The Revolutionary Rise of Semaglutide in FDA Approved Weight Loss Drugs
In recent years, the landscape of obesity management has experienced a seismic shift with the FDA approval of Semaglutide as a weight loss drug. Originally developed and approved for type 2 diabetes, Semaglutide’s remarkable efficacy in reducing body weight has captivated both medical experts and patients alike. But what exactly sets this injectable medication apart in the crowded arena of weight loss therapies?
Unlocking the Fat-Burning Potential: How Does Semaglutide Work?
Semaglutide belongs to the glucagon-like peptide-1 (GLP-1) receptor agonists class, which mimic a natural hormone that regulates appetite and insulin secretion. By enhancing satiety and reducing hunger signals in the brain, it helps users consume fewer calories without the typical struggle of restrictive dieting. This nuanced mechanism not only supports sustained weight loss but also promotes metabolic health improvements, such as better glycemic control.
What Makes Semaglutide Different from Other FDA Approved Weight Loss Drugs?
Unlike older weight loss medications that often focus on stimulating metabolism or suppressing appetite through less targeted pathways, Semaglutide offers a refined, hormone-based approach with a robust clinical safety profile. Clinical trials have demonstrated average weight reductions approaching 15% of body weight when combined with lifestyle modifications — a significant improvement over many alternatives. Moreover, its once-weekly injectable format improves patient adherence compared to daily pills, providing a pragmatic solution for real-world use.
Expert Insights: The Clinical Journey and Patient Experiences
Leading endocrinologists and obesity specialists emphasize that Semaglutide’s effectiveness is maximized when integrated into a comprehensive medical weight loss program. Patients report not only notable weight loss but also enhanced energy levels and better quality of life. For instance, a 45-year-old patient with obesity and prediabetes shared how a supervised Semaglutide regimen resulted in a 20-pound weight loss within three months, alongside improved blood sugar readings.
However, like all medications, Semaglutide is not devoid of considerations. Side effects such as nausea or gastrointestinal discomfort can occur, underscoring the importance of doctor supervision as detailed in safe dosage guidelines.
Strategic Weight Loss Synergies: Semaglutide and Lifestyle Interventions
Integrating Semaglutide with dietary strategies like intermittent fasting or balanced nutrition amplifies results. This synergy taps into the medication’s appetite modulation while reinforcing behavioral changes, leading to sustainable outcomes. For a deeper dive into this innovative combination, explore semaglutide and intermittent fasting insights.
How Can Patients Navigate the Safe and Effective Use of Semaglutide?
Understanding the correct dosing, timing, and monitoring is crucial. Medical supervision is paramount to adjust doses and manage side effects, ensuring the treatment aligns with individual health profiles. Comprehensive guides such as safe dosage and usage of semaglutide injections provide evidence-based frameworks essential for both clinicians and patients.
For those curious about personal results and transformation stories, semaglutide before and after results offer compelling real-world evidence of this drug’s impact.
Engage with this evolving conversation — share your experiences or questions about Semaglutide in the comments below, and help foster a community dedicated to informed and empowered weight loss journeys.
For authoritative information on obesity treatment and FDA approved drugs, the FDA’s official announcement offers a detailed review of Semaglutide’s approval and clinical data.
Learning to Listen: My Journey with Semaglutide’s Side Effects and Adjustments
When I first started my treatment with Semaglutide, I was optimistic but cautious. The promise of significant weight loss was exciting, yet I knew from my research and conversations with my healthcare provider that side effects like nausea and mild gastrointestinal discomfort were possible. Indeed, during the initial weeks, I experienced some queasiness, which made me wonder if the medication was right for me. However, by closely following the doctor-supervised dosage guidelines and communicating openly with my medical team, we adjusted the dose gradually. This approach not only minimized my side effects but also helped me stay consistent with the treatment.
