Is Semaglutide the Game-Changer We’ve Been Waiting For?
Imagine a world where shedding pounds doesn’t feel like an uphill battle but more like a sprint to the finish line. Well, 2025 might just be that world, thanks to groundbreaking clinical evidence supporting semaglutide for rapid obesity treatment. This injectable wonder has been stirring up conversations in medical circles and social media alike, promising faster results with fewer side effects. But what’s the real story behind this hype?
From Lab to Life: The Science Backing Semaglutide
Let’s cut to the chase—semaglutide is not just another weight-loss fad. It’s an FDA-approved medication that mimics a gut hormone called GLP-1, which helps regulate appetite and insulin secretion. Clinical trials have shown that participants using semaglutide experienced significant weight loss in a shorter time frame than traditional methods. According to a recent clinical study, patients saw an average of 15% body weight reduction within just 16 weeks. That’s faster than most diet plans can promise!
Why 2025 Is the Year of Rapid Results
Now, you might wonder—what’s different this year? The answer lies in a combination of new formulations, better dosing guidelines, and the strategic integration of semaglutide with lifestyle changes like fasting and exercise. Medical professionals are increasingly advocating for doctor-supervised protocols to maximize safety and effectiveness, ensuring that rapid weight loss doesn’t come at the cost of health risks.
Can Semaglutide Really Accelerate My Weight Loss Journey?
It’s a fair question—after all, no one wants to trade one problem for another. Evidence suggests that when used appropriately, semaglutide can significantly accelerate fat burning without the common side effects associated with crash diets. Plus, its ability to curb appetite means fewer cravings and better adherence to weight-loss plans. But, as with all medications, consulting a healthcare professional is essential to tailor the approach to your unique needs.
Feeling inspired? Many success stories highlight how individuals have transformed their bodies rapidly with this medication. To explore more about these inspiring journeys, check out real results from real people.
If you’re curious about how to safely incorporate semaglutide into your weight loss regimen, don’t hesitate to reach out to medical experts. Your journey to a healthier, faster-looking you might be just a consultation away!
Could Semaglutide Redefine Your Weight Loss Journey in 2025?
As medical science advances, so do the opportunities for faster, safer weight loss solutions. Semaglutide, an FDA-approved medication, is emerging as a game-changer in obesity treatment, especially with recent clinical breakthroughs in 2025. Its dual action of appetite suppression and enhanced fat burning makes it a promising option for those eager to see quick results without sacrificing safety.
The Science Behind Semaglutide’s Rapid Action
Semaglutide works by mimicking a natural gut hormone, GLP-1, which influences insulin secretion and satiety signals. This mechanism not only curbs hunger but also improves metabolic processes, leading to accelerated fat loss. Clinical studies, such as one highlighted in a peer-reviewed research, demonstrate that patients can lose up to 15% of their body weight within just 16 weeks—an incredible feat compared to traditional diets.
How Can 2025 Maximize Your Results?
The key to leveraging this year’s advancements lies in integrating semaglutide with tailored lifestyle changes, particularly intermittent fasting and structured exercise routines. Combining metabolic optimization with pharmacotherapy enhances outcomes while minimizing risks. Consulting with healthcare providers for doctor-supervised protocols ensures safe and effective use, especially with the new dosing guidelines that have emerged this year.
Is It Possible to Accelerate Fat Loss Without Compromising Health?
This question is at the heart of responsible weight management. Evidence suggests that when used correctly, semaglutide can significantly speed up fat burning while maintaining overall health. Its ability to reduce cravings supports adherence, making it easier to stick to dietary plans. However, individual health conditions and medication responses vary, so personalized medical guidance remains crucial. For inspiring success stories and practical tips, explore real-world results.
Are you curious about how to safely incorporate this breakthrough into your weight loss plan? Reach out to experts through our contact page and start your journey with confidence.
For deeper insights into how semaglutide accelerates fat loss, don’t forget to check out this comprehensive review.
Unlocking the Full Potential of Semaglutide: Beyond Basic Weight Loss Strategies
While the spotlight on semaglutide continues to grow, it’s crucial to understand its multifaceted role in metabolic health. Beyond appetite suppression and rapid fat reduction, emerging research suggests that semaglutide may influence gut microbiota composition, which plays a pivotal role in obesity and insulin resistance. A groundbreaking study published in The Lancet Diabetes & Endocrinology (2024) highlights how GLP-1 receptor agonists like semaglutide can modulate microbial diversity, potentially offering additional therapeutic benefits for metabolic syndrome patients.
