Harnessing Semaglutide Within Advanced Medical Weight Loss Frameworks
In the evolving landscape of obesity management, semaglutide has emerged as a groundbreaking pharmacological agent with robust clinical validation for effective weight reduction. Its integration into structured medical weight loss programs represents a paradigm shift, offering synergistic benefits beyond monotherapy. Understanding how to unlock semaglutide’s full potential requires an expert grasp of its physiological mechanisms, optimal dosing protocols, and the importance of comprehensive patient monitoring within multidisciplinary programs.
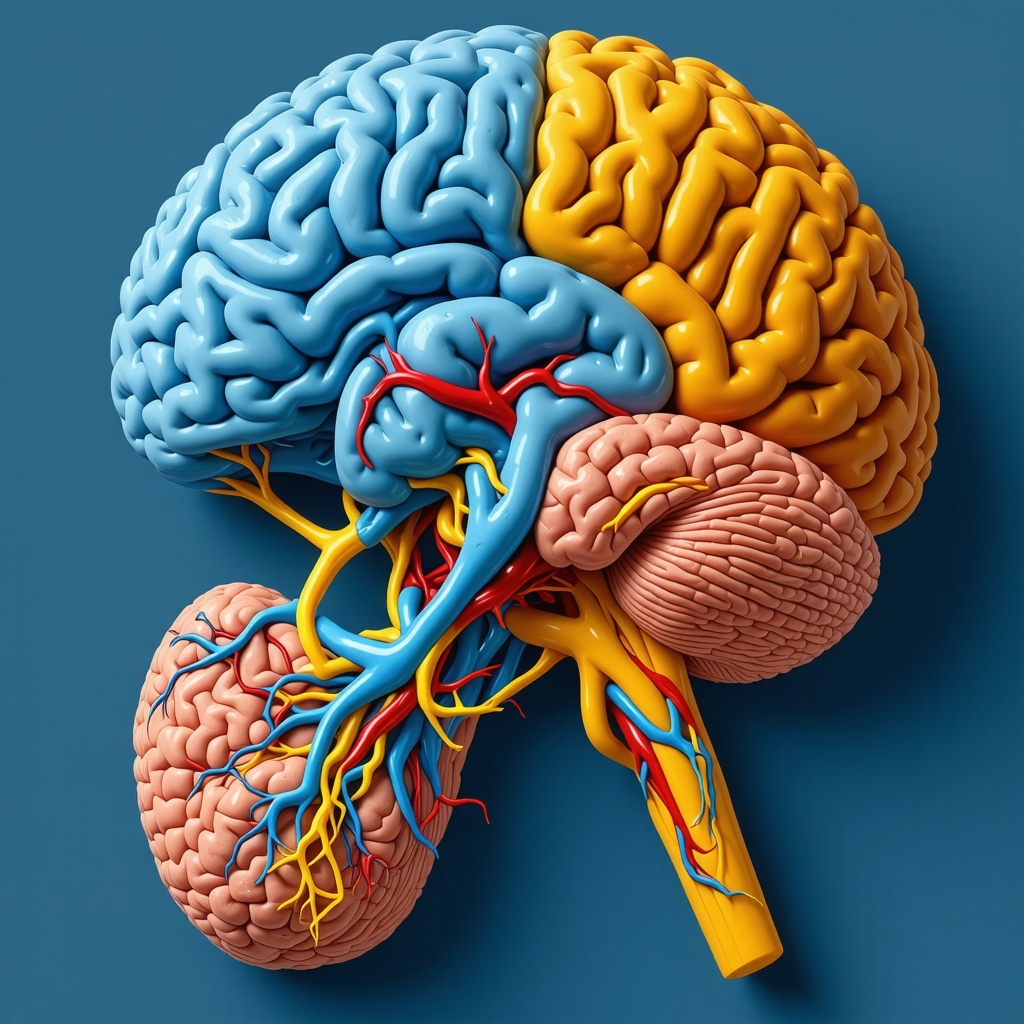
Mechanistic Insights: How Semaglutide Optimizes Metabolic Regulation
Semaglutide, a glucagon-like peptide-1 (GLP-1) receptor agonist, modulates appetite regulation centers in the hypothalamus, enhancing satiety and reducing caloric intake. This effect is compounded by delayed gastric emptying and improved insulin sensitivity, collectively facilitating sustained fat loss. When embedded in medical weight loss programs, semaglutide’s metabolic modulation aligns with nutritional counseling and behavioral interventions, amplifying long-term adherence and efficacy.
