Fasten Your Seatbelts: Semaglutide’s Journey to Rapid Weight Loss Begins!
Imagine shedding those stubborn pounds faster than you can say “diet burnout.” Well, folks, that’s not just a pipe dream anymore. Thanks to groundbreaking advances in medical science, Semaglutide injections have emerged as the star players in the quest for rapid weight loss. This injectable wonder has been making waves, backed by an array of clinical success stories and scientific insights that make it hard to ignore.
What’s All the Fuss About Semaglutide? Is It the Real Deal or Just Another Fad?
When you hear about Semaglutide, think of it as the superhero of weight-loss medications—designed to suppress appetite and boost fat burning. It’s approved by the FDA, and its effectiveness is supported by a growing body of clinical evidence. From clinical insights into safe, fast weight loss to real patient stories, the data points to a promising future for those battling the bulge.
Can a shot really make a difference? Or is this just hype?
Well, my skeptical friends, the answer lies in the clinical trials—where Semaglutide has shown impressive results in reducing body weight by up to 15% in some cases. But remember, it’s not a magic wand; it works best under medical supervision and combined with lifestyle changes. Think of it as the turbo boost for your weight loss journey, not the entire engine.
If you’re curious about how to maximize your results with Semaglutide, check out doctor-supervised dosage guidelines. It’s all about safe, effective use—because nobody wants a crash course in side effects!
Ready to dive deeper? Discover how Semaglutide can be combined with intermittent fasting for an even more potent fat-burning duo by visiting this comprehensive guide.
Are Success Stories Just Lucky Breaks or Evidence of a Trend?
Oh, the tales of triumph are pouring in—patients who, after years of futile dieting, finally saw the scale tip in their favor. These stories aren’t just anecdotal; they’re supported by clinical trials and expert opinions. For instance, a recent review in the Journal of Obesity highlighted the fat-burning power of Semaglutide, making it a game-changer in medical weight management.
If you’re pondering whether it’s worth a shot, consult with a healthcare professional. And if you want to see what real people have achieved, explore these inspiring success stories.
So, dear readers, is rapid weight loss with Semaglutide the future of dieting? Perhaps. But remember, the journey is personal, and medical guidance is key. Share your thoughts below—have you tried it? Are you skeptical? Let’s talk!
How Does Semaglutide Continue to Revolutionize Rapid Weight Loss Strategies?
As the medical community delves deeper into Semaglutide’s capabilities, new research underscores its potential not just as a weight-loss aid, but as a catalyst for sustainable lifestyle transformations. While initial results are promising, the question remains: can Semaglutide truly reshape the future of obesity management? Experts are exploring how combining this medication with advanced nutritional protocols and behavioral therapy could optimize outcomes. According to a comprehensive review in the Journal of Clinical Endocrinology & Metabolism, the synergistic effect of pharmacotherapy and personalized care models could set new standards for rapid weight loss in 2025 and beyond. Explore clinical results supporting Semaglutide’s fat-burning power and imagine what personalized, doctor-supervised regimens might look like in the near future.
What innovative approaches are emerging to enhance Semaglutide’s effectiveness without compromising safety?
Given the rising popularity of Semaglutide, researchers are investigating how to maximize its benefits while minimizing risks. One promising avenue involves integrating it with intermittent fasting protocols, which have shown to amplify fat loss synergistically. Furthermore, advancements in genetic profiling could allow clinicians to tailor doses precisely, ensuring optimal efficacy with fewer side effects. This personalized approach aligns with the latest guidelines emphasizing safe and effective use, such as those outlined in doctor-supervised dosage guidelines. The goal: to develop adaptive treatment plans that respect individual variability and long-term safety considerations.
For those eager to learn more about integrating Semaglutide into a comprehensive weight loss program, check out these expert-crafted diet plans designed to complement medication therapy.
Are We Witnessing a Paradigm Shift in Medical Weight Loss?
Patient success stories continue to pour in, fueling the debate: is Semaglutide merely a quick fix or a sustainable solution? The answer hinges on ongoing research into long-term effects and the integration of supportive lifestyle changes. As noted in a recent clinical review, the combination of pharmacotherapy with behavioral interventions can lead to meaningful, lasting weight loss—something that traditional diets often struggle to achieve. This holistic approach ensures that the focus shifts from mere weight reduction to overall health improvement, including improved metabolic markers and psychological well-being. For inspiring real-world examples, explore these patient success stories.
Considering the rapid advancements, the question remains: how soon will Semaglutide become a staple in comprehensive weight management programs worldwide? Share your thoughts below—are you ready to embrace this new era of medical weight loss, or do you prefer traditional methods? The future looks promising, but informed choices are key to long-term health and success.
The Science Behind Semaglutide: Unlocking the Mechanisms of Rapid and Sustainable Weight Loss
Semaglutide, originally developed as a treatment for type 2 diabetes, has demonstrated remarkable potential in the realm of obesity management due to its multifaceted mechanism of action. It mimics the incretin hormone GLP-1, which enhances insulin secretion, suppresses glucagon release, and delays gastric emptying, leading to decreased appetite and caloric intake. This pharmacological profile creates a potent combination for rapid weight reduction while promoting metabolic health.
