Harnessing the Dynamic Duo: Semaglutide Meets Intermittent Fasting
In the evolving landscape of weight management, two strategies have garnered significant attention for their potent fat loss capabilities: semaglutide, a groundbreaking FDA-approved injectable medication, and intermittent fasting, a time-restricted eating pattern hailed for metabolic benefits. When combined thoughtfully, these approaches may unlock accelerated and sustainable fat loss results that go beyond traditional dieting methods.
Why Semaglutide Amplifies Fat Burning in Fasting States
Semaglutide mimics the glucagon-like peptide-1 (GLP-1) hormone, enhancing insulin secretion, suppressing appetite, and slowing gastric emptying. This pharmacological effect aligns seamlessly with intermittent fasting’s metabolic adaptations—such as increased fat oxidation and improved insulin sensitivity—to create a metabolic environment primed for rapid fat loss. Clinical trials have demonstrated semaglutide’s efficacy in reducing body weight by targeting obesity mechanisms at a hormonal level (NEJM Semaglutide Obesity Trial).
Creative Strategies to Maximize Synergy Between Semaglutide and Fasting
To truly leverage this combination, personalized approaches are essential. Implementing a 16:8 intermittent fasting protocol while initiating semaglutide under medical supervision can optimize appetite control and enhance fat mobilization. Additionally, pairing this with nutrient-dense, low-glycemic meals during eating windows supports stable blood sugar and sustained energy. Such integrated plans, often structured by healthcare professionals, ensure safety and effectiveness (doctor-supervised semaglutide plans).
How Does Combining Semaglutide and Intermittent Fasting Impact Long-Term Metabolic Health?
Beyond immediate weight loss, this combination may improve long-term metabolic markers by reducing insulin resistance and promoting favorable changes in lipid profiles. However, individual responses vary, and sustained benefits depend on adherence, lifestyle integration, and ongoing medical evaluation. Awareness of potential side effects, such as gastrointestinal symptoms from semaglutide, is crucial to managing treatment effectively.
Real-World Success: Case Studies Illuminating the Path
Consider a 45-year-old patient with obesity who integrated weekly semaglutide injections with a 16:8 intermittent fasting regimen. Over 24 weeks, the patient experienced significant weight reduction, improved energy levels, and reduced cravings, illustrating the practical impact of combining pharmacotherapy with lifestyle modification. Such cases emphasize the importance of expert guidance and customized protocols to maximize outcomes.
Explore more on combining semaglutide and intermittent fasting for fat burn to deepen your understanding of this powerful strategy.
If this expert insight resonates with your weight loss journey, connect with specialists who can tailor a safe, effective plan just for you.
Facing Challenges Head-On: My Personal Semaglutide and Fasting Journey
Embarking on the semaglutide and intermittent fasting journey wasn’t without its hurdles. Initially, the gastrointestinal side effects—nausea and mild dizziness—tested my resolve. However, by gradually adjusting the semaglutide dosage under my doctor’s guidance and modifying my fasting schedule slightly, I found a rhythm that my body could tolerate better. This experience underscored the importance of doctor supervision in managing the treatment safely and effectively.
Incorporating Mindful Eating Habits Alongside Fasting and Medication
One insight that profoundly impacted my progress was integrating mindful eating during my eating windows. Rather than rushing meals or mindlessly snacking, I focused on savoring nutrient-dense foods, which enhanced satiety and reduced the temptation to overeat. This mindful approach complemented semaglutide’s appetite-suppressing effects, making it easier to maintain a calorie deficit without feeling deprived.
What Role Does Emotional Well-being Play in Successful Weight Loss with Semaglutide and Fasting?
Weight loss is as much an emotional journey as a physical one. From my experience and supported by research from the National Institutes of Health, maintaining emotional well-being helps prevent relapse and supports sustained lifestyle changes. Semaglutide’s effect on hunger hormones can reduce food cravings, but addressing emotional triggers and practicing stress management remain vital components of long-term success.
Practical Tips for Staying Consistent and Motivated
To keep momentum, I recommend setting realistic milestones and celebrating small victories. Tracking progress through weekly weigh-ins and journaling how semaglutide and fasting affect energy and mood can provide tangible feedback. Also, connecting with communities or healthcare specialists experienced in semaglutide treatment can offer invaluable support and accountability.
If you’re curious about crafting a personalized plan or want to hear about others’ journeys, don’t hesitate to reach out to experts or share your story in the comments below. Your insights might just inspire someone else starting this transformative path.