What Are the Critical Safety and Dosage Considerations in Semaglutide-Based Weight Loss Protocols?
Precision in dosage escalation schedules is paramount to minimize gastrointestinal side effects and maximize tolerability. Clinical guidelines endorse a gradual titration approach, often starting at 0.25 mg weekly and increasing to 2.4 mg as tolerated. Within supervised medical programs, continuous patient assessment ensures early identification of adverse reactions and adjustment of therapy accordingly. For detailed protocols, see doctor-supervised semaglutide safe dosage guidelines.
Integrating Semaglutide Into Multimodal Weight Loss Strategies for Enhanced Outcomes
Medical weight loss programs that combine semaglutide with adjunctive interventions such as intermittent fasting, tailored diet plans, and behavioral support yield superior results compared to pharmacotherapy alone. Evidence from recent randomized controlled trials demonstrates that this integrated approach promotes not only rapid fat reduction but also mitigates weight regain risks. The synergy between semaglutide’s pharmacodynamics and lifestyle modifications under expert supervision is critical for sustainable obesity management.
Evidence-Based Clinical Applications and Real-World Outcomes
Numerous clinical studies, including those published in the Journal of the American Medical Association, validate semaglutide’s efficacy in achieving clinically significant weight loss in diverse populations. Medical weight loss programs leveraging these insights have reported patient success stories characterized by meaningful body mass index (BMI) reductions and improved metabolic markers. Such data underscore the importance of incorporating semaglutide within evidence-based frameworks.
Call to Action: Engage with Expert-Level Resources to Master Semaglutide Weight Loss Protocols
Professionals and patients seeking to deepen their understanding of semaglutide’s role in medical weight loss are encouraged to explore comprehensive treatment guides and clinical insights available at Medical Weight Loss Programs Unlocking Success With Semaglutide. Sharing clinical experiences and advancing dialogue in expert forums further enriches collective knowledge and optimizes patient outcomes.
Optimizing Patient Selection Criteria for Semaglutide Therapy
Identifying ideal candidates for semaglutide-based weight loss programs is critical to maximizing therapeutic success. Patients with a BMI ≥30 kg/m² or ≥27 kg/m² with obesity-related comorbidities such as type 2 diabetes or hypertension typically benefit most. However, nuanced evaluation of metabolic profiles, prior weight loss attempts, and psychological readiness informs personalized treatment plans. Integrating semaglutide into multidisciplinary care ensures that biological, behavioral, and environmental factors are collectively addressed to sustain weight loss.
Synergizing Semaglutide with Nutritional and Behavioral Interventions for Sustainable Fat Loss
While semaglutide effectively suppresses appetite and regulates glucose metabolism, its efficacy is amplified when combined with evidence-based nutritional strategies and behavioral therapy. Tailored diet plans emphasizing low glycemic index foods, adequate protein intake, and mindful eating complement the drug’s pharmacodynamics. Behavioral interventions such as cognitive-behavioral therapy (CBT) and motivational interviewing enhance adherence and facilitate lifestyle changes essential for long-term weight maintenance. For expertly crafted nutritional protocols, review guide to crafting the best semaglutide diet plans for fat loss.
Exploring Emerging Research: Could Semaglutide Revolutionize Weight Loss Maintenance?
Recent trials have begun to explore semaglutide’s role not only in inducing weight loss but also in preventing weight regain, a common challenge in obesity management. Continuous low-dose maintenance therapy might sustain metabolic improvements and appetite regulation, reducing rebound weight gain. These insights suggest a potential paradigm shift toward chronic management of obesity as a relapsing disease, rather than episodic treatment. Ongoing studies will clarify optimal long-term dosing and patient monitoring frameworks.
