Unlocking the Synergy: How Diet Amplifies Semaglutide’s Weight Loss Power
Embarking on a semaglutide injection regimen is an exciting step toward transformative weight loss, but the injection alone is only part of the equation. Integrating a thoughtfully designed diet plan can significantly enhance your results, improve your metabolic health, and support sustainable fat loss. This article delves into expert-backed semaglutide diet plans crafted to complement your injection journey, blending medical science with practical nutrition strategies for optimal outcomes.
Reimagining Nutrition: The Core Principles Behind Semaglutide-Supported Diets
Semaglutide works by mimicking the glucagon-like peptide-1 (GLP-1) hormone, which regulates appetite and glucose metabolism. Understanding this mechanism guides the dietary choices that best complement the drug’s effects. Diets rich in high-quality proteins, fiber, and low-glycemic carbohydrates help stabilize blood sugar levels and prolong satiety—maximizing semaglutide’s appetite-suppressing benefits.
Emphasizing nutrient-dense whole foods such as leafy greens, lean meats, legumes, and healthy fats fosters metabolic efficiency and reduces cravings. Avoiding processed sugars and refined grains mitigates insulin spikes that could undermine fat loss. This strategic nutritional alignment empowers semaglutide users to experience smoother weight loss trajectories and improved energy levels.
Practical Meal Frameworks: Structuring Your Days Around Semaglutide
Experts recommend structuring meals to harness semaglutide’s appetite modulation, ideally consuming smaller, nutrient-packed meals spaced evenly throughout the day. For example, a typical day might begin with a protein-rich breakfast including eggs and spinach, followed by fiber-loaded snacks like nuts or berries, and balanced lunches and dinners combining vegetables, whole grains, and lean proteins.
Hydration also plays a critical role. Drinking ample water supports digestion and can help manage any gastrointestinal side effects sometimes experienced during semaglutide therapy.
How Can Intermittent Fasting Complement Semaglutide for Accelerated Fat Loss?
Intermittent fasting (IF) has emerged as a powerful dietary strategy that, when paired with semaglutide, can amplify fat-burning mechanisms. By limiting eating windows, IF enhances insulin sensitivity and promotes fat mobilization, working synergistically with semaglutide’s appetite suppression. However, timing and personalization are key—consulting with a healthcare provider ensures this combination supports your unique health profile without compromising nutrition.
For readers interested in detailed guidance, exploring this resource on semaglutide and intermittent fasting offers scientifically grounded insights.
Expert Tips for Navigating Challenges and Maximizing Results
Weight loss journeys with semaglutide are highly individual. Some users may experience mild nausea or digestive discomfort initially; adjusting meal composition to lighter, easily digestible foods can alleviate these symptoms. Regular monitoring of blood glucose and nutritional intake ensures safety and effectiveness, especially for those with underlying metabolic conditions.
Additionally, pairing semaglutide with professional medical support and personalized diet planning—as highlighted in doctor-supervised semaglutide programs—can optimize your weight loss while minimizing risks.
Ready to elevate your semaglutide journey with a tailored diet plan? Share your questions or success stories below, and join a community committed to smart, sustainable fat loss.
For deeper exploration of semaglutide’s clinical benefits and diet integration, the National Institutes of Health provides comprehensive research on GLP-1 receptor agonists and obesity management.
Listening to Your Body: Adjusting Your Semaglutide Diet as You Progress
One of the most important lessons I’ve learned on my semaglutide journey is that no one-size-fits-all diet plan exists, especially when it comes to integrating medication that affects your appetite and metabolism. Early on, I noticed fluctuations in my energy levels and occasional digestive discomfort, which prompted me to tweak my meal timing and food choices. For instance, swapping heavier dinners for lighter, protein- and fiber-rich options helped ease those initial side effects and kept me energized throughout the day.
It’s crucial to be attuned to how your body responds and to communicate openly with your healthcare provider. This personalized approach can make a significant difference in maintaining momentum and avoiding burnout.
Balancing Macronutrients: What Worked for Me
While semaglutide naturally suppresses appetite, I found that consciously balancing my macros—especially prioritizing lean proteins and complex carbs—provided sustained fullness and better workout recovery. Incorporating foods like grilled chicken, quinoa, and a variety of colorful vegetables kept my meals exciting and nutrient-dense. Healthy fats from sources such as avocado and nuts also played a key role in keeping hunger at bay.