Integrating Advanced Nutrigenomics with Semaglutide and Fasting for Personalized Fat Loss
Emerging research in nutrigenomics reveals that genetic variations significantly influence how individuals respond to both pharmacological agents like semaglutide and dietary regimens such as intermittent fasting. Tailoring fasting windows and nutrient intake based on one’s genetic profile can optimize semaglutide’s efficacy by enhancing metabolic flexibility and minimizing side effects. For instance, polymorphisms in genes regulating GLP-1 receptor sensitivity may dictate dosage adjustments or fasting schedules, ensuring maximal therapeutic benefit while maintaining patient comfort.
This bespoke approach transcends the traditional one-size-fits-all paradigm, ushering in a new era where weight loss strategies are harmonized with an individual’s unique genomic landscape. Healthcare practitioners equipped with genetic data can customize semaglutide titration and fasting protocols to mitigate adverse reactions such as nausea or hypoglycemia, thereby improving adherence and outcomes.
Decoding the Biochemical Symphony: How Semaglutide Alters Hormonal Crosstalk During Fasting
When semaglutide is administered concomitantly with intermittent fasting, it orchestrates a complex hormonal interplay beyond appetite suppression. The drug modulates incretin hormones and influences the hypothalamic-pituitary-adrenal axis, which collectively recalibrate energy homeostasis. This recalibration fosters a metabolic milieu favoring enhanced lipolysis and mitochondrial biogenesis, mechanisms critical for sustained fat oxidation.
Moreover, semaglutide’s role in attenuating postprandial glucagon spikes during feeding windows can stabilize glycemic excursions, reducing the propensity for insulin resistance development over time. Understanding these nuanced hormonal dynamics enables clinicians to strategically time medication and fasting periods, optimizing fat loss while preserving lean muscle mass.
How Do Variations in Fasting Protocols Affect Semaglutide’s Pharmacodynamics and Fat Loss Efficiency?
The pharmacodynamics of semaglutide can be markedly influenced by the chosen intermittent fasting regimen. For example, alternate-day fasting may induce different gastric emptying rates and GLP-1 receptor engagement compared to daily time-restricted feeding (16:8). Such variations alter semaglutide absorption kinetics and its subsequent effects on appetite regulation and insulin secretion.
Clinical observations suggest that individuals practicing prolonged fasting windows might experience amplified semaglutide benefits due to synergistic elevation of ketone bodies, which themselves act as metabolic modulators. However, this requires careful balancing to avoid hypoglycemia, especially in patients with comorbidities. Hence, an integrative approach considering fasting duration, semaglutide dosage, and patient metabolic status is paramount.
For an in-depth exploration of these interactions and evidence-based fasting protocols tailored to semaglutide therapy, consult the Journal of Clinical Endocrinology & Metabolism, which offers comprehensive analyses on pharmacokinetic and metabolic outcomes.
Leveraging Continuous Glucose Monitoring (CGM) to Fine-Tune Semaglutide and Fasting Regimens
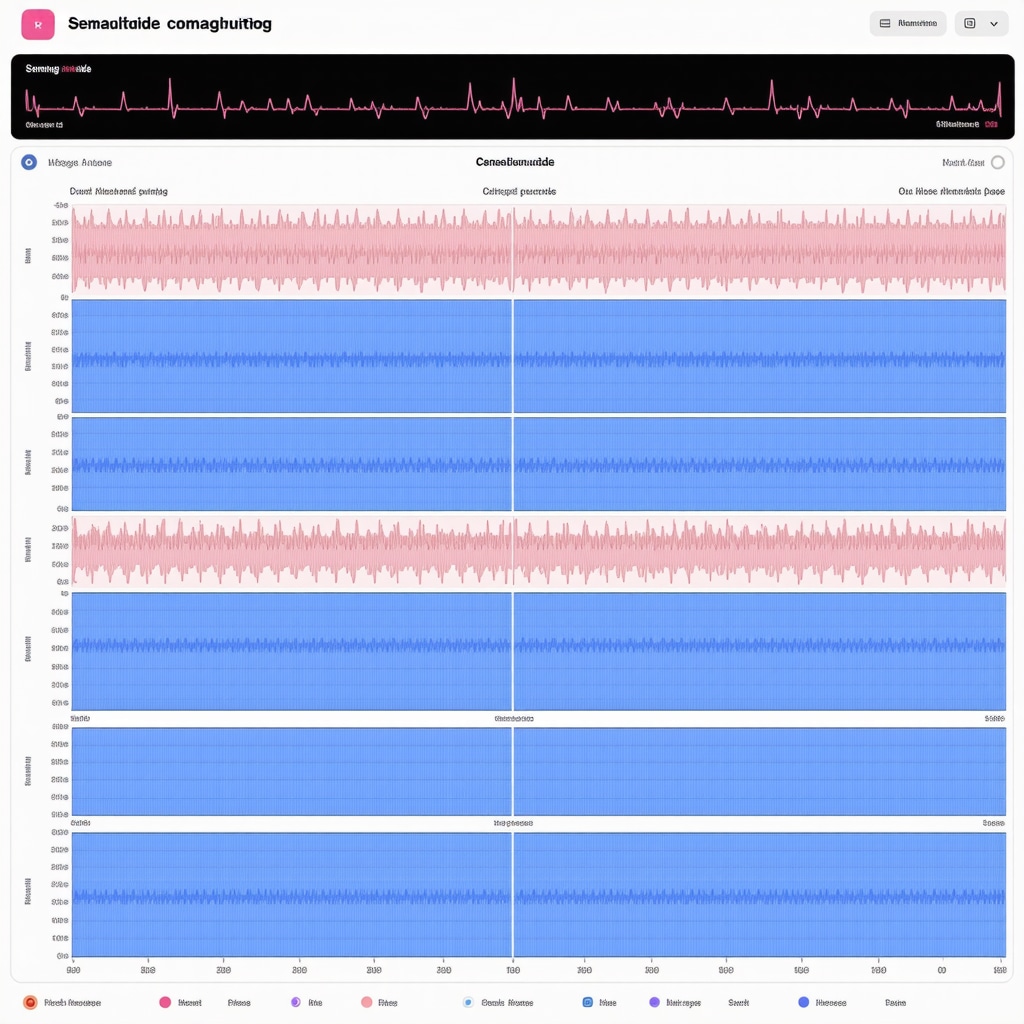