How Can Clinicians Balance Semaglutide’s Potency with Safety in Diverse Patient Populations?
Managing semaglutide’s powerful effects requires clinician expertise in titrating doses, monitoring side effects, and tailoring treatment to individual patient profiles. Factors such as age, renal function, gastrointestinal tolerance, and coexisting conditions modulate therapy safety. Utilizing structured protocols and patient education minimizes risks while maximizing fat-burning outcomes. Healthcare providers are encouraged to stay abreast of evolving guidelines, such as those outlined in the safe dosage guidelines to prevent side effects with semaglutide shots.
Leveraging Real-World Data and Patient-Reported Outcomes in Semaglutide Programs
Beyond controlled trials, real-world evidence increasingly informs best practices in semaglutide use. Patient-reported outcomes highlight quality-of-life improvements, appetite control, and energy levels, which correlate strongly with adherence and sustained weight loss. Registries and longitudinal studies provide granular data to refine treatment algorithms and personalize care. The integration of digital health tools for remote monitoring further enhances clinical oversight and patient engagement.
According to a 2023 systematic review in The Lancet Diabetes & Endocrinology, semaglutide shows consistent efficacy across diverse demographics, underscoring its broad applicability in clinical practice.
Engage with the Community: Share Your Insights and Discover Advanced Semaglutide Strategies
We invite healthcare professionals and patients alike to contribute their experiences and questions about semaglutide-based weight loss interventions. Sharing practical tips and clinical anecdotes enriches collective expertise. For further exploration, consider visiting medical weight loss programs unlocking success with semaglutide and join the discussion to optimize your approach.
Personalizing Semaglutide Therapy: Navigating Complex Comorbidities and Polypharmacy Challenges
In clinical practice, patients eligible for semaglutide therapy often present with multifaceted health profiles that extend beyond simple obesity metrics. The interplay of comorbidities such as cardiovascular disease, chronic kidney disease, and psychiatric disorders necessitates a nuanced approach to semaglutide initiation and maintenance. Polypharmacy, common in these populations, raises concerns about drug–drug interactions, particularly with medications affecting gastrointestinal motility or glucose metabolism. Experienced clinicians must perform comprehensive medication reconciliation and collaborate across specialties to optimize therapeutic outcomes while minimizing adverse events.
Moreover, tailoring semaglutide regimens in elderly patients requires balancing efficacy with tolerability, as age-related changes in pharmacokinetics and pharmacodynamics may alter drug exposure and side effect profiles. This demographic often benefits from slower dose escalation and vigilant monitoring of hydration status and renal function to prevent complications.
What Strategies Ensure Safe Semaglutide Use in Patients with Complex Medical Histories?
Effective management begins with a thorough baseline assessment including cardiovascular risk stratification, glycemic control evaluation, and psychological readiness screening. Integrating semaglutide into a multidisciplinary framework—engaging endocrinologists, cardiologists, psychiatrists, and dietitians—supports individualized care plans. Protocols emphasizing gradual titration, patient education on side effect recognition, and prompt intervention underpin safety. For instance, addressing nausea proactively through dietary modifications and antiemetic adjuncts can enhance adherence. Continual reassessment through validated patient-reported outcome measures helps detect subtle intolerance or emerging contraindications, ensuring dynamic adjustments to therapy.
Emerging evidence also suggests that genetic polymorphisms affecting GLP-1 receptor sensitivity might influence individual response variability, hinting at future precision medicine paradigms in semaglutide therapy (Diabetes Care, 2021).
Advancing Weight Loss Maintenance: The Role of Semaglutide in Long-Term Metabolic Reset and Behavioral Adaptation
While semaglutide’s acute effects on appetite suppression and glycemic regulation are well documented, its potential in long-term weight loss maintenance is gaining significant attention. Chronic obesity is increasingly conceptualized as a relapsing condition necessitating sustained intervention rather than finite treatment. Semaglutide’s capacity to recalibrate central appetite circuits may facilitate a metabolic reset that supports enduring behavioral changes.
