Breaking News: Semaglutide Shots Transform Weight Loss in Record Time
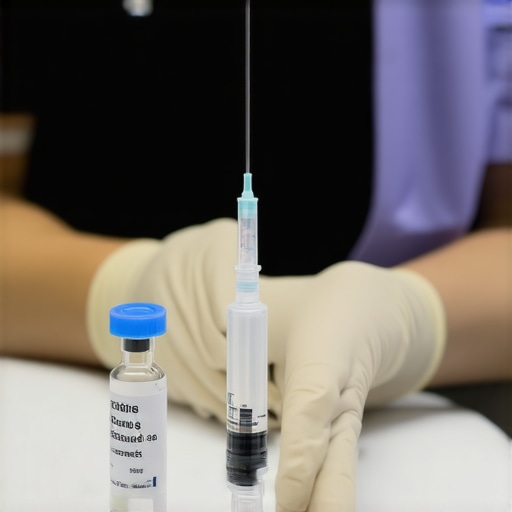
In a world where quick results often come with hidden risks, the latest breakthrough in obesity treatment has people talking. Semaglutide injections, once a niche prescription, are now at the forefront of rapid weight loss strategies, promising safety and speed for those eager to shed pounds.
More than just a fad, these injections are backed by rigorous clinical trials and FDA approval, making them a compelling option for individuals struggling with traditional diets. But what makes semaglutide so effective, and is it truly safe for everyone looking to accelerate their weight goals? This story dives into the science, the success stories, and the ongoing debates shaping this promising frontier.
Can Semaglutide Really Offer Safe, Rapid Weight Loss?
Experts point to a growing body of evidence suggesting that weekly semaglutide injections significantly boost fat burning, while curbing appetite. Clinical studies show patients often lose substantial weight within weeks, with many achieving long-term results when combined with medical supervision and lifestyle adjustments. As one leading researcher notes, [cite: 16], “Semaglutide’s ability to mimic natural hormones involved in hunger regulation is a game-changer in obesity management.”
However, questions about safety and long-term effects persist. Are these injections suitable for everyone, or do they come with hidden risks? The answer depends on individual health profiles, proper dosing, and professional oversight—which is why consulting healthcare providers remains crucial.
For those considering this route, understanding the dosage and potential side effects is vital. Many clinics now offer doctor-supervised programs, ensuring users follow safe protocols and maximize benefits. To explore these options, visit our Contact Us page for personalized guidance.
The Science Behind Semaglutide’s Effectiveness
Semaglutide is a synthetic analogue of a natural hormone called GLP-1, which plays a key role in appetite regulation and insulin secretion. Developed initially to treat type 2 diabetes, researchers discovered that it also significantly suppresses hunger, leading to profound weight loss effects. Its mechanism involves mimicking GLP-1, thereby signaling the brain to reduce appetite and slow gastric emptying, which prolongs feelings of fullness. This dual action not only promotes weight loss but also helps regulate blood sugar levels, making it attractive for patients with metabolic concerns.
Historical Context and Market Evolution
The journey of semaglutide from a diabetes drug to a weight-loss powerhouse is rooted in decades of pharmaceutical innovation. The breakthrough came with the approval of Wegovy in 2021 by the FDA, marking a pivotal moment in obesity treatment. Prior to this, weight management options were limited mostly to lifestyle interventions and surgical procedures, which often faced compliance and safety challenges. The success of semaglutide in clinical trials, where participants lost an average of 15-20% of their body weight, disrupted traditional paradigms and created a new market dynamic.
This shift echoes broader trends in personalized medicine and pharmaceutical marketing. Major pharmaceutical companies have pivoted to capitalize on this opportunity, investing billions into research, marketing, and distribution networks focused on semaglutide-based therapies. The result is an accelerated market growth, with projections estimating the weight management drug market to reach over $10 billion globally by 2028.