Integrating technology such as CGM systems empowers patients and clinicians to observe real-time glycemic responses to semaglutide under various fasting schedules. This data-driven feedback loop facilitates precise modifications to medication timing and fasting windows, reducing risks of hypoglycemia and enhancing metabolic control.
CGM insights also reveal patterns in glucose variability linked to dietary composition during eating phases, informing adjustments that complement semaglutide’s action. Such precision medicine tools are invaluable for patients with type 2 diabetes or insulin resistance, where balancing glucose levels is critical to safe and effective fat loss.
Incorporating CGM into treatment protocols embodies the cutting edge of personalized weight management and underscores the necessity of multidisciplinary collaboration among endocrinologists, dietitians, and patients.
If you’re ready to harness these advanced strategies and personalized tools, connect with our expert team to develop a data-informed semaglutide and fasting plan tailored uniquely to your metabolic profile.
Personalizing Fat Loss: The Intersection of Nutrigenomics and Therapeutic Fasting
Recent strides in nutrigenomics underscore the profound impact of genetic polymorphisms on individual variability in response to semaglutide administration combined with intermittent fasting. Variations in genes encoding the GLP-1 receptor and metabolic regulators can significantly influence therapeutic outcomes, necessitating genotype-informed customization of dosing and fasting schedules. This tailored strategy not only potentiates metabolic efficiency but also mitigates adverse events, fostering improved patient adherence in clinical practice.
Unveiling the Hormonal Nexus: Semaglutide’s Modulation of Metabolic Pathways During Fasting
Semaglutide’s pharmacodynamics extend beyond appetite suppression by intricately modulating hormonal axes during fasting states. It recalibrates the hypothalamic-pituitary-adrenal axis and incretin hormone profiles, promoting enhanced lipolysis and mitochondrial biogenesis. These biochemical adjustments facilitate sustained fat oxidation and preserve lean muscle mass, crucial for long-term metabolic health. Timing semaglutide administration to coincide with fasting windows can optimize these hormonal effects, but requires meticulous clinical oversight to balance efficacy and safety.
How Do Different Intermittent Fasting Protocols Influence Semaglutide’s Pharmacokinetics and Therapeutic Efficacy?
The interplay between varying fasting regimens—such as alternate-day fasting versus 16:8 time-restricted feeding—and semaglutide’s absorption and receptor engagement dynamics is complex. Prolonged fasting intervals may amplify ketone body production, which synergizes with semaglutide’s metabolic actions to augment fat loss but also heightens hypoglycemia risk in susceptible populations. Therefore, selecting an intermittent fasting protocol must be individualized, taking into account metabolic status, comorbidities, and medication titration schedules.
For an authoritative, data-driven discourse on these nuanced interactions, the Journal of Clinical Endocrinology & Metabolism offers in-depth analyses elucidating pharmacokinetic and metabolic outcomes pertinent to semaglutide and fasting combinations.