Nonetheless, weight regain remains a persistent challenge after discontinuation. Integrating semaglutide with structured behavioral programs that reinforce mindful eating, stress management, and physical activity is critical to cement lifestyle changes. Continuous low-dose semaglutide maintenance therapy is under investigation to determine optimal duration and dosing that balance efficacy with safety.
Healthcare providers must also address psychological factors—such as reward sensitivity and executive function deficits—that undermine sustained weight control. Incorporating cognitive-behavioral therapy and motivational enhancement alongside pharmacotherapy leverages neuroplasticity to consolidate new habits.
How Does Semaglutide Influence Neurobehavioral Mechanisms Underpinning Weight Loss Maintenance?
Semaglutide’s GLP-1 receptor agonism extends beyond peripheral metabolic effects; it modulates reward pathways in the mesolimbic system, reducing hedonic eating drives and cravings. Neuroimaging studies reveal attenuated activation of the nucleus accumbens during food cue exposure following semaglutide treatment, suggesting a direct impact on food motivation circuits (Neuropsychopharmacology, 2021). Understanding these mechanisms enables clinicians to anticipate behavioral responses and tailor adjunctive therapies accordingly, enhancing long-term success.
Integrating Digital Health Innovations: Enhancing Semaglutide Therapy Through Remote Monitoring and AI-Driven Personalization
The advent of digital health tools presents unprecedented opportunities to refine semaglutide-based weight loss programs. Remote patient monitoring platforms enable continuous tracking of weight trends, glycemic indices, and side effect profiles, facilitating timely clinical interventions. Artificial intelligence algorithms can analyze these data streams to predict adherence risks and recommend personalized adjustments in dosing or lifestyle modifications.
Such technology empowers patients through real-time feedback and fosters a collaborative therapeutic alliance. Moreover, virtual coaching and telemedicine consultations mitigate geographical barriers, expanding access to expert-guided semaglutide care. Ongoing trials are exploring the integration of wearable biosensors and behavioral analytics to optimize dosing schedules and maximize metabolic benefits.
Call to Action: Deepen Expertise and Collaborate on Cutting-Edge Semaglutide Protocols
Clinicians and researchers committed to advancing obesity therapeutics are encouraged to engage with specialized forums and subscribe to emerging literature, including the latest clinical guidelines and translational research findings. Explore comprehensive resources and case studies at Medical Weight Loss Programs Unlocking Success With Semaglutide to stay at the forefront of evidence-based practice. Sharing your clinical experiences and innovative strategies will contribute to the collective expertise necessary to optimize patient-centered outcomes in this dynamic field.
Precision Titration Protocols: Navigating Complex Patient Profiles with Semaglutide
Advanced semaglutide administration demands meticulous customization of dosing regimens tailored to the patient’s multifactorial clinical context. For individuals presenting with polypharmacy and multimorbidity, clinicians must adopt a phased titration strategy, integrating pharmacokinetic monitoring and vigilant adverse effect surveillance. This approach mitigates risks of gastrointestinal intolerance and hypoglycemia, especially in patients with compromised renal or hepatic function. Employing comprehensive medication reconciliation tools enhances detection of potential drug–drug interactions, reinforcing safety in complex care environments.
Harnessing Pharmacogenomics: Toward Personalized Semaglutide Responsiveness
Emerging pharmacogenomic data elucidate how genetic polymorphisms in GLP-1 receptor pathways modulate individual responsiveness to semaglutide. Variants influencing receptor affinity and downstream signaling cascades may predict differential weight loss outcomes and side effect profiles. Integrating genotypic screening into clinical workflows could refine candidate selection and optimize therapeutic efficacy, heralding a new era of precision obesity pharmacotherapy. This paradigm aligns with precision medicine principles, emphasizing tailored interventions based on individual molecular characteristics.
What Are the Latest Evidence-Based Approaches to Mitigate Semaglutide-Induced Gastrointestinal Adverse Effects?