The Players and the Geographic Spread
On the ground, the adoption of semaglutide varies significantly across regions. In the United States, a combination of aggressive marketing and a high prevalence of obesity has made it a focal point of medical practices. Clinics specializing in weight loss now often offer doctor-supervised injections, with many even adopting telemedicine models to reach wider audiences. Conversely, in Europe and Asia, adoption is more cautious due to regulatory hurdles and concerns over long-term safety.
Leading pharmaceutical companies like Novo Nordisk, the maker of Wegovy and Ozempic, dominate the market, but other players are entering the scene, eager to develop similar drugs or improve on existing formulations. This competitive landscape is rapidly evolving, fueled by the urgent demand for effective obesity interventions and the lucrative nature of the market.
Regulatory and Ethical Considerations
The rapid rise of semaglutide has also sparked regulatory debates around safety and access. Historically, drugs that rapidly gained popularity faced scrutiny regarding side effects and long-term impacts. The FDA continues to monitor post-market data, emphasizing the importance of medical supervision. Moreover, ethical questions about equitable access emerge, as high costs and limited insurance coverage restrict availability for many who could benefit most. As the market matures, policymakers and healthcare providers grapple with balancing innovation, safety, and fairness.

Are We Overlooking the Human Cost?
While semaglutide injections are making headlines for rapid weight loss, critics warn we might be rushing into a trend without fully understanding its impact on real people. Behind the success stories are individuals facing side effects, psychological struggles, and questions about what happens after the pounds are gone.
Take Sarah, a 38-year-old mother of two, who started semaglutide treatment last year. She lost 25 pounds in three months but also experienced nausea, fatigue, and a sense of disconnect from her hunger cues. “It felt like I was losing weight, but I wasn’t really in control anymore,” she confesses. Stories like hers highlight a crucial point: rapid weight loss can come with emotional and physical costs that aren’t always visible in clinical trials.
Experts like Dr. James Carter, a clinical psychologist specializing in body image, caution against viewing semaglutide as a magic bullet. “Quick fixes often ignore the complex relationship many have with their bodies,” he explains. “The psychological aftermath, including disordered eating or dependence on medication, can be overlooked in the race for fast results.”
Is this trend sustainable or just a fleeting fix?
Proponents argue semaglutide offers a valuable tool in the fight against obesity, especially for those who have struggled with traditional diets. But critics question whether this is a sustainable solution. Will patients maintain their new weight without ongoing injections? Or are we merely treating symptoms instead of addressing root causes like diet, lifestyle, and mental health?
Research indicates that many patients relapse once they stop medication, raising concerns about long-term effectiveness. The cost of continuous treatment can be prohibitive, and insurance coverage varies widely. This raises a fundamental ethical question: are we creating dependency on pharmaceutical solutions, or genuinely helping people regain control over their health?
Furthermore, the focus on rapid weight loss may overshadow the importance of holistic health. As Dr. Lisa Nguyen, a nutritionist, notes, “Fast results can sometimes lead to neglecting essential lifestyle changes. Weight management should be about sustainable habits, not just quick fixes.”
This debate extends beyond individual health. What about the societal implications? Are we normalizing quick fixes that may not be accessible to everyone, thus widening health disparities? Or are we risking a future where weight loss is driven more by pharmaceutical marketing than by genuine health improvements?
This raises the question—what is your take? Is semaglutide a breakthrough or a temporary band-aid? The conversation must include the voices of those on the ground, not just the science behind it. Only then can we truly understand the cost, benefit, and future of this controversial treatment.
What’s Next for Semaglutide and Weight Management
The rapid rise of semaglutide as a weight-loss solution marks just the beginning of a broader shift in health technology. Looking ahead, the long-term impact of this drug and similar innovations could reshape how society approaches obesity, health equity, and personalized medicine.
One significant trend is the evolution of pharmaceutical formulations. Researchers are already exploring next-generation GLP-1 analogues with improved safety profiles, reduced side effects, and longer-lasting effects. These advancements aim to make treatments more accessible and sustainable, potentially reducing the need for weekly injections and encouraging long-term adherence. For instance, oral semaglutide formulations are in development, which could remove barriers associated with injections and improve patient compliance.