Optimizing Treatment Through Continuous Glucose Monitoring (CGM) Technology
Integrating CGM devices into clinical protocols affords granular insight into glycemic fluctuations in response to semaglutide under diverse fasting regimens. This real-time data facilitates dynamic adjustments in medication timing, fasting duration, and nutrient composition to mitigate hypoglycemic episodes and augment metabolic control. Particularly for patients with insulin resistance or type 2 diabetes, CGM-guided interventions epitomize precision medicine, enabling a harmonized approach among endocrinologists, dietitians, and patients.
Employing CGM not only enhances safety but also empowers patients through tangible feedback loops, fostering sustained engagement with their weight loss regimens.
If you seek to leverage these cutting-edge methodologies and bespoke monitoring tools, connect with our expert team to co-create a semaglutide and intermittent fasting strategy meticulously tailored to your unique metabolic blueprint.
Frequently Asked Questions (FAQ)
What is semaglutide and how does it aid in fat loss?
Semaglutide is a GLP-1 receptor agonist medication originally approved for type 2 diabetes and obesity management. It promotes weight loss by enhancing insulin secretion, suppressing appetite, delaying gastric emptying, and modulating metabolic hormones, thereby facilitating reduced caloric intake and improved fat oxidation.
How does intermittent fasting complement semaglutide therapy?
Intermittent fasting induces metabolic adaptations such as increased fat oxidation, improved insulin sensitivity, and elevated ketone production. When combined with semaglutide’s hormonal effects, fasting enhances the medication’s efficacy by synergistically promoting lipolysis and appetite control, optimizing fat loss beyond either strategy alone.
Are there specific fasting protocols better suited when using semaglutide?
Protocols like the 16:8 time-restricted feeding are commonly paired with semaglutide due to their balance between fasting duration and sustainability. However, alternate-day or prolonged fasting may enhance ketogenesis and fat burning but require careful medical supervision to avoid hypoglycemia, especially in patients with comorbidities.
What role does nutrigenomics play in personalizing semaglutide and fasting regimens?
Nutrigenomics examines genetic variations influencing metabolism and drug response. Tailoring semaglutide dosage and fasting schedules based on individual genetic profiles can optimize therapeutic outcomes, minimize side effects, and improve adherence by aligning treatment with one’s unique metabolic and receptor sensitivities.
How can continuous glucose monitoring (CGM) improve treatment outcomes?
CGM provides real-time glucose data, helping clinicians and patients adjust semaglutide dosing and fasting windows dynamically. This minimizes hypoglycemia risk, stabilizes blood sugar, and allows personalized dietary adjustments, crucial for patients with insulin resistance or diabetes undergoing combined therapy.
What are common side effects to expect when combining semaglutide with intermittent fasting?
Gastrointestinal symptoms such as nausea, mild dizziness, or constipation are common during initial semaglutide titration. Intermittent fasting may amplify these effects if not properly managed. Gradual dose escalation, medical supervision, and mindful eating during feeding windows help mitigate adverse events.
Does emotional well-being influence weight loss success with this combination?
Absolutely. Emotional health impacts eating behaviors and adherence. Semaglutide reduces food cravings hormonally, but addressing stress and emotional triggers through mindfulness or counseling enhances long-term lifestyle changes and prevents relapse.
Can semaglutide preserve lean muscle mass during fasting-induced weight loss?
Yes. Semaglutide’s modulation of hormonal axes promotes lipolysis and mitochondrial biogenesis while preserving lean tissue. Combining it with proper nutrition during eating windows and appropriate fasting protocols supports muscle retention during fat loss.
Is professional supervision necessary when combining these treatments?
Yes, medical supervision ensures safe titration of semaglutide, selection of appropriate fasting regimens, monitoring of side effects, and metabolic parameters. Personalized plans reduce risks and enhance efficacy, particularly for individuals with underlying health conditions.
How long does it typically take to see results from combining semaglutide with intermittent fasting?
Weight loss timelines vary but many patients observe meaningful fat reduction within 12 to 24 weeks. Consistency, adherence to prescribed protocols, and integration of lifestyle factors influence the rate and sustainability of results.
Trusted External Sources
- New England Journal of Medicine (NEJM) Semaglutide Obesity Trial: Provides rigorous clinical trial data on semaglutide’s efficacy and safety in weight management, foundational for understanding pharmacological mechanisms.
- Journal of Clinical Endocrinology & Metabolism: Offers in-depth analyses of semaglutide’s pharmacokinetics and metabolic effects in conjunction with intermittent fasting, essential for advanced clinical insights.
- National Institutes of Health (NIH) Nutritional Genomics Research: Explores the impact of genetic polymorphisms on diet and drug response, supporting personalized approaches to weight loss therapy.