Interestingly, research from the National Institutes of Health highlights how combining GLP-1 receptor agonists like semaglutide with nutrient-dense diets can optimize fat loss and metabolic health (NIH Study on GLP-1 and Obesity), reinforcing the importance of quality nutrition alongside medication.
Have you noticed changes in your food preferences or appetite since starting semaglutide?
This question often comes up in conversations I have with others embarking on this treatment. Many report a decreased desire for sugary or processed foods, which aligns with semaglutide’s appetite modulation effects. Personally, I found myself naturally gravitating toward healthier options, making diet adherence less of a chore and more of a lifestyle shift.
Tips for Staying Consistent and Motivated
Consistency is key, but life’s unpredictability sometimes challenges even the best-laid plans. To stay on track, I recommend prepping meals in advance, keeping healthy snacks handy, and celebrating small victories along the way. Joining online communities or following blogs that focus on semaglutide and diet synergy can provide encouragement and practical tips.
If you’re considering combining semaglutide with intermittent fasting, or want a comprehensive plan tailored just for you, check out some trusted resources like doctor-supervised semaglutide programs and strategic weight loss guides to ensure safe and effective results.
I’d love to hear your stories and insights! Have you tried semaglutide with a specific diet plan? What worked or didn’t work for you? Feel free to share your experiences in the comments below to support others on this path.
Precision Macronutrient Timing: Unlocking Metabolic Flexibility with Semaglutide
Beyond simply balancing macronutrients, the timing of nutrient intake plays a pivotal role in amplifying semaglutide’s efficacy. Chrononutrition—the science of aligning eating patterns with circadian rhythms—suggests that consuming higher protein and complex carbohydrates earlier in the day can synchronize metabolic processes, enhance insulin sensitivity, and sustain energy levels. This strategic timing not only supports semaglutide’s appetite suppression but also mitigates postprandial glucose spikes, contributing to a more stable metabolic environment.
For instance, front-loading calories with a nutrient-dense breakfast rich in amino acids and fiber primes the body for optimal glucose disposal throughout the day. Conversely, lighter dinners emphasizing healthy fats and low-glycemic vegetables can reduce nocturnal insulin secretion and support overnight fat oxidation. Integrating these principles requires individualized planning, considering personal circadian tendencies and physical activity schedules.
Synergizing Semaglutide with Gut Microbiome Modulation: The Next Frontier in Weight Management
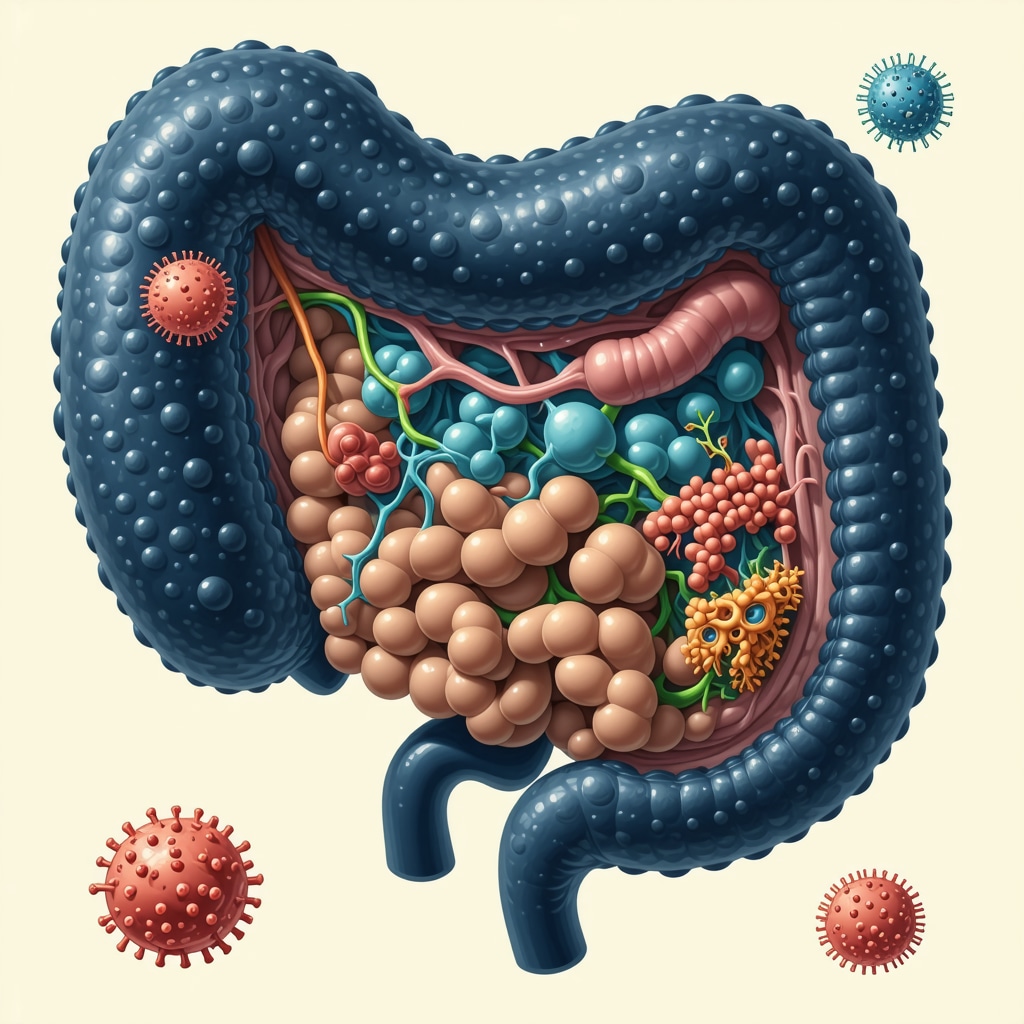
