Understanding Semaglutide’s Dominance in FDA Approved Weight Loss Medications
The landscape of FDA approved weight loss drugs has evolved significantly with the introduction of semaglutide, a glucagon-like peptide-1 (GLP-1) receptor agonist originally developed for type 2 diabetes management. Semaglutide’s superior efficacy in inducing sustained weight loss has positioned it as a market leader, reshaping therapeutic strategies for obesity treatment. Its dual action—enhancing satiety and reducing appetite—offers a pharmacological advantage that surpasses many traditional weight loss agents.
The Pharmacodynamics and Clinical Advantages of Semaglutide over Other FDA Approved Drugs
Semaglutide’s molecular design enables prolonged receptor activation, resulting in significant reductions in caloric intake and enhanced energy expenditure. Clinical trials published in the New England Journal of Medicine demonstrate weight loss averaging 15-20% of body weight, a magnitude rarely achieved by other FDA approved drugs such as orlistat or phentermine-topiramate. Moreover, semaglutide’s once-weekly injectable formulation improves patient adherence compared to oral regimens.
Exploring the Nuanced Safety Profile and Patient Selection Criteria for Semaglutide Use
While semaglutide showcases a favorable safety profile, including gastrointestinal discomfort as the most common adverse effect, its use requires careful patient selection, especially considering contraindications like personal or family history of medullary thyroid carcinoma. The expert consensus emphasizes the importance of a multidisciplinary approach to dosage titration and monitoring, ensuring maximal therapeutic benefits with minimal risk.
What Are the Challenges in Integrating Semaglutide into Comprehensive Obesity Management Protocols?
Despite its clinical efficacy, integrating semaglutide into broader obesity treatment regimens presents challenges including cost barriers, insurance coverage variability, and the necessity for patient education on injection techniques and lifestyle modifications. There is also ongoing discourse among endocrinologists regarding long-term outcomes and the potential need for combination therapies to optimize sustained weight loss.
Leveraging Semaglutide in Combination with Lifestyle Interventions for Enhanced Outcomes
Emerging evidence suggests that coupling semaglutide therapy with structured lifestyle interventions—such as tailored dietary plans and intermittent fasting—can synergistically amplify fat loss and metabolic improvements. Medical weight loss programs increasingly incorporate semaglutide alongside behavioral counseling to maximize patient success rates, a strategy supported by longitudinal studies indicating improved weight maintenance.
For clinicians and researchers seeking to deepen their understanding of semaglutide’s role in obesity treatment, exploring detailed clinical insights and injection guidelines can be invaluable. Comprehensive resources like FDA Approved Semaglutide Clinical Insights provide authoritative guidance for maximizing therapeutic outcomes.
Explore further expert-level content and share your professional experiences with semaglutide in our community forum at Contact Us to advance collective knowledge in this rapidly evolving field.
Optimizing Semaglutide Therapy Through Personalized Dosing and Patient Monitoring
Achieving maximal efficacy with semaglutide requires an individualized approach to dosing and vigilant patient monitoring. Clinicians emphasize gradual dose escalation, typically starting at 0.25 mg weekly and titrating up to 2.4 mg, to enhance tolerability and minimize gastrointestinal side effects. Monitoring parameters should include glycemic control, gastrointestinal tolerance, and psychological well-being, as mood alterations have been reported in some patients. This tailored strategy aligns with recommendations detailed in the doctor supervised semaglutide safe dosage guidelines, ensuring safety while promoting sustained fat loss.
Integrating Semaglutide with Nutritional Strategies: Beyond Calorie Restriction
Recent clinical insights advocate for combining semaglutide with advanced nutritional paradigms beyond mere calorie limitation. Low-carbohydrate and Mediterranean-style diets have demonstrated potential in synergizing with semaglutide’s appetite suppression, optimizing metabolic outcomes. Furthermore, intermittent fasting protocols can enhance fat oxidation rates and insulin sensitivity when paired with semaglutide, creating a potent one-two punch against obesity. For a comprehensive understanding of such combinatory approaches, see Semaglutide and Intermittent Fasting: A Strategic Weight Loss Duo for 2025.
