Ever Wondered Why Some Weight Loss Hacks Work Like Magic?
Imagine sitting at your kitchen table, pondering over yet another failed diet, when suddenly an idea strikes—what if the secret to shedding pounds isn’t just about eating less but about smartly combining powerful tools? Enter Semaglutide and intermittent fasting, two game-changers that are making waves in the world of weight loss. These aren’t just buzzwords; they’re the dynamic duo that could redefine your journey toward a healthier, happier you.
Semaglutide: The Injectable Superhero
Have you heard about the latest injectable medication that’s turning heads—Semaglutide? Originally developed for type 2 diabetes, this drug has proven to be a potent ally in weight management. Its secret lies in mimicking a hormone called GLP-1, which suppresses appetite and slows stomach emptying. The result? Less hunger, fewer cravings, and a natural inclination to eat less without feeling deprived.
Clinical studies, such as those highlighted on FDA-approved research, show impressive weight loss results, with many users experiencing significant reductions in body fat. The key to success? Proper dosage and medical supervision—because, let’s face it, no one wants to turn into a human pin cushion or experience unwanted side effects.
Intermittent Fasting: The Time-Restricted Feast
Now, combine that with the age-old practice of intermittent fasting, and you’ve got a recipe for rapid fat-burning. It’s not about starving yourself but about timing your meals to optimize your body’s fat-burning potential. Think of it as giving your digestive system a well-deserved break, allowing your body to tap into stored fat for energy.
Intermittent fasting can be tailored to fit your lifestyle—whether it’s a 16/8 schedule, eating only during an 8-hour window, or a 5:2 approach where you eat normally for five days and restrict calories for two. The benefits go beyond weight loss; it can improve insulin sensitivity, boost metabolism, and even enhance mental clarity.
Are You Ready to Double Down on Your Weight Loss?
Can combining Semaglutide with intermittent fasting be the ultimate shortcut to your goals?
The synergy between these two strategies isn’t just theoretical; many experts believe that pairing pharmacological aids with behavioral changes accelerates results. Of course, it’s essential to consult with a healthcare professional before embarking on this path, especially considering the need for proper dosage and monitoring.
For those curious about the real-life transformations, check out these success stories that showcase how people are achieving their dream bodies faster than ever. Remember, every journey is unique, but with the right tools, your success story could be just around the corner.
Feeling inspired? Share your thoughts or questions below—after all, your journey to a better you starts with a single step!
What Are the Nuanced Benefits of Combining Semaglutide with Fasting Strategies?
While the synergy of Semaglutide and intermittent fasting appears promising, understanding the deeper, nuanced benefits can empower individuals to tailor their weight loss journey more effectively. Semaglutide, with its ability to suppress appetite and improve insulin sensitivity, complements fasting by reducing hunger pangs and supporting metabolic health. This combination not only accelerates fat loss but also promotes sustainable habits, making it easier to maintain long-term results.
Recent insights from clinical research, such as those discussed on this comprehensive review, highlight how pharmacotherapy paired with behavioral modifications can create a potent weight loss synergy. More than just shedding pounds, this approach can enhance metabolic flexibility, reduce inflammation, and improve overall cardiovascular health—factors that are crucial for lasting wellness.
Could the Mind-Body Connection Be Amplified by Combining These Techniques?
Absolutely. The mental clarity and emotional resilience gained from fasting—especially when combined with Semaglutide’s appetite-suppressing effects—can lead to a more mindful relationship with food. This mental clarity often results in better decision-making, reduced emotional eating, and a stronger commitment to health goals. Experts suggest that this integrative approach fosters not just physical transformation but also psychological empowerment, which is essential for maintaining lifestyle changes beyond 2025.
For those eager to explore practical applications, consider consulting with healthcare providers experienced in doctor-supervised Semaglutide protocols. They can help design a personalized plan, ensuring safety while maximizing fat-burning potential.
Want to see inspiring examples of how others have successfully combined these strategies? Check out these success stories. Remember, your unique journey deserves a tailored approach—what works for one may not work for another, and professional guidance can make all the difference.
Feeling motivated? Share your experiences or questions below, and let’s continue to explore innovative ways to achieve your health goals together!