Integrating Semaglutide with Real-Life Challenges: Breaking Old Habits
One of the most insightful parts of my journey was recognizing how Semaglutide influenced my relationship with food. The medication’s appetite-suppressing effects gave me a new perspective on hunger cues. Instead of mindlessly snacking or eating out of boredom, I became more mindful about what and when I ate. This behavioral shift was crucial for long-term success and something I never expected to happen so naturally. Pairing the medication with lifestyle changes, such as balanced nutrition and intermittent fasting techniques, significantly enhanced my results. For anyone interested, the synergy between Semaglutide and intermittent fasting is well worth exploring.
Could Semaglutide Be the Missing Piece in Your Weight Management Puzzle?
This question often comes to mind when I hear others struggling with weight loss. The truth is, Semaglutide is not a magic bullet—it requires commitment, medical supervision, and lifestyle adjustments. But for many, including myself, it has been a game-changer. The key is understanding that it’s part of a broader strategy, not a standalone solution. If you’re curious about how Semaglutide fits into your personal health goals, consulting with a healthcare professional who can tailor the treatment is essential.
Trustworthy Resources That Guided My Choices
Throughout my experience, I leaned heavily on credible information sources to navigate the complexities of this treatment. For example, the FDA’s official announcement on Semaglutide provided me with a solid foundation of understanding regarding its approval and clinical data. Knowing that such an authoritative body has thoroughly vetted the drug gave me confidence in its safety and efficacy. You can read more about this at the FDA’s official announcement.
I also recommend checking out detailed guides like the safe dosage and usage of Semaglutide injections to understand how to manage this treatment responsibly.
Sharing Your Story: Let’s Build a Supportive Community
If you’ve tried Semaglutide or are considering it, I encourage you to share your experiences or questions in the comments below. Weight loss journeys can be isolating, but by opening up, we can learn from each other and create a supportive network. Whether you’ve faced side effects, found effective lifestyle integrations, or simply want to know more about this medication, your input is valuable. Also, explore more personal accounts and expert reviews on related topics like weekly Semaglutide shot results that offer comprehensive overviews and practical tips.
Decoding the Pharmacokinetics and Personalized Dosing Strategies of Semaglutide
Understanding Semaglutide’s pharmacokinetics is crucial for clinicians aiming to tailor treatments to individual patient needs. The drug exhibits a prolonged half-life of approximately one week, enabling its convenient once-weekly administration. However, interpatient variability in absorption and metabolism necessitates a nuanced approach to dosage titration, particularly in populations with renal impairment or hepatic dysfunction. Recent pharmacodynamic studies demonstrate that gradual dose escalation mitigates the incidence of gastrointestinal adverse effects while maintaining therapeutic efficacy, emphasizing the importance of personalized regimens within supervised clinical settings.
Integrating Semaglutide into Multimodal Obesity Management: Beyond Pharmacotherapy
While Semaglutide’s appetite suppression and metabolic benefits position it as a cornerstone in obesity treatment, experts advocate for its use within a comprehensive, behavioral, and psychosocial framework. Cognitive-behavioral therapy (CBT), nutritional counseling, and structured physical activity programs synergize with pharmacological effects to consolidate sustainable lifestyle modifications. This multidimensional approach addresses the complex biopsychosocial etiology of obesity, reducing relapse risk and enhancing quality of life. Furthermore, emerging data on gut-brain axis modulation by GLP-1 receptor agonists suggest potential neurocognitive benefits that warrant further exploration.
What Are the Long-Term Safety and Efficacy Considerations for Semaglutide in Chronic Weight Management?
Longitudinal studies extending beyond two years indicate that Semaglutide maintains significant weight reduction with a stable safety profile, though vigilance for rare adverse events remains imperative. Pancreatitis and medullary thyroid carcinoma concerns, although not definitively linked, necessitate careful patient selection and ongoing monitoring. Additionally, the cessation of therapy often leads to weight regain, underscoring the need for sustained treatment plans and continuous patient engagement. A pivotal trial published in The New England Journal of Medicine provides comprehensive data supporting these observations.