Emerging research underscores the bidirectional relationship between GLP-1 receptor agonists like semaglutide and gut microbiome composition. Semaglutide may influence microbial diversity by modulating gastrointestinal motility and nutrient absorption, while a balanced microbiome can enhance GLP-1 secretion and metabolic regulation. This interplay opens promising avenues for dietary strategies that nurture beneficial microbes to optimize semaglutide’s weight loss potential.
Incorporating prebiotic-rich foods such as inulin-containing chicory root, garlic, and onions, alongside fermented probiotics like kefir and kimchi, fosters a gut environment conducive to improved GLP-1 activity. Moreover, reducing intake of processed foods and emulsifiers that disrupt microbial integrity is critical. Personalized microbiome testing, though still nascent, can guide targeted dietary adjustments to maximize therapeutic synergy.
How Does Gut Microbiota Influence Semaglutide’s Effectiveness in Weight Reduction?
Gut microbiota impact energy homeostasis, inflammation, and hormone signaling—all central to weight regulation. Specific microbial strains enhance endogenous GLP-1 production, complementing semaglutide’s pharmacological action. Conversely, dysbiosis can impair GLP-1 pathways, diminishing treatment response. Understanding these complex interactions enables clinicians and nutritionists to tailor interventions that harness microbiota-modulated mechanisms, potentially improving outcomes for semaglutide users (Frontiers in Endocrinology, 2022).
Personalized Nutrigenomics: Tailoring Semaglutide Diets to Genetic Profiles
Advancements in nutrigenomics reveal that genetic variations significantly influence individual responses to semaglutide and dietary interventions. Polymorphisms in genes regulating appetite, insulin sensitivity, and lipid metabolism may dictate optimal macronutrient ratios and timing for each patient. Integrating genetic testing into clinical practice offers a cutting-edge approach to customizing semaglutide diet plans, enhancing adherence and efficacy.
For example, individuals with FTO gene variants associated with increased hunger may benefit from higher protein and fiber intake, while those with genes affecting lipid metabolism might require tailored fat quality adjustments. Collaborating with genetic counselors and dietitians trained in nutrigenomic interpretation can unlock these personalized nutrition strategies, advancing semaglutide therapy beyond conventional paradigms.
Unlocking Deeper Insights: Next Steps in Optimizing Your Semaglutide Journey
These sophisticated strategies underscore the importance of a holistic, precision-based approach to semaglutide-supported weight loss. As science evolves, integrating macronutrient timing, microbiome modulation, and nutrigenomic insights will become paramount to achieving sustained, individualized success.
