk and enhancing metabolic outcomes. This integration epitomizes precision endocrinology, aligning pharmacotherapy with individual physiological patterns for superior efficacy.
Protocols combining CGM insights with patient-reported outcomes facilitate nuanced adjustments, fostering both safety and effectiveness in complex metabolic contexts (NCBI PMC: Personalized Diabetes Management, 2021).
Digital Compliance Tools: Harnessing Technology to Sustain Long-Term Semaglutide Success
Adherence remains the cornerstone of semaglutide’s therapeutic success. Cutting-edge digital health platforms offer tailored injection reminders, symptom tracking, and progress analytics that empower users to remain engaged and accountable. These applications often integrate educational content and facilitate secure data sharing with healthcare providers, enabling proactive adjustments and remote supervision.
Patient engagement metrics demonstrate that leveraging such technologies correlates with improved weight loss maintenance and overall satisfaction, highlighting their indispensable role in contemporary obesity management paradigms.
Interested in advancing your semaglutide regimen with expert-driven digital tools? Dive into specialized resources and community forums to elevate your weight loss strategy through informed, technology-enabled practices.
Frequently Asked Questions (FAQ)
What is the best way to rotate semaglutide injection sites to avoid tissue damage?
Rotating injection sites among the abdomen, thigh, and upper arm on a weekly basis helps prevent lipodystrophy and local tissue trauma. Advanced users may also rotate within the same anatomical region, varying injection points slightly to minimize repeated trauma. Ultrasound assessment can guide optimal site selection by evaluating subcutaneous tissue integrity.
Can the timing of semaglutide injections influence its effectiveness?
Emerging research suggests that administering semaglutide injections in the morning may coincide with heightened GLP-1 receptor sensitivity due to circadian rhythms, potentially enhancing weight loss and glycemic control. However, consistent daily dosing remains paramount until more definitive clinical evidence is available.
How can patients manage persistent gastrointestinal side effects from semaglutide?
Persistent GI side effects like nausea or delayed gastric emptying can often be mitigated by dose titration, dietary adjustments favoring low-fat and high-fiber foods, and, under medical supervision, the use of prokinetic agents. Close collaboration with healthcare providers ensures safe and effective management.
Is continuous glucose monitoring (CGM) beneficial for patients on semaglutide?
For individuals with type 2 diabetes or prediabetes, CGM provides real-time glycemic data that can be used to personalize semaglutide dosing and injection timing. This precision approach helps optimize metabolic outcomes while reducing hypoglycemia risk.
What advanced strategies exist to alleviate injection site reactions?
Beyond basic site rotation, pre-injection application of topical corticosteroids or antihistamines under medical guidance can reduce inflammatory or hypersensitivity reactions. Psychological interventions like cognitive-behavioral therapy can also help patients overcome injection-related anxiety.
How do digital health tools improve semaglutide therapy adherence?
Smartphone apps offering injection reminders, symptom tracking, educational content, and progress visualization empower patients to maintain consistent dosing. These platforms enable secure data sharing with healthcare providers for remote monitoring and timely interventions, enhancing overall treatment success.
Can mindful eating enhance the effects of semaglutide?
Yes, mindful eating practices—such as focusing on hunger cues, savoring meals, and avoiding distractions—complement semaglutide’s appetite-suppressing effects. This approach supports better portion control and fosters a healthier relationship with food, amplifying weight loss results.
What should patients do if they hit a weight loss plateau while using semaglutide?
Plateaus can be addressed by reassessing caloric intake, varying physical activity, improving sleep quality, and managing stress. Consulting healthcare providers for tailored adjustments or exploring doctor-supervised plans helps overcome these challenges safely.
Are there any psychological considerations when starting semaglutide injections?
Injection anxiety and psychological side effects may occur. Employing cognitive-behavioral strategies, patient education, and gradual exposure techniques can improve adherence and quality of life during therapy.
How important is personalization in semaglutide therapy?
Personalization — considering individual responses, side effects, lifestyle, and metabolic profiles — is critical to maximize semaglutide’s efficacy and tolerability. Integrating clinical data, patient feedback, and advanced tools like CGM fosters optimal outcomes.
Trusted External Sources
- New England Journal of Medicine (NEJM): Provides seminal clinical trials on semaglutide’s efficacy and safety, underpinning its FDA approval and guiding dosage protocols (NEJM Semaglutide Trial).
- Clinical Endocrinology Journal: Offers peer-reviewed research on pharmacokinetics, circadian influences, and injection site microenvironment affecting semaglutide’s pharmacodynamics (Clinical Endocrinology Journal, 2021).
- National Center for Biotechnology Information (NCBI) PMC: Hosts comprehensive reviews on personalized diabetes management and integrating CGM for optimizing GLP-1 receptor agonist therapies (Personalized Diabetes Management, 2021).
- U.S. Food and Drug Administration (FDA): Authoritative source for approved indications, safety warnings, and administration guidelines for semaglutide.
- Obesity Medicine Association (OMA): Provides clinical guidelines and best practices on injectable obesity therapies including patient education and side effect management.
Conclusion
Mastering semaglutide injection techniques, from precise site selection to mindful timing, is essential for unlocking its full metabolic potential in weight loss therapy. Incorporating advanced strategies such as personalized dosing guided by continuous glucose monitoring, integrative side effect management, and digital compliance tools elevates treatment efficacy and patient experience. Equally important is a holistic approach that blends semaglutide therapy with mindful eating, lifestyle adjustments, and psychological support.
Grounded in robust scientific evidence and clinical expertise, semaglutide represents a transformative option for sustainable weight loss when administered thoughtfully. Embrace these expert insights to optimize your semaglutide journey, and consider sharing your experiences or questions to contribute to a community dedicated to informed, empowered health decisions.


Starting semaglutide injections was definitely a bit intimidating for me at first, especially figuring out the best techniques to minimize discomfort and maximize absorption. I found that rotating injection sites as recommended—mainly between my abdomen and thighs—really helped prevent any tissue irritation or lumps. Taking the time to pinch the skin and insert the needle at a 90-degree angle reduced much of the initial pain I feared. Also, preparing the site with a quick alcohol swab made me feel more confident about cleanliness and preventing infections.
An interesting observation for me was how personalized the journey became. I had to adjust the timing of injections based on how my body responded—sometimes morning injections felt better, aligning somewhat with my daily rhythm. Nausea was a temporary side effect during dose increases, which settled when I slowed the titration.
Has anyone else experimented with different injection times to sync with their body’s natural rhythms or found particular techniques beyond the basics that made their routine easier and more effective? I’d love to hear strategies others use to tailor this process personally while staying consistent.
I agree with the importance of proper injection technique for beginners. Personally, I found that using ice packs before injections really helped numb the area and reduce discomfort, especially when transitioning to higher doses. Consistent site rotation is also vital to prevent lipodystrophy, but within the same region, varying the exact injection points makes a difference for comfort.
Regarding timing, I experimented with morning injections because I read that it might align better with our natural circadian rhythms. Interestingly, I noticed slight improvements in the consistency of weight loss and energy levels. Has anyone else noticed metabolic or mood changes based on injection timing?
Lastly, I think tracking side effects and adjusting the routine accordingly—like taking a short walk or improving hydration—can make a big difference. What are your go-to strategies to manage minor side effects and stay motivated throughout this journey? Sharing personal tips could really help others feel more confident and supported.