Clinicians must weigh these factors against patient-specific risks and benefits, tailoring interventions accordingly. Shared decision-making and transparent communication are vital for optimizing adherence and outcomes.
Semaglutide’s Role in Addressing Comorbid Metabolic Disorders: A Holistic Perspective
Beyond weight loss, Semaglutide exerts profound effects on glycemic control, lipid profiles, and blood pressure regulation, positioning it as a multifaceted agent in metabolic syndrome management. Its glucose-lowering action is mediated by enhanced insulin secretion and delayed gastric emptying, which together improve postprandial glucose excursions. Consequently, patients with type 2 diabetes and obesity experience dual benefits, reducing polypharmacy and simplifying treatment regimens.
Moreover, recent investigations reveal Semaglutide’s potential in reducing inflammatory markers and improving endothelial function, which may translate into cardiovascular risk reduction. These pleiotropic effects highlight the importance of integrating Semaglutide within broader cardiometabolic care pathways, ideally coordinated by multidisciplinary teams.
Exploring Cutting-Edge Research: Semaglutide and Neuroendocrine Interactions Influencing Appetite and Weight Regulation
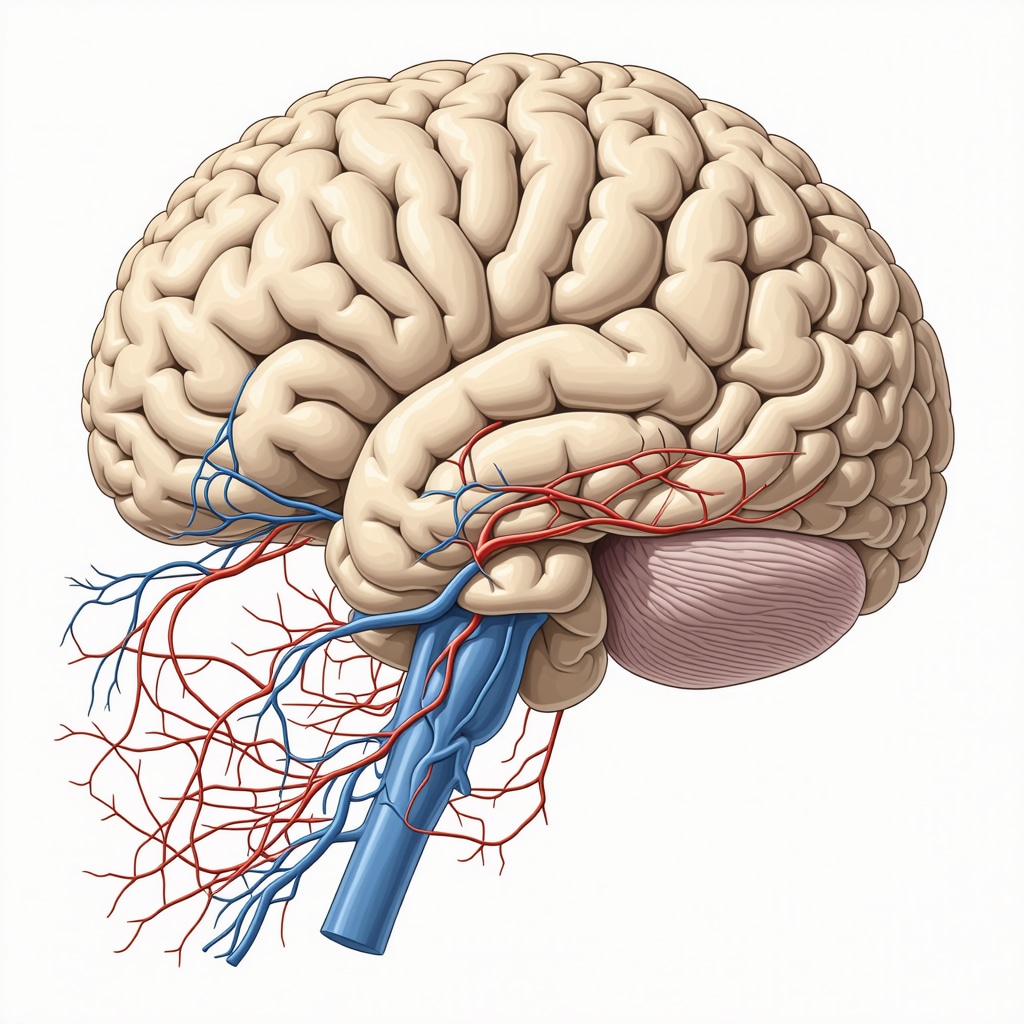
Emerging research delves into the neuroendocrine mechanisms by which Semaglutide modulates central appetite circuits. Functional neuroimaging studies demonstrate altered activity in the hypothalamus and reward-related brain regions, elucidating how GLP-1 receptor agonists recalibrate hunger and satiety signaling. These insights pave the way for next-generation therapeutics targeting specific neural pathways to enhance efficacy and minimize side effects.