Are you interested in exploring personalized semaglutide diet plans that incorporate your unique genetic and microbiome profile? Connect with our expert team to dive deeper into cutting-edge strategies tailored just for you.
Chrononutrition Mastery: Synchronizing Meal Timing with Semaglutide’s Pharmacodynamics
Building upon the concept of precision macronutrient timing, chrononutrition offers a sophisticated lens through which to optimize semaglutide’s pharmacological effects. Aligning nutrient intake with circadian biology not only enhances metabolic flexibility but also potentiates semaglutide’s efficacy in appetite regulation and glucose homeostasis. Incorporating a morning-centric feeding window rich in complex carbohydrates and amino acids primes insulin sensitivity and maintains satiety, while evening meals emphasizing low-glycemic index vegetables and healthy fats reduce nocturnal metabolic strain.
Such temporal alignment requires nuanced personalization, considering individual chronotypes and lifestyle demands to avoid metabolic desynchrony and optimize therapeutic outcomes.
Microbiome-Targeted Nutritional Interventions: Elevating Semaglutide’s Impact Through Gut Health Optimization
Recent advances illustrate a compelling bidirectional interaction between semaglutide treatment and gut microbiota modulation. The drug’s influence on gastrointestinal motility and nutrient absorption may reshape microbial communities, which in turn can affect endogenous GLP-1 secretion and systemic metabolic regulation. Integrating prebiotic fibers like inulin, resistant starches, and polyphenol-rich foods alongside fermented probiotics such as kefir and kimchi cultivates a diverse, resilient microbiome that synergizes with semaglutide’s mechanisms.
Reducing dietary emulsifiers and processed additives further preserves microbial integrity, thereby enhancing drug responsiveness and mitigating gastrointestinal side effects.
What Are the Mechanistic Pathways Linking Gut Microbiota Modulation to Enhanced Semaglutide Weight Loss Efficacy?
Emerging research identifies several mechanistic pathways wherein gut microbiota influence semaglutide’s effectiveness: modulation of enteroendocrine L-cell activity enhancing endogenous GLP-1 secretion; attenuation of systemic inflammation reducing insulin resistance; and alterations in bile acid metabolism that optimize lipid absorption and energy expenditure. Dysbiosis disrupts these pathways, potentially blunting semaglutide’s therapeutic action. Consequently, microbiome-targeted dietary strategies represent a promising adjunct to pharmacotherapy, as detailed in a 2022 peer-reviewed article published in Frontiers in Endocrinology, underscoring the clinical relevance of gut microbiome modulation in obesity treatment.
Integrating Nutrigenomics: Customizing Semaglutide Diet Plans Based on Genetic Insights
Progress in nutrigenomics reveals that individual genetic polymorphisms significantly dictate metabolic responses to both semaglutide and dietary macronutrient compositions. For instance, variants in the FTO gene influence appetite regulation and energy expenditure, suggesting a heightened need for protein and fiber-rich diets to mitigate hunger signals. Similarly, polymorphisms affecting lipid metabolism inform tailored fat quality recommendations, optimizing cardiovascular and weight loss outcomes.
Collaborative approaches involving genetic counselors and specialized dietitians enable the translation of these genomic insights into actionable, personalized nutrition plans that complement semaglutide therapy, thereby enhancing adherence and efficacy.
Engage with Experts to Unlock Personalized Semaglutide Nutrition Solutions
Harnessing the full potential of semaglutide for sustainable weight loss demands an integrative strategy encompassing chrononutrition, gut microbiome optimization, and nutrigenomics. If you aspire to explore bespoke dietary frameworks finely tuned to your unique biological and genetic landscape, connect with our team of experts. We specialize in translating cutting-edge scientific insights into practical, individualized semaglutide diet protocols designed to maximize efficacy and long-term success.
Take the next step in your weight loss journey by scheduling a personalized consultation today — empower your transformation with precision nutrition and expert guidance.
Frequently Asked Questions (FAQ)
What is the ideal diet to maximize semaglutide’s weight loss effects?