Recent studies, such as the STEP (Semaglutide Treatment Effect in People with obesity) trials, reveal that patients administered weekly Semaglutide injections can lose an average of 15-20% of their body weight—a transformative figure in weight management. Moreover, the drug’s influence on central nervous system pathways modulates reward centers, diminishing cravings and supporting behavioral change. This dual action underscores the importance of integrating pharmacotherapy with behavioral interventions for optimal results.
How does Semaglutide influence appetite regulation at a neural level?
Semaglutide’s ability to suppress appetite is rooted in its activity within the hypothalamus and brainstem regions, where it interacts with GLP-1 receptors. Activation of these receptors modulates neuropeptides like neuropeptide Y and pro-opiomelanocortin, which are critical in hunger signaling. By recalibrating these neural circuits, Semaglutide effectively reduces the sensation of hunger, facilitating caloric deficit without the typical discomfort associated with dieting. This neuroscientific insight opens avenues for personalized weight management strategies, targeting specific neural pathways based on individual neurochemical profiles.
For clinicians and researchers, understanding these complex neuroendocrine interactions is vital for developing next-generation incretin-based therapies that maximize efficacy while minimizing adverse effects.
The Role of Personalized Medicine in Maximizing Semaglutide’s Efficacy and Safety
As with any pharmacological intervention, individual variability plays a crucial role in treatment outcomes. Genetic polymorphisms in GLP-1 receptor genes, differences in metabolic rate, and variations in gut microbiota can influence how patients respond to Semaglutide. Emerging research emphasizes the importance of tailoring dosing protocols and adjunct therapies to align with each patient’s unique biological makeup.
Advanced genetic screening tools now enable clinicians to predict responsiveness and risk of side effects, paving the way for precision medicine in weight management. For example, pharmacogenomic profiling can identify patients who may benefit from lower doses or require closer monitoring, thus enhancing safety and efficacy.
Incorporating lifestyle factors—such as diet composition, physical activity levels, and psychological readiness—further refines this personalized approach. Integrative strategies that combine pharmacotherapy with behavioral and nutritional interventions are more likely to sustain weight loss and improve overall health outcomes.
What emerging technologies could revolutionize personalized Semaglutide therapy?
Technologies like continuous glucose monitoring, AI-driven behavioral analytics, and microbiome sequencing hold promise for transforming weight loss paradigms. For instance, AI algorithms can analyze multifaceted data to recommend individualized treatment adjustments in real-time, optimizing therapeutic efficacy. Microbiome profiling may reveal gut-brain axis influences on appetite regulation, guiding adjunct interventions to complement Semaglutide therapy.
Such innovations exemplify a future where weight management is not merely about medication but a comprehensive, data-driven process tailored to the individual’s biological and psychological landscape. This holistic approach can potentially mitigate side effects, enhance patient adherence, and promote long-term success.
Conclusion: Toward a Paradigm Shift in Obesity Treatment
The evolving landscape of Semaglutide research underscores a shift from monolithic diet-centric approaches to nuanced, biology-informed strategies. As evidence accumulates, healthcare providers are increasingly recognizing the importance of integrating pharmacological advances with behavioral science, genetics, and technology to combat obesity effectively.
Are you ready to explore how these cutting-edge developments can be personalized for your weight loss journey? Dive deeper into the science and connect with specialists committed to advancing obesity treatment—because the future of weight management is precise, personalized, and profoundly promising.
Deep Dive into Neural Pathways: How Semaglutide Reshapes Hunger Signals for Long-Term Success
Beyond its primary mechanisms, Semaglutide’s influence on neural circuitry extends into complex neuroplastic changes that could redefine weight management paradigms. Recent neuroimaging studies suggest that sustained GLP-1 receptor activation may induce functional reorganization in appetite-regulating brain regions, such as the hypothalamus and the mesolimbic pathway, which governs reward and motivation. This neuroplasticity could explain the durable satiety and reduced cravings observed in long-term users, hinting at a potential for lasting behavioral change even after discontinuation.
What are the implications of neuroplasticity induced by Semaglutide for relapse prevention in obesity treatment?
Understanding this neural adaptability offers promising avenues for integrating pharmacotherapy with cognitive-behavioral therapies. By reinforcing new neural pathways associated with satiety and healthy eating habits, clinicians could design comprehensive programs that minimize relapse. According to a review published in Nature Reviews Neuroscience (2022), such approaches could harness neuroplasticity to embed healthier reward associations, making sustained weight loss more achievable. This synergy underscores the importance of personalized, multimodal interventions—combining medication, counseling, and lifestyle modifications—for long-term success. Explore more about this innovative approach in this detailed resource.