Further investigation into individual genetic and epigenetic factors influencing response variability could enable precision medicine approaches, optimizing treatment outcomes. Collaborative efforts between endocrinologists, neuroscientists, and pharmacologists are critical to unravel these complex interactions.
Can Semaglutide Therapy Be Safely Combined with Other Pharmacological Agents for Weight Loss?
Combining Semaglutide with other weight loss agents presents both opportunities and challenges. Polypharmacy may enhance efficacy via complementary mechanisms but raises concerns about additive side effects and drug interactions. Current evidence suggests cautious co-administration with agents like bupropion-naltrexone or orlistat under strict medical supervision. However, robust clinical trials are sparse, and guidelines recommend individualized risk-benefit assessments.
Healthcare providers must remain vigilant for adverse events and adjust therapeutic plans dynamically. Patients should be thoroughly educated about potential risks, signs of complications, and the importance of adherence to monitoring protocols.
For a deeper understanding of combination therapies and emerging protocols, consult specialized pharmacological reviews and clinical trial registries.
Engage with Our Expert Community: If you are navigating complex treatment decisions involving Semaglutide or wish to explore personalized strategies integrating pharmacotherapy and lifestyle, leave your questions or insights below. Our panel of specialists is committed to providing evidence-based guidance to empower your weight management journey.
Precision Pharmacology: Tailoring Semaglutide Dosing for Optimal Outcomes
Delving deeper into the pharmacological nuances of Semaglutide reveals the imperative of individualized dosing strategies. Given its prolonged half-life and complex metabolism, clinicians must consider patient-specific factors such as renal function, hepatic status, and concomitant medications to optimize therapeutic efficacy while mitigating adverse effects. Recent pharmacokinetic modeling underscores the benefits of gradual titration schedules, which not only enhance tolerability but also sustain metabolic improvements over extended treatment periods.
Neural Circuitry Modulation: Unpacking Semaglutide’s Impact on Appetite Regulation
Cutting-edge neuroimaging studies illuminate how Semaglutide modulates central nervous system pathways involved in hunger and satiety. By activating GLP-1 receptors within the hypothalamus and mesolimbic reward centers, the drug recalibrates the neural encoding of food cues and hedonic responses. This sophisticated neuroendocrine interplay not only reduces caloric intake but may also influence mood and cognitive functions related to eating behaviors, offering a promising avenue for integrated obesity management.
Can Semaglutide Be Safely Combined with Other Weight Loss Medications to Enhance Therapeutic Efficacy?
The prospect of combinatorial pharmacotherapy involving Semaglutide and other FDA-approved agents such as bupropion-naltrexone or orlistat is gaining traction among obesity specialists. While preliminary evidence suggests potential additive benefits through complementary mechanisms—appetite suppression, fat absorption inhibition, or neurochemical modulation—the risks of amplified side effects and complex drug-drug interactions necessitate rigorous clinical evaluation. Current consensus advocates for individualized treatment plans under meticulous medical supervision, with ongoing research poised to refine protocols.