The most effective diet to complement semaglutide emphasizes nutrient-dense whole foods rich in lean proteins, fiber, and low-glycemic carbohydrates. This approach stabilizes blood sugar, prolongs satiety, and aligns with semaglutide’s appetite-suppressing mechanism. Avoiding processed sugars and refined grains further supports metabolic health and fat loss.
Can intermittent fasting be safely combined with semaglutide therapy?
Yes, intermittent fasting (IF) can synergize with semaglutide by enhancing insulin sensitivity and fat mobilization. However, timing and individual tolerance vary, so it’s critical to consult healthcare providers to tailor IF protocols safely, ensuring adequate nutrition and avoiding hypoglycemia or excessive hunger.
How does gut microbiome health influence semaglutide’s effectiveness?
The gut microbiome modulates metabolic pathways including endogenous GLP-1 secretion, inflammation, and energy balance. A balanced, diverse microbiota can enhance semaglutide’s pharmacodynamics, while dysbiosis may blunt its efficacy. Incorporating prebiotic fibers, fermented probiotics, and minimizing processed foods can optimize gut health and augment weight loss outcomes.
What role does macronutrient timing play in semaglutide-supported diets?
Chrononutrition strategies that front-load protein and complex carbohydrates in the morning and favor lighter, low-glycemic meals in the evening can enhance insulin sensitivity and metabolic flexibility. This temporal nutrient distribution complements semaglutide’s pharmacodynamics and supports sustained energy and fat oxidation.
Are genetic differences important when planning a semaglutide diet?
Absolutely. Nutrigenomic variations—such as FTO gene polymorphisms—affect appetite regulation and metabolism, influencing optimal macronutrient ratios and dietary strategies. Personalized nutrition informed by genetic testing can enhance semaglutide adherence and efficacy by tailoring diet plans to individual metabolic profiles.
What common side effects should be managed through diet during semaglutide treatment?
Gastrointestinal discomfort and mild nausea are common initially. Consuming smaller, easily digestible meals that are protein- and fiber-rich, staying well hydrated, and avoiding fatty or heavily processed foods can mitigate these symptoms and improve tolerance.
How important is professional supervision when using semaglutide for weight loss?
Professional medical supervision is crucial to ensure safe dosing, monitor metabolic parameters, and provide personalized dietary guidance. Doctor-supervised programs optimize therapeutic outcomes and minimize risks, especially for individuals with comorbidities.
Can lifestyle factors like physical activity enhance semaglutide’s effects?
Yes, integrating regular physical activity supports metabolic health, improves insulin sensitivity, and complements semaglutide’s weight loss mechanisms. Combined lifestyle modifications amplify overall efficacy and promote sustainable fat loss.
Is there evidence supporting the synergy of semaglutide and specialized diets?
Robust clinical research and emerging studies, including those from NIH and peer-reviewed journals, demonstrate that semaglutide’s efficacy is heightened when paired with diets optimized for macronutrient quality, timing, and gut microbiome support, confirming the value of integrative nutritional strategies.
Where can I find personalized semaglutide diet plans?
Specialized clinics and expert nutritionists offering genetic and microbiome testing services provide tailored semaglutide diet plans. Engaging with multidisciplinary teams ensures dietary approaches are aligned with your unique biology for maximum benefit.
Trusted External Sources
- National Institutes of Health (NIH) – GLP-1 Receptor Agonists and Obesity Management: Offers comprehensive, peer-reviewed research on semaglutide’s pharmacology and clinical applications, informing evidence-based diet integration strategies.
- Frontiers in Endocrinology (2022) – Gut Microbiome and GLP-1 Interactions: Provides in-depth mechanistic insights into how gut microbiota modulate semaglutide’s efficacy, guiding microbiome-targeted nutritional interventions.
- American Diabetes Association (ADA): Supplies clinical guidelines on GLP-1 therapies and nutritional recommendations for metabolic health, enhancing safe semaglutide usage.
- International Society of Nutrigenetics/Nutrigenomics: Offers expert consensus and research updates on genetic influences in nutrition, supporting personalized semaglutide diet planning.
- Obesity Medicine Association: A resource for best practices in obesity pharmacotherapy combined with medical nutrition therapy, ensuring holistic patient care.