How Can Emerging Biomarkers Guide Tailored Semaglutide Treatment Plans?
Advancements in biomarker research hold promise for refining semaglutide therapy personalization. Biomarkers such as fasting insulin levels, gut microbiota composition, and genetic polymorphisms related to GLP-1 receptor sensitivity could predict individual responsiveness and risk of adverse effects. Incorporating these biomarkers into clinical algorithms may optimize patient selection, dosing schedules, and adjunctive interventions, thereby enhancing efficacy and safety. Ongoing studies published in authoritative journals like Diabetes Care underscore the critical role of these biomarkers in future obesity pharmacotherapy (Diabetes Care, 2022).
Addressing Real-World Barriers: Accessibility, Cost, and Long-Term Adherence
Despite semaglutide’s transformative potential, real-world implementation faces hurdles including high cost, insurance limitations, and patient adherence challenges. Solutions involve advocating for policy changes to improve coverage, developing patient education platforms focused on injection techniques and lifestyle integration, and leveraging telemedicine for continuous support. Exploring structured medical weight loss programs that incorporate semaglutide can also facilitate adherence and optimize outcomes; see Medical Weight Loss Programs Using Semaglutide That Work Fast for actionable frameworks.
We invite healthcare professionals and researchers to share insights or case studies on semaglutide implementation challenges and successes in our community forum via Contact Us. Collaboratively, we can advance best practices and patient outcomes in this dynamic therapeutic area.
Harnessing Pharmacogenomics: Precision Medicine for Semaglutide Optimization
In the quest to maximize semaglutide’s therapeutic potential, pharmacogenomics emerges as a frontier for individualized obesity treatment. Genetic polymorphisms within the GLP-1 receptor gene and downstream signaling pathways can significantly influence pharmacodynamics and patient response. For instance, variants affecting receptor expression or signaling efficiency might predict differential weight loss outcomes or susceptibility to adverse effects. By integrating comprehensive genomic profiling into clinical workflows, practitioners can tailor semaglutide dosing regimens with unprecedented precision, reducing trial-and-error approaches and enhancing safety.
This paradigm shift toward precision medicine is supported by burgeoning evidence highlighting genotype-phenotype correlations in GLP-1 receptor agonist responsiveness. As noted in a recent Nature Medicine review, incorporating genetic markers into therapeutic decision-making frameworks could revolutionize obesity pharmacotherapy (Nature Medicine, 2023).
Mitigating Gastrointestinal Side Effects: Advanced Strategies for Enhancing Patient Tolerability
Gastrointestinal adverse events, particularly nausea and vomiting, remain the principal challenges in semaglutide adherence. Innovative mitigation techniques involve both pharmacologic and non-pharmacologic interventions. Gradual dose escalation protocols remain fundamental, yet adjunctive measures such as co-administration of antiemetic agents or prokinetic drugs are being explored to further improve tolerability. Additionally, dietary modifications emphasizing small, frequent meals rich in low-fat, low-fiber foods can attenuate gastrointestinal discomfort.
Emerging research also investigates the role of gut-brain axis modulation via probiotics and microbiome-targeted therapies to alleviate adverse effects. Such approaches aim to recalibrate gut motility and sensitivity, thereby enhancing the patient’s ability to continue therapy uninterrupted.