Authoritative Evidence and Expert Recommendations
For comprehensive insights into the long-term safety and efficacy of Semaglutide, The New England Journal of Medicine publishes pivotal clinical trial data elucidating sustained weight loss outcomes and monitoring parameters. Additionally, guidelines from endocrinology societies emphasize the integration of pharmacotherapy with behavioral interventions to maximize benefits.
Unlock the Full Potential of Semaglutide: If you’re navigating complex weight management challenges or considering advanced pharmacological strategies, consult with specialized healthcare professionals to tailor treatment plans that harmonize efficacy, safety, and lifestyle compatibility. Engage with our expert community by sharing your questions or experiences below, and stay informed with the latest research developments.
Frequently Asked Questions (FAQ)
What is Semaglutide, and how does it promote weight loss?
Semaglutide is a glucagon-like peptide-1 (GLP-1) receptor agonist originally developed for type 2 diabetes management. It promotes weight loss primarily by mimicking the GLP-1 hormone, which enhances satiety and suppresses appetite through central nervous system pathways. This leads to reduced caloric intake and improved metabolic parameters.
How is Semaglutide administered, and what dosing strategies optimize safety and efficacy?
Semaglutide is administered as a once-weekly subcutaneous injection. Optimal dosing involves gradual titration starting from a low dose to minimize gastrointestinal side effects such as nausea and vomiting. Clinicians tailor dosing regimens based on individual patient factors, including renal and hepatic function, to maintain therapeutic efficacy while ensuring tolerability.
Can Semaglutide be combined safely with other weight loss medications?
Combining Semaglutide with other FDA-approved weight loss agents like bupropion-naltrexone or orlistat is an area of emerging interest. While potential additive benefits exist due to complementary mechanisms, additive side effects and drug interactions require cautious, individualized medical supervision. Robust clinical trial data are limited, so combination therapy should be approached prudently.
What are the common side effects, and how can patients manage them?
The most common side effects include nausea, vomiting, diarrhea, and mild gastrointestinal discomfort, particularly during dose escalation. Management strategies involve slow dose titration, adequate hydration, dietary adjustments, and close communication with healthcare providers to adjust therapy as needed.
How long should Semaglutide treatment continue, and what are the long-term safety considerations?
Long-term studies indicate that Semaglutide maintains weight loss efficacy over periods exceeding two years with a favorable safety profile. However, discontinuation often leads to weight regain, suggesting the need for sustained treatment plans combined with lifestyle modifications. Rare but serious risks, such as pancreatitis and potential thyroid tumors, necessitate ongoing monitoring and patient selection.
Does Semaglutide offer benefits beyond weight loss?
Yes, Semaglutide improves glycemic control, lipid profiles, and blood pressure, offering cardiovascular and metabolic benefits. It also reduces inflammatory markers and improves endothelial function, positioning it as a valuable agent in managing metabolic syndrome and related comorbidities.
How does Semaglutide affect appetite regulation in the brain?
Semaglutide modulates neural circuits in the hypothalamus and mesolimbic reward centers, altering hunger signals and reducing hedonic responses to food. This neuroendocrine modulation recalibrates eating behaviors, potentially improving mood and cognitive control over food intake.
What lifestyle modifications enhance Semaglutide’s effectiveness?
Integrating Semaglutide with behavioral interventions such as balanced nutrition, intermittent fasting, physical activity, and cognitive-behavioral therapy amplifies weight loss outcomes. This multimodal approach addresses the complex biopsychosocial factors underlying obesity for sustained success.
Who should avoid Semaglutide therapy?
Semaglutide is contraindicated in individuals with a personal or family history of medullary thyroid carcinoma or multiple endocrine neoplasia syndrome type 2. Caution is warranted in patients with pancreatitis history or severe gastrointestinal disease. Comprehensive medical evaluation is essential before initiation.
How can patients and clinicians ensure responsible Semaglutide use?
Responsible use involves thorough patient education, regular monitoring for efficacy and side effects, individualized dosing adjustments, and integration with lifestyle support. Shared decision-making and adherence to evidence-based guidelines optimize outcomes and safety.