Gastrointestinal side effects remain the primary limitation in semaglutide therapy adherence. Innovative mitigation strategies include dose fractionation, co-administration of prokinetic agents, and structured dietary modifications emphasizing low-residue, small frequent meals. Recent randomized trials have also evaluated adjunctive antiemetic protocols that significantly reduce nausea and vomiting incidence without compromising weight loss efficacy. Patient education on anticipatory symptom management and real-time symptom tracking through digital platforms further enhances tolerability and persistence.
Integrating Advanced Digital Biomarkers: AI-Powered Monitoring for Dynamic Dose Adjustments
Cutting-edge digital health technologies now enable real-time assessment of patient-specific responses via biosensors capturing physiological and behavioral biomarkers. Machine learning algorithms analyze patterns pertaining to appetite fluctuations, glycemic variability, and side effect emergence, facilitating preemptive dose modulation. This AI-driven personalization not only improves safety profiles but also maximizes therapeutic outcomes by dynamically aligning semaglutide dosing with patient metabolic status and lifestyle factors.
Authoritative External Reference: The Lancet’s Semaglutide Pharmacogenomics Review (2023)
For an in-depth examination of genetic determinants influencing semaglutide response, consult the comprehensive review published in The Lancet Diabetes & Endocrinology (2023). This article synthesizes current evidence on GLP-1 receptor variants and their clinical implications, providing a robust framework for integrating pharmacogenomics into obesity therapeutics.
Call to Action: Elevate Your Clinical Practice with Cutting-Edge Semaglutide Insights
Healthcare professionals dedicated to mastering semaglutide therapy’s nuances are invited to explore advanced protocol frameworks and participate in expert forums at Medical Weight Loss Programs Unlocking Success With Semaglutide. Engage with peer-reviewed case studies, share clinical experiences, and access emerging research to refine your approach and optimize patient outcomes in this rapidly evolving therapeutic domain.
Expert Insights & Advanced Considerations
1. Precision Titration is Essential for Maximizing Therapeutic Outcomes
Individualized dose escalation protocols that consider patient comorbidities, polypharmacy, and tolerability thresholds greatly enhance semaglutide’s safety and efficacy profile. Gradual titration minimizes gastrointestinal adverse effects, preserves patient adherence, and allows dynamic dose adjustments based on real-time clinical feedback, as detailed in doctor-supervised semaglutide safe dosage guidelines.
2. Integration of Semaglutide with Behavioral and Nutritional Therapies Amplifies Long-Term Success
Pharmacological appetite suppression synergizes with evidence-based dietary frameworks and cognitive-behavioral interventions to address neurobehavioral drivers of obesity. This multimodal approach fosters sustainable lifestyle changes that extend beyond the pharmacodynamic window of semaglutide, as explored in guide to crafting the best semaglutide diet plans for fat loss.
3. Pharmacogenomic Profiling Promises to Revolutionize Personalized Semaglutide Therapy
Emerging evidence on GLP-1 receptor polymorphisms suggests that genotypic screening could predict response variability and side effect susceptibility. This precision medicine angle heralds a future where semaglutide regimens are tailored not merely by clinical phenotype but by molecular signatures, enhancing both safety and efficacy (The Lancet Diabetes & Endocrinology, 2023).
4. Digital Health Innovations Enhance Monitoring and Personalized Dose Optimization
AI-driven platforms and biosensors enable continuous tracking of metabolic markers, appetite fluctuations, and side effect profiles. This data-driven approach facilitates preemptive dose adjustments and adherence support, expanding access through telemedicine and virtual coaching, thereby optimizing semaglutide’s clinical impact.
Curated Expert Resources
- Journal of the American Medical Association (JAMA): Provides rigorous clinical trial data validating semaglutide’s efficacy and safety in diverse populations (Semaglutide Weight Loss Trial).
- The Lancet Diabetes & Endocrinology (2023) Pharmacogenomics Review: Deep dive into genetic determinants influencing semaglutide response, essential for clinicians exploring precision therapeutics (Full Article).