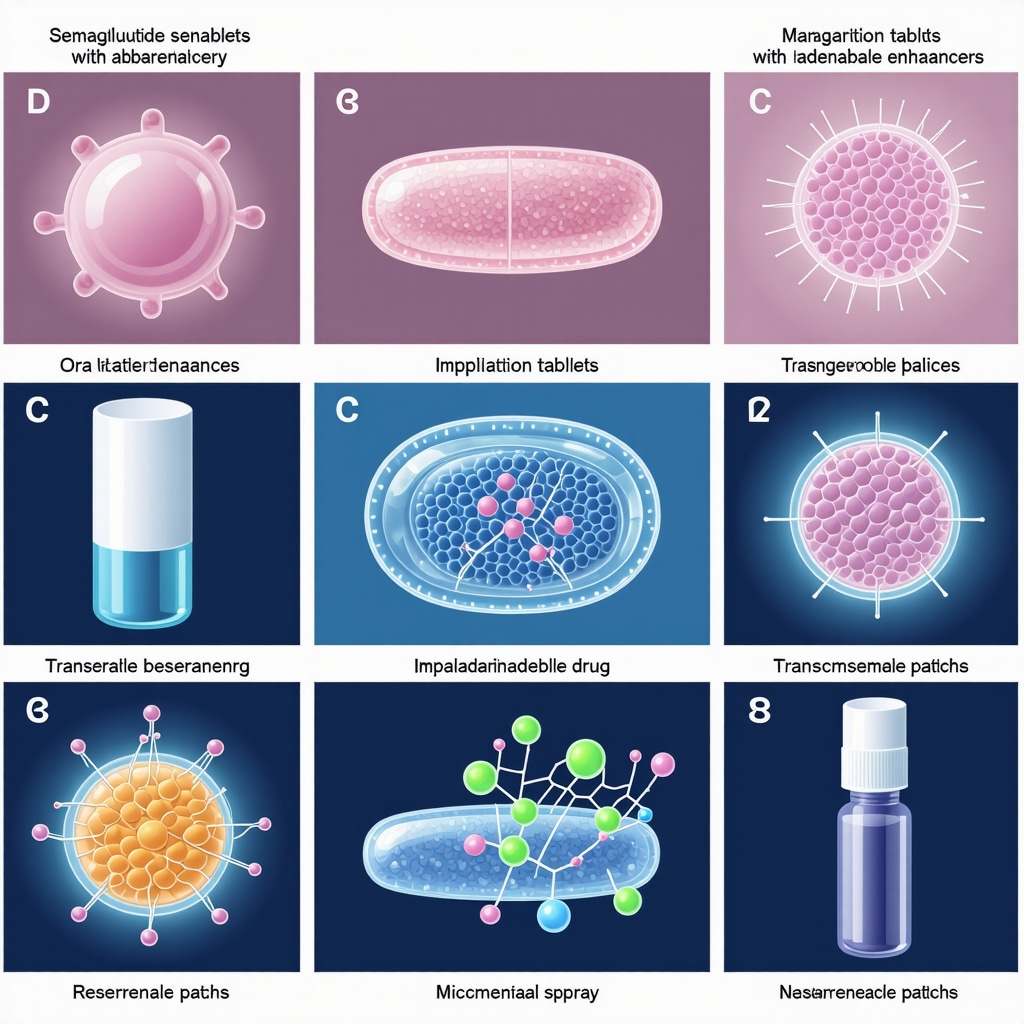
What Are the Latest Innovations in Semaglutide Delivery Systems to Improve Patient Compliance?
While once-weekly subcutaneous injections are standard, novel delivery modalities are under clinical evaluation to enhance convenience and adherence. These include oral semaglutide formulations utilizing absorption enhancers to overcome gastrointestinal barriers, as well as implantable devices providing sustained release over months. Transdermal patches and nasal sprays are also in early-stage development, aiming to reduce injection-associated anxiety and expand patient acceptance.
These innovations promise to broaden semaglutide’s accessibility and improve quality of life for patients requiring long-term obesity management, signaling a transformative evolution in drug delivery technology.
Integrating Semaglutide into Multimodal Obesity Treatment Ecosystems: Beyond Pharmacotherapy
Recognizing obesity as a multifactorial disease, comprehensive management increasingly involves integrating semaglutide with behavioral therapy, surgical interventions, and digital health tools. Multidisciplinary care teams encompassing endocrinologists, dietitians, psychologists, and exercise physiologists facilitate holistic treatment plans. Digital platforms leveraging artificial intelligence-driven coaching and remote monitoring enable real-time adjustment of semaglutide dosing and lifestyle recommendations, fostering sustainable weight loss.
Such ecosystems emphasize patient empowerment and continuous engagement, which are critical for long-term success. The convergence of pharmacological advances with digital therapeutics represents an exciting frontier for personalized, adaptive obesity care.