Trusted External Sources
- U.S. Food and Drug Administration (FDA) – Provides authoritative information on the approval status, clinical trial data, safety warnings, and official prescribing information for Semaglutide, ensuring clinicians and patients access up-to-date regulatory insights.
- The New England Journal of Medicine (NEJM) – Publishes pivotal clinical trials and longitudinal studies on Semaglutide’s efficacy and safety, offering peer-reviewed, high-impact evidence critical for informed clinical decisions.
- American Society of Clinical Endocrinology (ASCE) – Offers expert guidelines and consensus statements on obesity pharmacotherapy, including practical recommendations for integrating Semaglutide into comprehensive weight management frameworks.
- Obesity Medicine Association (OMA) – Provides specialized educational resources and clinical protocols on obesity treatment, emphasizing multidisciplinary approaches and pharmacological innovations like Semaglutide.
- National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) – Delivers valuable research summaries and patient-oriented materials about obesity, metabolic disorders, and emerging therapies, supporting holistic understanding of Semaglutide’s role.
Conclusion: Synthesizing Semaglutide’s Role in Modern Weight Management
Semaglutide represents a transformative advancement in FDA-approved weight loss pharmacotherapy, marrying sophisticated neuroendocrine mechanisms with practical dosing regimens to achieve substantial and sustained weight reduction. Its ability to improve metabolic health markers while modulating central appetite pathways distinguishes it from traditional agents, making it an indispensable component of comprehensive obesity management. Nonetheless, its optimal use hinges on individualized dosing, vigilant monitoring, and integration with lifestyle and behavioral strategies.
As research continues to unravel Semaglutide’s full therapeutic potential and neurobiological effects, clinicians and patients alike are empowered to embrace precision medicine approaches that enhance efficacy and safety. The journey toward effective weight management is multifaceted, and Semaglutide offers a powerful, scientifically grounded tool within this complex puzzle.
We encourage readers to share their experiences, ask questions, and explore related expert content to foster an informed and supportive community dedicated to advancing health and well-being through evidence-based interventions.


The insights into Semaglutide’s mechanism—particularly its hormone-based approach in regulating appetite—really highlight how revolutionary it is compared to traditional weight loss drugs. I’ve read that the key lies in its ability to signal fullness to the brain, which helps reduce calorie intake naturally. What fascinates me most is the reported effect on metabolic health, not just weight loss. Improving parameters like glycemic control while losing weight could be life-changing, especially for patients grappling with type 2 diabetes alongside obesity.
However, what I find particularly compelling is the emphasis on integrating Semaglutide into a comprehensive lifestyle program rather than viewing it as a standalone miracle cure. The patient stories citing significant weight loss combined with better energy levels speak to its potential, but also signal the importance of medical supervision and behavioral changes. It makes me wonder how accessible such supervised programs are for the average patient and what barriers exist in real-world settings.
For those already on this treatment, how have you managed the initial side effects like nausea, and what lifestyle changes did you find most supportive? Also, for practitioners, are there any innovative approaches you’ve seen in integrating pharmacotherapy like Semaglutide with psychological support to sustain long-term outcomes? It would be enlightening to hear diverse experiences and strategies.
Jessica’s point about the importance of integrating Semaglutide into a comprehensive lifestyle program really resonates with me. From what I’ve learned and experienced, tackling weight loss solely with medication often falls short without addressing the underlying behavioral patterns. Managing the initial side effects like nausea can indeed be challenging. In my experience, gradual dose escalation under medical supervision, as emphasized by the article, helped ease these symptoms. I also found that staying well-hydrated and adjusting meal composition—favoring smaller, more frequent meals with balanced nutrients—mitigated gastrointestinal discomfort.