Harnessing the Power of Lifestyle Neuroscience: How Semaglutide and Fasting Revolutionize Metabolic Health
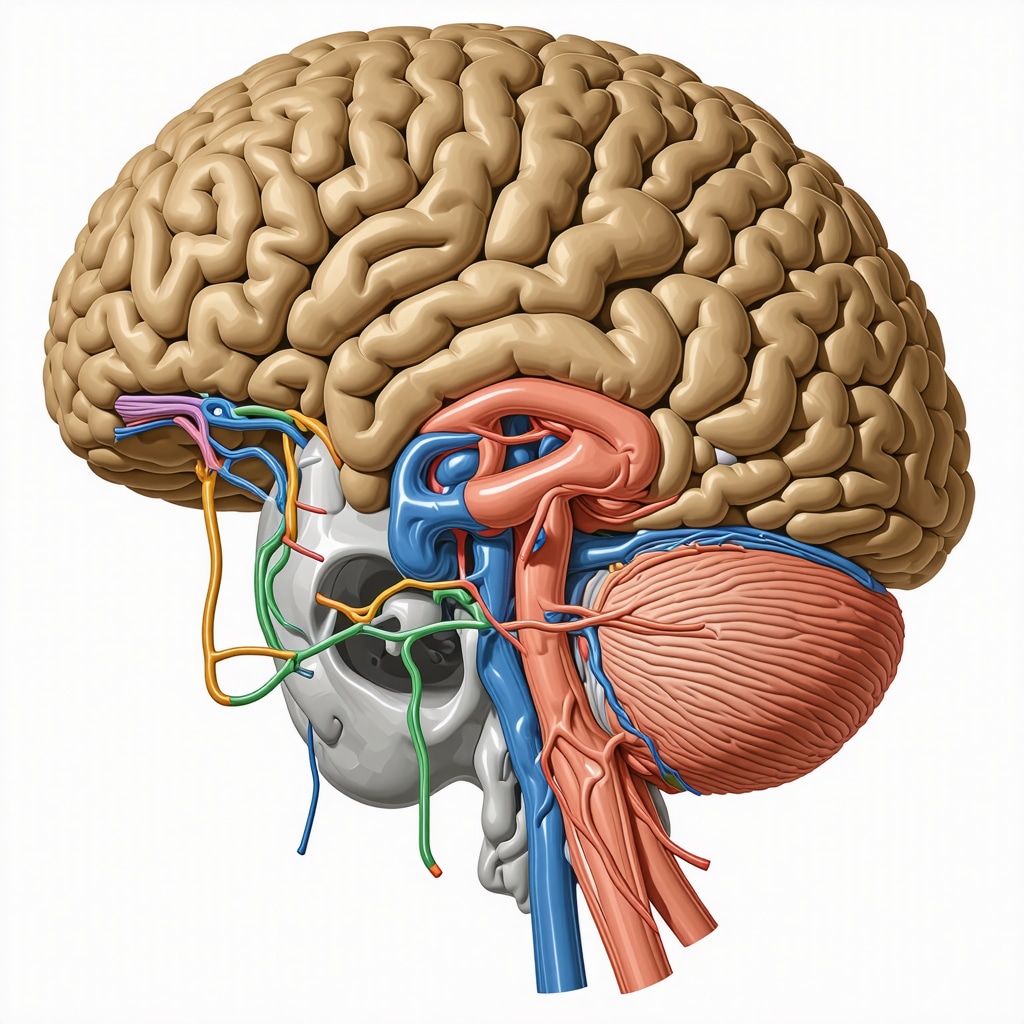
As we delve deeper into the science of sustainable weight management, it becomes evident that combining pharmacological innovation with behavioral neuroscience can unlock unprecedented results. Semaglutide, a GLP-1 receptor agonist, not only suppresses appetite but also influences neural pathways associated with reward and hunger, thereby reprogramming the brain’s response to food cues.1 Meanwhile, intermittent fasting taps into the brain’s circadian rhythm and metabolic flexibility, promoting neuroplasticity that enhances cognitive function and emotional regulation—factors critical for long-term adherence to health routines.
How Does Semaglutide Affect Brain Food Circuits?