For clinicians and researchers eager to delve deeper into these emerging strategies and contribute to evolving best practices, we encourage active participation in our expert forums and continuous education modules available via Contact Us.
Pharmacogenomic Profiling: Unlocking Personalized Semaglutide Regimens
Recent strides in pharmacogenomics are enabling clinicians to transcend conventional dosing paradigms by integrating genetic insights to customize semaglutide therapy. Variants within the GLP-1 receptor gene (GLP1R), along with polymorphisms affecting downstream effectors like adenylate cyclase and protein kinase A, have been implicated in differential receptor sensitivity and intracellular signaling efficiency. Such genetic heterogeneity can profoundly influence both efficacy and tolerability profiles, necessitating genotype-guided titration strategies.
Implementing comprehensive genomic screening protocols prior to therapy initiation facilitates identification of patients likely to exhibit suboptimal response or heightened adverse event risk. This precision medicine approach promises to reduce attrition rates and optimize therapeutic windows. For an in-depth appraisal of genotype-phenotype correlations and clinical integration frameworks, refer to the authoritative Nature Medicine 2023 review on GLP-1 receptor pharmacogenomics.
Cutting-Edge Drug Delivery Systems: Enhancing Semaglutide Patient Compliance and Convenience
While subcutaneous injections remain the clinical gold standard, burgeoning delivery technologies aim to surmount patient adherence barriers by offering less invasive and more user-friendly administration routes. Oral semaglutide formulations leveraging absorption enhancers such as sodium N-(8-[2-hydroxybenzoyl] amino) caprylate (SNAC) have demonstrated bioavailability sufficient for therapeutic efficacy, albeit requiring fasting administration protocols to maximize absorption.
Beyond oral routes, implantable biodegradable reservoirs enabling steady semaglutide release over extended periods are progressing through clinical trials, promising to reduce injection frequency drastically. Moreover, transdermal patches employing microneedle arrays and nasal sprays with permeation enhancers are under exploratory phases, targeting improved patient experience and expanded candidacy among needle-phobic populations.
How Can Multimodal Digital Health Platforms Integrate with Semaglutide Therapy to Optimize Long-Term Weight Management?
The convergence of pharmacotherapy and digital health technologies offers unprecedented opportunities to individualize and dynamically adjust semaglutide treatment plans. AI-driven platforms can analyze real-time biometric data, dietary logs, and patient-reported outcomes to recommend dose modifications and lifestyle interventions aligned with evolving metabolic status. Integration of telemedicine facilitates continuous patient engagement, adherence monitoring, and psychosocial support, addressing multifactorial contributors to obesity.
Such digital ecosystems also enable the incorporation of behavioral economics principles, utilizing gamification and personalized feedback loops to enhance motivation and sustain lifestyle changes synergistic with semaglutide’s pharmacodynamics. This holistic approach, supported by emerging evidence in obesity management literature, represents the next frontier in comprehensive care.
Healthcare providers and researchers are encouraged to engage with these advanced insights and contribute to the evolving dialogue by visiting our expert community through Contact Us, fostering innovation and excellence in obesity therapeutics.
Expert Insights & Advanced Considerations
Pharmacogenomic Profiling as a Game-Changer in Semaglutide Personalization
The integration of pharmacogenomics into semaglutide therapy heralds a paradigm shift from standardized dosing to precision medicine. Genetic variants in the GLP-1 receptor and downstream signaling pathways can dictate individual responsiveness and adverse effect profiles, enabling clinicians to tailor titration protocols and optimize therapeutic efficacy while minimizing risks. This approach reduces trial-and-error and enhances patient adherence.
Emerging Drug Delivery Innovations to Improve Patient Compliance
While weekly subcutaneous injections remain the standard, novel delivery systems such as oral formulations enhanced with absorption facilitators, implantable biodegradable reservoirs, transdermal microneedle patches, and nasal sprays promise to mitigate injection-associated barriers. These advancements will expand patient accessibility, improve quality of life, and potentially broaden semaglutide candidacy among individuals reluctant to use injectable therapies.