Conclusion
Optimizing semaglutide’s transformative weight loss potential extends far beyond pharmacology; it hinges on integrating precision nutrition tailored to individual biological rhythms, gut microbiome health, and genetic profiles. Embracing nutrient-dense, balanced diets rich in protein, fiber, and low-glycemic carbohydrates, timed strategically throughout the day, amplifies appetite regulation and metabolic efficiency. Concurrently, fostering a healthy gut environment and leveraging nutrigenomic insights personalizes therapy to maximize adherence and outcomes.
Achieving sustainable fat loss with semaglutide is a dynamic, multifaceted journey that thrives on expert guidance, continuous self-awareness, and lifestyle integration. We invite you to apply these advanced strategies, share your experiences, and explore further expert content to empower your transformation with confidence and precision.


I’ve been following your discussion about integrating diet with semaglutide, and I must say, the emphasis on high-quality proteins and low-glycemic carbs really resonates with my experience. When I started semaglutide, I noticed my appetite decreased quite a bit, but it was the nutrient-dense meals, like grilled chicken with quinoa and plenty of veggies, that helped me maintain energy levels and avoid the typical fatigue that often comes with calorie restriction. The idea of timing macronutrient intake to align with circadian rhythms is fascinating too—I had not realized how front-loading protein and complex carbs in the morning could improve metabolic flexibility and insulin sensitivity. On the challenge side, managing the initial mild nausea was tricky, but switching to smaller, fiber-rich meals spaced throughout the day really helped with tolerability. I’d be curious to know if others have experimented with intermittent fasting alongside semaglutide and how they’ve balanced the fasting windows without compromising necessary nutrient intake. Has anyone found particular meal timing or food combinations especially effective in overcoming those early side effects or maintaining workout performance while on semaglutide?
Building on what Lydia mentioned about intermittent fasting (IF) combined with semaglutide, I’ve been experimenting with a 14:10 IF window while on semaglutide and found it crucial to prioritize nutrient-dense meals during the eating period. I tend to schedule my first meal shortly after my morning injection to align nutrient intake with semaglutide’s appetite-suppressing peak. This seems to help me avoid significant hunger during fasting without compromising energy for my afternoon workouts. Smaller, protein- and fiber-rich meals spaced evenly within the feeding window have mitigated the nausea side effects, which I initially struggled with. Hydration also plays a key role; sipping water infused with lemon or herbal teas helps support digestion and keep nausea at bay. I do think that individualizing meal timing based on how one’s body responds to both semaglutide and fasting is essential, and consulting healthcare providers for tailored protocols prevents potential issues like hypoglycemia. For those who have tried combining IF and semaglutide, how have you managed balancing fasting periods without feelings of fatigue or dizziness? Also, has anyone noticed their workout recovery improved or diminished during IF while using semaglutide? I’d be eager to hear different strategies or experiences to better navigate this combo.
Building on the wonderful insights shared about timing macronutrients with semaglutide, I’ve personally experienced that leaning into a protein- and fiber-rich breakfast early in the day really makes a difference in hunger control through the afternoon. It aligns well with the concept of chrononutrition highlighted in the article. On the challenge side, I initially faced some mild nausea, similar to others, and found that breaking my meals into smaller, evenly spaced portions throughout the day helped significantly. I also started adding fermented foods like kefir to my diet after reading about the gut microbiome’s role in semaglutide’s effectiveness—this addition seemed to help with digestion and overall metabolic balance. Regarding combining intermittent fasting with semaglutide, while I have not tried a strict fasting window, I maintain a consistent 12-hour overnight fasting period to give my digestion a break. I wonder if anyone experimenting with longer fasting windows has adjusted their hydration or electrolyte intake to manage energy levels and nausea? I’d love to hear about strategies others have found effective for sustaining energy and workout performance while managing side effects on this journey.