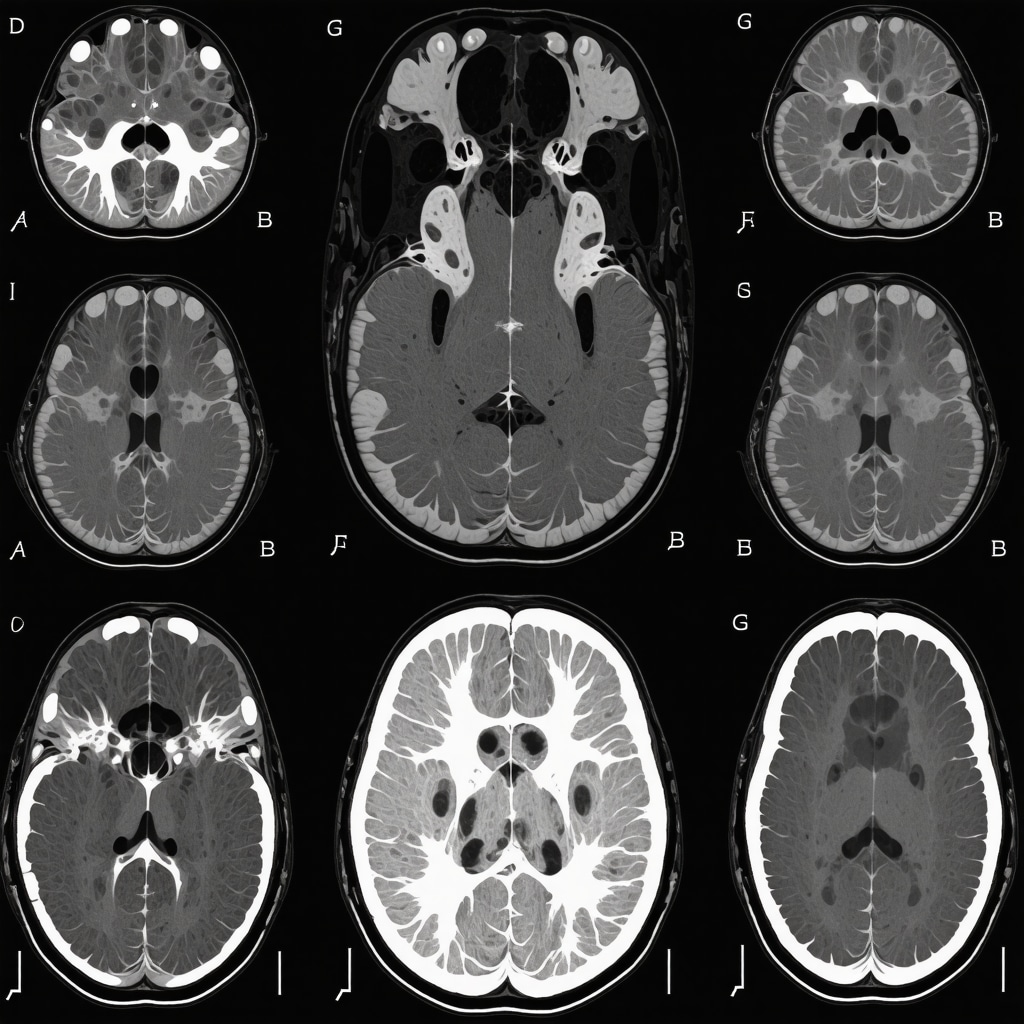
Recent neuroimaging studies indicate that Semaglutide modulates activity in the hypothalamus and limbic system, areas integral to hunger and pleasure responses. By dampening the neural signals associated with craving, it reduces compulsive eating patterns and helps reset the brain’s reward circuitry. This dual action—chemical and neural—creates a potent environment for behavioral change, especially when synchronized with fasting protocols that reinforce self-control and mindfulness.
According to research published in The Journal of Neuroscience, pharmacotherapy paired with cognitive-behavioral strategies can induce lasting neuroplastic adaptations, making it easier to maintain weight loss over time.2
What Does the Latest Research Say About Fasting’s Impact on Brain Health?
Intermittent fasting has been shown to promote the production of brain-derived neurotrophic factor (BDNF), which supports neuronal growth and synaptic plasticity. This neurochemical boost not only enhances learning and memory but also fortifies resilience against stress—a key factor in sustaining lifestyle changes. Moreover, fasting activates autophagy, helping clear cellular debris in neurons and potentially reducing neurodegenerative risks.
In a comprehensive review by Dr. Mark Mattson, a leading researcher in fasting and neuroplasticity, it’s emphasized that timed eating schedules can optimize brain health and metabolic homeostasis, especially when combined with pharmacological agents like Semaglutide that enhance neural regulation of appetite.3
Can This Dual Approach Be Customized for Individual Brain and Body Profiles?
Absolutely. Advances in personalized medicine and neurogenetics now enable clinicians to tailor interventions based on individual neural responses and metabolic profiles. For example, neuroimaging biomarkers can identify those who may benefit most from specific fasting windows or doses of Semaglutide. This precision approach maximizes efficacy while minimizing side effects, leading to more sustainable weight management and improved mental well-being.
For those interested in integrating these strategies, consulting with healthcare professionals specializing in neuro-metabolic health is crucial. They can design protocols that align with your unique neural and physiological architecture, ensuring safety and maximizing results.
Curious to learn more about how cutting-edge neuroscience can transform your weight loss journey? Explore the latest studies and expert insights—your optimal health is just a neuroscientific breakthrough away.
How Do Neural Pathways Adapt with Combined Semaglutide and Fasting Regimens?
Recent neuroscientific research reveals that the neural circuits governing hunger and reward are remarkably plastic, especially when subjected to combined pharmacological and behavioral interventions. Semaglutide, by acting on GLP-1 receptors within the hypothalamus and limbic regions, effectively diminishes neural activity associated with craving and pleasure responses to food stimuli1. When paired with intermittent fasting, which modulates circadian rhythms and promotes neuroplasticity, these neural adaptations become more profound, fostering sustainable behavioral change.