Multimodal Digital Health Ecosystems Amplifying Semaglutide’s Impact
AI-driven digital platforms that integrate real-time biometric data, behavioral analytics, and telemedicine enable dynamic customization of semaglutide treatment plans. These systems enhance patient engagement through personalized feedback, gamification, and continuous psychosocial support, addressing the multifactorial nature of obesity and reinforcing sustainable lifestyle changes synergistic with pharmacotherapy.
Strategic Integration with Nutritional and Lifestyle Interventions
Combining semaglutide with tailored dietary approaches—such as Mediterranean diets, low-carbohydrate regimens, and intermittent fasting—maximizes metabolic benefits and fat oxidation. Structured lifestyle modifications complement semaglutide’s appetite suppression mechanisms, fostering more substantial and enduring weight loss outcomes within comprehensive medical weight loss programs.
Addressing Real-World Barriers: Cost, Accessibility, and Long-Term Adherence
Despite semaglutide’s efficacy, practical challenges remain, including cost constraints and insurance variability. Proactive solutions involve policy advocacy, patient education on injection techniques, and leveraging telehealth for continuous support. Integrating semaglutide into evidence-based medical weight loss programs can improve adherence and amplify clinical outcomes.
Curated Expert Resources
- FDA Approved Semaglutide Clinical Insights – An authoritative resource detailing clinical applications, safe dosing, and injection protocols essential for maximizing therapeutic outcomes: Access Here.
- Doctor Supervised Semaglutide Safe Dosage Guidelines – Comprehensive guidance on individualized titration strategies and monitoring to mitigate side effects and optimize fat loss: Explore Guidelines.
- Semaglutide and Intermittent Fasting: A Strategic Weight Loss Duo for 2025 – Insightful exploration of synergistic dietary strategies that enhance semaglutide’s efficacy: Learn More.
- Medical Weight Loss Programs Using Semaglutide That Work Fast – Practical frameworks for integrating semaglutide into multidisciplinary treatment plans to ensure rapid and sustained weight loss: Discover Programs.
- Nature Medicine 2023 Review on GLP-1 Receptor Pharmacogenomics – Cutting-edge review elucidating the genetic factors influencing semaglutide response and implications for precision obesity pharmacotherapy: Read Review.
Final Expert Perspective
In synthesizing the multifaceted advancements surrounding semaglutide, it is evident that this FDA approved weight loss medication transcends traditional pharmacotherapy paradigms. Precision medicine through pharmacogenomic profiling, innovative delivery systems, integration with digital health platforms, and strategic lifestyle combinations collectively enhance its therapeutic impact. Addressing real-world barriers remains essential to harness semaglutide’s full potential in clinical practice. Engaging with authoritative resources and fostering collaborative discourse—such as through our expert community—will be pivotal in shaping the future of obesity management.
For those committed to advancing their mastery of semaglutide and contributing to cutting-edge obesity therapeutics, we invite you to explore detailed clinical insights and share your professional perspectives at Contact Us. Together, we can refine best practices and elevate patient outcomes in this dynamic field.


The article provides a comprehensive overview of semaglutide’s impact on FDA-approved weight loss medications, and I find its dual mechanism of improving satiety while reducing appetite particularly compelling. From what I’ve read and observed in discussions with healthcare providers, the prolonged receptor activation is a key factor setting semaglutide apart in terms of efficacy, especially given those impressive clinical trial results showing 15-20% body weight loss. However, the requirement for weekly injections still feels like a potential barrier for many patients, even if adherence is better compared to daily oral meds. I’m curious how others have seen patient acceptance evolve over time, especially with newer delivery options on the horizon. Additionally, the emphasis on tailored dosing and multidisciplinary monitoring makes me wonder about the feasibility in primary care settings where resources might be more limited. Integrating semaglutide safely without overwhelming patients or providers seems to be an ongoing challenge. How have others balanced the need for rigorous patient education and lifestyle counseling to complement semaglutide therapy? It seems combining pharmacotherapy with structured lifestyle changes is essential for sustainable outcomes, but the practical workflow for this integration isn’t always straightforward in a busy clinical practice.