I’ve been closely following the insights shared here about combining semaglutide injections with diet to amplify weight loss. What particularly struck me is the role of gut microbiome modulation alongside precision nutrition, something that I hadn’t considered deeply before. Since starting semaglutide, I noticed that my digestive comfort greatly improved when I incorporated fermented foods like kimchi and kefir, which seemed to support both my appetite regulation and energy. The concept of personalized nutrigenomics is fascinating too—understanding that genetic differences can influence how we respond to diet and medication opens new possibilities for tailoring plans that truly fit individual needs. It’s empowering to think that by integrating my unique genetic and gut profile, I might optimize my fat loss journey even more. Has anyone here explored genetic testing to customize their semaglutide diet? If so, how did it influence your food choices or macronutrient balance? Also, I’m curious about practical steps for nurturing gut health during semaglutide treatment—does anyone have favorite prebiotic or probiotic-rich recipes or tips that helped support their progress? It seems this multi-layered approach, blending medication, diet, microbiome, and genetics, holds real promise but might also feel overwhelming at first. How do others navigate balancing these elements without getting discouraged?
Replying to Lydia — I’ve been experimenting with semaglutide plus a modest IF window and wanted to share what helped me bridge the fasting periods without losing workout performance. I eased in with 12:12 for two weeks, then moved to 14:10; that gradual approach reduced dizziness and allowed me to learn how my body responded. Timing matters: I schedule my first meal about 45–60 minutes after my morning injection when possible, focusing on a protein-forward plate (eggs or a protein shake) with a small portion of complex carbs for energy. For workouts, a light pre-workout snack (Greek yogurt with berries or a 20–25 g protein shake) and a recovery meal within 60–90 minutes afterward kept strength and recovery steady.
To manage nausea and low energy, I found small, bland, low-fat meals, ginger tea, and electrolyte-rich drinks (or a cup of low-sodium broth) helpful during longer fasts. Always monitor how you feel and check with your provider if you have metabolic conditions. Curious—what’s your go-to pre/post-workout snack while on semaglutide?
I really appreciate the detailed insights shared here about integrating diet with semaglutide. From personal experience, I’ve found that focusing on nutrient-dense, low-glycemic foods not only helps with satiety but also keeps my energy stable throughout the day. The emphasis on timing meals to align with circadian rhythms has made a noticeable difference in my metabolic health and appetite control, especially when I increase my morning intake of proteins and complex carbs. I’ve also begun experimenting with gut-friendly foods like kimchi and kefir, which seem to support digestion and overall well-being. What’s been most encouraging is seeing how small adjustments—like adding fermented foods or shifting meal times—can significantly improve side effects and workout performance. Has anyone else noticed particular foods or timing strategies that help reduce nausea or boost energy during their semaglutide journey? Also, how do you balance maintaining variety in your diet while keeping consistent with nutrient timing? Curious to hear more practical tips from those who’ve navigated these tweaks successfully!
This article really resonated with me, especially the focus on nutrient timing and microbiome health. Since starting semaglutide, I’ve noticed that incorporating high-protein breakfasts and probiotic-rich foods like yogurt and sauerkraut has helped reduce the nausea I initially experienced. I’ve been experimenting with meal timing, trying to front-load my calories in the morning to maximize satiety and insulin sensitivity, which seems to work well with the drug’s appetite suppression. However, I still find that managing energy levels during fasting windows can be tricky, particularly during long days at work when I can’t prep meals as easily. Has anyone found effective strategies for maintaining energy and focus while combining semaglutide with intermittent fasting, especially on busy days? Also, I’d love to hear how others have personalized meal timing to suit their lifestyles and biological rhythms—it seems like the key to long-term success. This comprehensive approach to diet and medication makes me optimistic about sustainable weight loss.
I found this discussion about balancing diet and semaglutide especially helpful, as I recently started my injection regimen. Incorporating nutrient-dense foods like lean proteins and fiber-rich vegetables has made a noticeable difference in managing side effects like nausea, while also helping me stay energized throughout the day. The emphasis on meal timing, particularly front-loading calories in the morning, aligns well with my current experience and seems to enhance the medication’s appetite-suppressing effects. I’ve also been experimenting with probiotic foods like kefir and sauerkraut, which appear to support digestion and metabolic health. What surprises me most is how small dietary adjustments can significantly improve overall well-being and weight loss progress on semaglutide. I’m curious, have others found specific foods or meal timing strategies particularly effective in overcoming initial side effects or sustaining energy levels? Additionally, how have you personalized your diet to fit your daily routine and biological rhythms? It would be great to hear some practical tips and shared experiences so I can fine-tune my approach for better results.