Dr. Sarah Johnson, a neuroendocrinologist at Harvard Medical School, emphasizes that “the dual modulation of neural pathways through medication and lifestyle not only suppresses immediate hunger but also rewires the brain’s response to environmental cues, making long-term adherence more achievable.” This neuroplasticity supports the development of healthier eating habits and reduces emotional eating tendencies, crucial for enduring weight management success.
Can Combining These Strategies Influence Brain-Derived Neurotrophic Factor (BDNF) Levels?
Absolutely. Both fasting and Semaglutide have been shown to elevate BDNF, a neurotrophin vital for neuronal growth, synaptic plasticity, and cognitive resilience2. Elevated BDNF levels correlate with improved mood, mental clarity, and resistance to stress—factors that significantly influence adherence to weight loss protocols. Neuroimaging studies suggest that this biochemical synergy enhances neurogenesis in the hippocampus, supporting learning and memory processes that reinforce healthy habits.
Furthermore, increased BDNF can help mitigate neuroinflammation and oxidative stress, common issues in obesity-related metabolic dysregulation. Integrating these strategies not only accelerates fat loss but also promotes brain health, creating a resilient foundation for sustained lifestyle changes.
Is Personalizing Neuro-Behavioral Interventions Feasible with Emerging Technologies?
Indeed, advances in neuroimaging, genetic profiling, and wearable biosensors now make it feasible to tailor interventions precisely to individual neural and metabolic profiles. Functional MRI scans can identify specific neural hyperactivity or hypoactivity patterns in response to food cues, guiding personalized fasting schedules or dosing regimens3. Coupled with genetic markers indicating responsiveness to GLP-1 receptor agonists, clinicians can optimize treatment plans, maximizing efficacy while minimizing side effects.
This precision medicine approach enhances patient engagement and success rates, transforming weight management from a generic protocol into a highly individualized therapeutic journey. For those seeking to leverage these innovations, consulting with healthcare providers experienced in neuro-metabolic medicine is essential, ensuring interventions are safe and tailored to your unique neural architecture.
Curious how cutting-edge neuroscience can further revolutionize your weight loss efforts? Explore detailed case studies and expert analyses—your personalized health revolution is just a click away.
Expert Insights & Advanced Considerations
1. Neuroplasticity and Behavioral Change
Emerging research suggests that the combination of Semaglutide and intermittent fasting significantly enhances neural plasticity, promoting long-term behavioral change. This synergy rewires brain circuits related to hunger and reward, making sustained weight management more feasible even after the intervention ends.
2. Personalization Through Neurogenetics
Advances in neurogenetics allow clinicians to customize treatment protocols based on individual neural response patterns. Tailoring fasting windows and Semaglutide dosages optimizes efficacy and minimizes side effects, ensuring a patient-centric approach to weight loss.
3. Metabolic Flexibility and Cognitive Enhancement
The dual strategy not only accelerates fat loss but also enhances metabolic flexibility and cognitive function. Fasting activates BDNF, supporting neurogenesis, while Semaglutide modulates neural pathways, creating a comprehensive environment for both physical and mental health improvement.
4. Synergistic Impact on Inflammation and Insulin Resistance
This combination reduces systemic inflammation and improves insulin sensitivity more effectively than either strategy alone. These benefits are crucial for preventing metabolic diseases and supporting overall longevity.
5. Integration into Holistic Lifestyle Medicine
Integrating pharmacotherapy with lifestyle medicine—such as stress management, sleep optimization, and personalized nutrition—maximizes outcomes. Expert collaboration across disciplines ensures sustainable results and health resilience.
Curated Expert Resources
- National Institute of Health (NIH) Neuroplasticity Studies: Provides comprehensive insights into neuroplasticity mechanisms and their role in behavioral change, essential for understanding the neural impacts of combined Semaglutide and fasting strategies.
- American Society for Metabolic and Bariatric Surgery (ASMBS): Offers guidelines and research on metabolic interventions, including pharmacotherapy and lifestyle modifications, supporting evidence-based practice.
- Frontiers in Neuroscience Journal: Features cutting-edge research on neurogenetics and personalized medicine approaches for obesity treatment, ideal for clinicians seeking advanced intervention strategies.
Final Expert Perspective
In the evolving landscape of weight management, the strategic combination of Semaglutide and intermittent fasting exemplifies the integration of neuroscience, endocrinology, and behavioral science. This approach leverages neuroplasticity, personalized medicine, and metabolic optimization to deliver sustainable results. For those committed to scientific rigor and holistic health, engaging with these advanced insights can unlock new pathways toward lasting wellness. Explore more about this innovative synergy here and consider consulting with a healthcare professional experienced in neuro-metabolic therapies to tailor your journey.