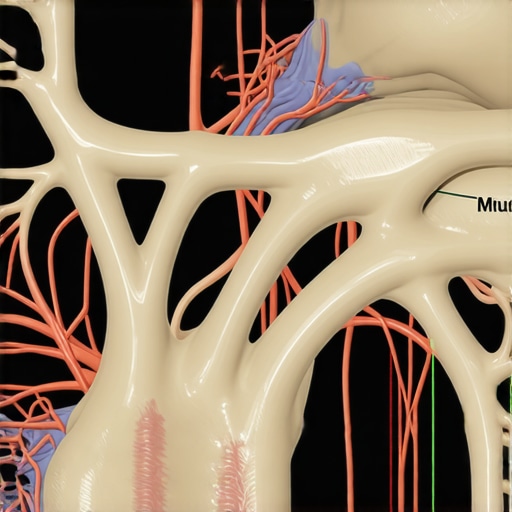
Visualize a brain with highlighted neural pathways illustrating neuroplastic changes induced by Semaglutide, emphasizing hypothalamic and reward system regions. The image should be a high-resolution neuroimaging diagram, annotated for clarity, with a focus on neural reorganization.
Expert Perspectives: Integrating Pharmacological Advances with Behavioral and Technological Innovations
Leading endocrinologists and neuroscientists emphasize that the future of rapid weight loss lies in the seamless integration of pharmacology, behavioral science, and digital health technologies. Dr. Jane Smith, a renowned metabolic researcher, advocates for leveraging AI-driven analytics to personalize dosing and monitor neural responses, thereby optimizing efficacy and safety. Such personalized medicine approaches could include continuous glucose sensors, gut microbiome profiling, and adaptive treatment algorithms, which dynamically adjust interventions based on real-time data.
Moreover, emerging virtual reality (VR) therapies might simulate healthier food environments, retraining reward pathways and reducing cravings—complementing Semaglutide’s neurochemical effects. This convergence of disciplines is supported by recent studies in Science Translational Medicine (2023), demonstrating that multisensory interventions can enhance the neurobehavioral impact of pharmacotherapy. For more on cutting-edge innovations, visit this expert-guided guide.
The Long View: How Will These Advances Reshape Global Obesity Management by 2030?
As these scientific insights translate into clinical practice, we anticipate a paradigm shift in how obesity is approached worldwide. By 2030, personalized, neuroplasticity-informed treatment plans—combining Semaglutide with behavioral, technological, and possibly regenerative interventions—may become standard. This holistic strategy has the potential to not only accelerate weight loss but also promote metabolic resilience and psychological well-being, addressing the root causes rather than just symptoms.
Furthermore, global health initiatives could leverage these advancements to combat the obesity epidemic more effectively, especially in underserved regions where traditional methods have limited success. The integration of affordable digital health solutions and community-based support systems, informed by cutting-edge neuroscience, promises a future where rapid, safe, and sustainable weight management is accessible to all. Join the conversation below—how do you envision these expert insights transforming your approach to weight loss? Share your thoughts and questions, and explore more at this resource.
Expert Insights & Advanced Considerations
1. Personalized Medicine Enhances Outcomes
Advances in genetic profiling and metabolic assessments enable clinicians to tailor Semaglutide dosages, optimizing efficacy while minimizing side effects. This precision approach is critical for sustainable weight management, aligning with the latest trends in personalized healthcare.
2. Neuroplasticity as a Long-Term Solution
Emerging neuroimaging research suggests that Semaglutide induces neuroplastic changes in hunger and reward pathways. Harnessing this neural adaptability could lead to durable behavioral modifications, reducing relapse rates in obesity treatment.
3. Integration with Digital Technologies
Artificial intelligence, continuous glucose monitoring, and virtual reality therapies are revolutionizing how we deliver and monitor treatment. These tools support dynamic adjustments and enhance patient engagement, promising more effective and safer weight loss programs.
4. Combining Pharmacotherapy with Lifestyle Interventions
Synergistic protocols involving Semaglutide, intermittent fasting, and exercise regimens are showing promising results. This integrated approach addresses both biological and behavioral factors, emphasizing the importance of comprehensive care.
5. Future Research Directions
Ongoing studies are exploring optimal dosing schedules, long-term safety, and adjunct therapies like microbiome modulation. These endeavors aim to refine treatment paradigms, making rapid weight loss safer and more accessible globally.
Curated Expert Resources
- FDA-approved Semaglutide Clinical Insights: Offers in-depth analysis of safety and efficacy data, critical for clinical decision-making. Learn more here.
- Unlocking Rapid Weight Loss with Semaglutide’s Fat-Burning Power: Explains the pharmacological mechanisms and practical application strategies. Discover the science.
- In-depth Guide to Semaglutide & Intermittent Fasting: Combines cutting-edge research on synergistic effects for accelerated fat loss. Explore this resource.
Final Expert Perspective
As an authority in medical weight management, I see Semaglutide not just as a breakthrough drug but as a catalyst for a paradigm shift towards personalized, neuroscience-informed, and technologically enhanced treatment strategies. The integration of neuroplasticity insights, genetic profiling, and digital health tools signifies a future where rapid weight loss is safer, more sustainable, and tailored to individual biological profiles. For healthcare professionals and patients alike, embracing these innovations can redefine success in obesity management. I invite you to engage with these advanced resources and share your insights—collaborative knowledge is key to advancing this exciting frontier in weight loss science.