- American Diabetes Association (ADA) Scientific Statements: Provides guidelines on glucose monitoring and diabetes management, relevant for integrating CGM with semaglutide and fasting regimens.
- Endocrinology and Metabolism Clinics of North America: Features expert reviews on hormonal regulation during fasting and medication interventions, valuable for understanding biochemical pathways.
Conclusion
Combining semaglutide with intermittent fasting represents a sophisticated and promising strategy for accelerated and sustainable fat loss. This synergistic approach leverages semaglutide’s hormonal modulation and appetite suppression alongside the metabolic benefits of fasting to optimize lipolysis, insulin sensitivity, and energy homeostasis. Personalization through nutrigenomics and continuous glucose monitoring further refines treatment, enhancing efficacy and minimizing side effects. Success hinges on careful medical supervision, mindful eating, and attention to emotional well-being, underscoring the holistic nature of effective weight management. Armed with this expert knowledge, individuals can confidently explore this dynamic duo, transforming their fat loss journey with precision and safety. If you found this comprehensive guide insightful, share it with others, comment your experiences, and explore related expert content to deepen your understanding and support community learning.


What really stands out to me in this post is the careful balance needed between semaglutide use and intermittent fasting to maximize fat loss while minimizing side effects like nausea or dizziness. The point about how personalized plans shaped by healthcare professionals are crucial cannot be overstated. I tried intermittent fasting before but struggled with hunger and energy dips. The idea of semaglutide supporting appetite suppression while fasting seems like a promising way to overcome those barriers. However, it seems critical to also incorporate mindful eating during feeding times to avoid feeling deprived, which is a great insight shared here. I’m curious if anyone else has combined these two approaches under medical supervision? Particularly, does anyone find the 16:8 fasting protocol is flexible enough, or have you experimented with alternate-day fasting with semaglutide? Also, how do you manage the initial side effects? This combination sounds effective but demands a thoughtful and adaptive approach. I’d love to hear diverse experiences and strategies for staying consistent and motivated as well, especially with emotional and psychological hurdles that often accompany weight loss journeys.
Replying to Melanie Turner’s insightful comment—I’ve been on a similar path combining semaglutide with a 16:8 intermittent fasting routine under doctor supervision. I agree the 16:8 protocol strikes a workable balance for many; it’s sustainable without being overly restrictive, which helps maintain energy and mood. That said, a few weeks in, I experimented briefly with alternate-day fasting but found the more prolonged fasting windows challenging alongside semaglutide’s effects, particularly around lightheadedness. Managing initial side effects like nausea took patience and gradual dose increases, as the post recommends, coupled with ensuring I eat nutrient-dense, low-glycemic meals during feeding periods. Mindful eating was a game changer for me, too—really helped curb unproductive snacking and enhanced the appetite suppression from semaglutide. The emotional side of this journey shouldn’t be underestimated; I’ve had to actively practice stress management techniques, like meditation and journaling, to avoid emotional eating triggers. I’m curious, has anyone here integrated continuous glucose monitoring (CGM) into their regimen? The article highlights CGM’s role in fine-tuning semaglutide and fasting schedules to prevent hypoglycemia and optimize fat loss. I’d love to hear about others’ experiences with this technology and how it might impact motivation and consistency during treatment.
Building on Melissa and Jonathan’s experiences, I’ve been integrating semaglutide with a 16:8 intermittent fasting schedule under medical supervision for about six months now. I completely agree that the 16:8 approach strikes a good balance—it’s manageable and doesn’t feel overwhelming, which is crucial for sustainability. I found that starting with a lower semaglutide dose and gradually increasing it helped reduce the nausea and dizziness during the initial weeks. Additionally, pairing the medication with nutrient-dense meals rich in fiber and protein during the eating window stabilized my energy levels and reduced cravings.
One thing I’ve been exploring lately is how genetic factors might influence responses to this combo, following insights from the post’s section on nutrigenomics. It’s fascinating how genetic variations in GLP-1 receptor sensitivity could mean personalized dosing and fasting schedules would markedly improve results and reduce side effects. I wonder, have any others here pursued genetic testing or discussed nutrigenomic approaches with their healthcare providers to fine-tune treatment?
Also, I’m curious about continuous glucose monitoring (CGM) use—while I’ve read about its benefits in adjusting fasting windows and medication timing, I haven’t tried it yet. Has anyone found CGM helpful to boost motivation or prevent hypoglycemia in this context? Sharing how technology integrates with these medical and lifestyle strategies would be insightful for those considering or already on this path.