Regarding supportive lifestyle changes, incorporating mindfulness-based eating habits made a significant difference for me. Semaglutide naturally curbed my appetite, but being mindful about food choices and recognizing true hunger cues amplified the benefits. As for psychological support, I’ve come across some clinics integrating cognitive-behavioral therapy alongside pharmacotherapy to address emotional eating and sustain motivation. This multidimensional approach seems promising for long-term adherence and success.
I’m curious if others in this community have encountered or are currently participating in such combined treatment models? How do you find the balance between medication and behavioral therapy in maintaining weight loss and overall well-being? It would be great to hear about practical strategies or challenges you’ve faced on this journey.
Building on the insightful points Jessica and Michelle raised about integrating Semaglutide into a comprehensive weight loss regimen, I wanted to share an observation from my own experience. What struck me most was how crucial gradual dose titration is—not only for minimizing nausea but also for fostering long-term adherence. Following the doctor-supervised dosage guidelines really made a difference for me to stay consistent despite initial gastrointestinal discomfort.
Also, the article’s mention of pairing Semaglutide with intermittent fasting caught my attention. I tried a modified intermittent fasting approach, and the appetite suppression from Semaglutide made it remarkably easier to stick with it. This synergy helped me shift from impulsive eating habits to more mindful, controlled meals. I’ve heard some clinics are now embedding psychological support such as CBT alongside pharmacotherapy; this seems promising for sustainable lifestyle changes beyond just medication effects.
However, I’m curious about accessibility challenges. Jessica wondered about real-world barriers to supervised programs, and I’ve seen similar concerns in my community—insurance coverage, cost, and provider availability can limit access. For those who’ve navigated these hurdles, what strategies or resources have helped you get proper medical supervision and comprehensive support with Semaglutide treatment? Any recommendations for connecting with multidisciplinary teams or programs that integrate behavioral therapy would be greatly appreciated.
Building on the thoughtful perspectives shared here, I’d like to emphasize how crucial patient education and realistic expectations are when beginning Semaglutide therapy. While the hormonal mechanism targeting appetite regulation is impressive, as Jessica pointed out, it really shines when combined with behavioral strategies that address emotional eating and lifestyle habits. From my point of view, gradual dose escalation under close medical supervision is key—not only to minimize gastrointestinal side effects but also to empower patients to stay motivated throughout their journey.
I personally found that integrating mindfulness practices helped me become more attuned to true hunger signals, reducing the temptation for snacking driven by stress or boredom. This aligns with what Michelle mentioned about cognitive-behavioral therapy (CBT) being integrated alongside pharmacotherapy. The synergy between medication and psychological support seems promising for curbing relapse.
Regarding the concern about accessibility of supervised programs, I think telehealth has started to bridge some gaps, offering virtual visits with obesity specialists and behavioral therapists. While cost and insurance remain hurdles, expanding these remote options might improve access for many.
Has anyone else experienced telemedicine support while on Semaglutide? How did it compare to in-person supervision in managing side effects and lifestyle coaching? It would be great to hear how different modes of care impact adherence and outcomes.
I really appreciate the detailed exploration of Semaglutide’s role in weight management presented in this post. The emphasis on its hormone-based mechanism of action, particularly how it modulates appetite through central nervous system pathways, is enlightening. From what I’ve discovered, this approach not only supports weight loss but also enhances metabolic health, which is crucial for individuals managing type 2 diabetes alongside obesity.
One aspect that stands out is the importance of integrating Semaglutide with comprehensive lifestyle changes, such as balanced nutrition and intermittent fasting. Combining pharmacotherapy with behavioral interventions, including cognitive-behavioral therapy, seems essential for long-term success. I’ve read that patient adherence improves significantly when side effects like nausea are managed through gradual dose titration under medical supervision.
This brings me to wonder about the accessibility of such comprehensive, supervised programs. Given the challenges around insurance coverage and provider availability, do you think expanding telemedicine offerings could be a viable solution to improve patient access and support? For those who have navigated both in-person and virtual care models, how do you find the effectiveness in terms of side effect management and lifestyle coaching? Sharing these experiences could be invaluable for others considering Semaglutide treatment.