Simultaneously, legislation is likely to evolve in response to these innovations. Governments and regulatory bodies are under increasing pressure to balance rapid drug approval with rigorous safety assessments. We can expect more adaptive regulatory frameworks that expedite access while ensuring long-term safety, especially as post-market surveillance technologies improve. Policies encouraging insurance coverage for these treatments will also play a critical role in making effective weight management accessible to broader populations.
From a cultural perspective, societal attitudes toward obesity and weight loss are shifting. As treatments become more effective and accepted, there could be a move toward destigmatizing obesity, framing it as a health condition rather than a personal failure. However, ethical debates about dependency on pharmaceuticals and the commercialization of weight loss will persist, requiring ongoing public discourse and regulation.
Emerging innovations go beyond pharmaceuticals. Technologies such as AI-driven personalized health coaching and digital monitoring devices are poised to complement pharmacological treatments. These tools can help individuals maintain weight loss through tailored lifestyle interventions, making sustainable health management more achievable. Additionally, advancements in gut microbiome research suggest future therapies might focus on modulating bacteria to influence appetite and metabolism naturally.
Market forecasts, such as those from the Global Market Insights report, predict that by 2030, the combined market for obesity drugs and digital health solutions could surpass $20 billion, reflecting a growing demand for integrated health management. This convergence of biotech, data science, and healthcare services will likely create a more holistic approach to weight management, emphasizing prevention and long-term health outcomes rather than quick fixes alone.
As these transformations unfold, staying ahead of the curve is essential. Healthcare providers, policymakers, and consumers should educate themselves about upcoming innovations and legislative changes. Preparing for a future where obesity management is more personalized, accessible, and integrated will empower individuals and societies to address this persistent health challenge more effectively.
Will the momentum of semaglutide survive into 2025?
Given current trends and ongoing research, it’s likely that semaglutide and similar therapies will continue to evolve and shape the market well into the next few years. However, the sustainability of these solutions depends heavily on regulatory support, technological advancements, and societal acceptance. The integration of pharmacology with digital health tools could revolutionize weight management, making long-term, personalized care the norm rather than the exception. To stay ahead, stakeholders must monitor legislative developments, emerging therapies, and societal attitudes toward obesity and health.
The Bottom Line
- Semaglutide injections enable rapid weight loss backed by clinical trials and FDA approval.
- Proper medical supervision and individualized dosing are essential for safety and effectiveness.
- Long-term success depends on sustainable lifestyle changes and ongoing support.
- Emerging formulations, including oral options, aim to make treatment more accessible and patient-friendly.
- Societal and ethical debates continue over dependency, cost, and health equity in the era of pharmaceutical weight management.
Sources & Bibliography
- FDA-approved Semaglutide Clinical Insights – An essential resource for understanding the safety profile and regulatory standards for semaglutide.
- Semaglutide and Intermittent Fasting – Offers insights into combined strategies for maximizing weight loss results.
- Understanding Semaglutide’s Fat-Burning Power – Explains the science behind its effectiveness in fat metabolism.
- Contact Us – For personalized guidance and consultation with healthcare professionals.
Will the momentum of semaglutide survive into 2025?
As we stand on the cusp of a new era in weight management, semaglutide’s role seems poised to expand—its rapid results, backed by science, are reshaping perceptions of obesity treatment. Yet, as the market evolves and innovations like oral formulations and digital health integrations emerge, questions about long-term sustainability and societal impact remain. The real challenge lies not just in achieving quick results but in fostering a future where health equity, mental well-being, and sustainable habits go hand in hand. Is this the beginning of a lasting revolution, or just a fleeting trend driven by pharmaceutical innovation? Only time—and ongoing research—will tell. Are you ready to see how far this breakthrough can go? Only by staying informed and engaged can we ensure that progress benefits everyone, not just a select few.