- BestFastWeightLossDiets.com Medical Weight Loss Programs: Comprehensive guides on semaglutide dosing, dietary integration, and patient monitoring protocols (Unlocking Success With Semaglutide).
- Digital Health and AI in Obesity Management: Emerging literature on leveraging technology for personalized semaglutide therapy and adherence enhancement.
- Clinical Practice Guidelines on GLP-1 Receptor Agonists: Authoritative recommendations on safety, dosing, and patient selection criteria for semaglutide in obesity treatment.
Final Expert Perspective
Semaglutide’s transformative potential in medical weight loss programs lies not only in its robust pharmacodynamics but also in the strategic integration of precision dosing, behavioral support, and emerging technologies. Mastery of these dimensions empowers clinicians to deliver personalized, sustainable obesity care that transcends conventional treatment paradigms. By engaging with advanced resources and adopting a multidisciplinary approach, healthcare professionals can optimize semaglutide’s efficacy and safety, ultimately improving patient outcomes. For clinicians eager to deepen their expertise, exploring Medical Weight Loss Programs Unlocking Success With Semaglutide offers invaluable insights and collaborative opportunities to refine practice in this dynamic therapeutic landscape.


The article’s emphasis on integrating semaglutide within a comprehensive medical weight loss program really resonates with me. From my understanding, semaglutide’s role in modulating appetite through GLP-1 receptor agonism is a game-changer, but what intrigues me most is how this effect is enhanced when paired with nutritional guidance and behavioral therapy. I’ve read that gradual dose titration is crucial to managing side effects like nausea, ensuring patients stick to the regimen comfortably. This integrative approach seems to tackle obesity not just pharmacologically but holistically, addressing metabolic, psychological, and lifestyle factors simultaneously.
In my experience, weight loss isn’t just about the medication or diet alone but how these elements support sustainable habits. The challenge, as the article points out, lies in personalizing therapy—factoring in comorbidities, prior weight loss attempts, and readiness to change. It makes me wonder how clinicians balance these variables in busy clinical settings and to what extent digital health tools facilitate this personalization.
Has anyone here experienced or observed how remote monitoring or AI-driven adjustments impact patient adherence and long-term outcomes with semaglutide? I’m curious if these technologies can bridge gaps in care access and provide more timely interventions to minimize side effects and optimize dosing.
Reading through the post, I was particularly struck by the emphasis on comprehensive patient monitoring within multidisciplinary programs. In my practice, I’ve observed that integrating tools like digital platforms for remote monitoring can significantly enhance adherence, especially for patients who might be hesitant or struggle with in-clinic visits. For example, real-time data on side effects and weight progress allows us to make timely adjustments to dosing schedules, which seems aligned with the article’s emphasis on safety and personalization. While some clinicians worry about the reliability of remote data, I believe that with proper calibration and patient education, these tools can be invaluable.
However, I wonder about the scalability of such systems in resource-limited settings. Do others think that AI-driven dose adjustments could be feasibly implemented on a larger scale, perhaps in primary care? Also, how do we ensure that patient engagement remains high when relying heavily on digital monitoring? It feels like the future of semaglutide integration relies heavily on technology, but balancing that with human touch is still critical.
I find the comprehensive approach outlined in the post really compelling, especially how integrating semaglutide into multidisciplinary programs enhances not just weight loss but overall metabolic health. Personally, in my clinic, we’ve seen remarkable improvements when combining pharmacotherapy with behavioral counseling and nutritional guidance. The key seems to be careful patient selection and close monitoring, particularly when titrating doses to minimize side effects.
Regarding digital health tools, I’ve noticed that remote monitoring and AI algorithms can indeed boost adherence and provide timely intervention points. However, I wonder how practical it is to implement these technologies on a large scale, especially in less resource-rich settings. Do others have insights or experiences on balancing the benefits of high-tech monitoring with accessibility? Also, what strategies have you found effective in motivating patients to stay engaged with these digital tools over the long term? I believe that fostering a patient-centered, tech-savvy environment could truly revolutionize obesity management.