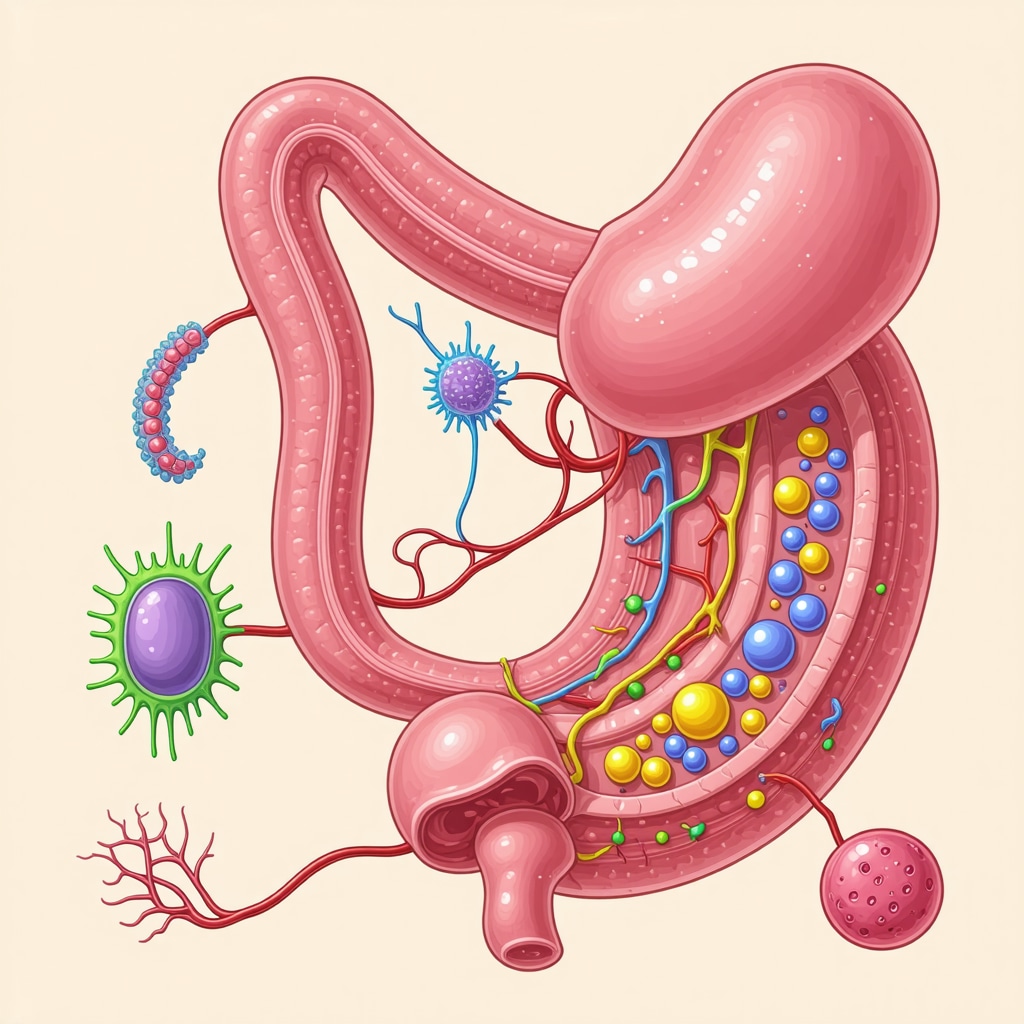
How Does Semaglutide Interact with Gut Microbiota to Enhance Weight Loss?
This sophisticated interplay involves semaglutide altering gut hormone signaling pathways, which in turn reshape the microbiome environment. These changes can lead to improved intestinal barrier function, reduced systemic inflammation, and enhanced energy expenditure. Such mechanisms might explain the sustained weight loss observed even after discontinuation of therapy in some cases. Clinicians are now considering microbiota profiling as part of personalized treatment plans to optimize outcomes.
For practitioners interested in integrating microbiome insights into their practice, current protocols recommend combining semaglutide therapy with dietary interventions rich in prebiotics and probiotics to synergize effects. This holistic approach may not only accelerate fat loss but also improve metabolic resilience in patients with complex health profiles.
The Nuanced Challenges of Dosing and Long-Term Use
Despite its promise, the application of semaglutide at an advanced level involves navigating intricate dosing regimens. Recent pharmacokinetic studies indicate that individualized titration schedules, based on genetic and metabolic markers, can mitigate side effects such as nausea or hypoglycemia. Moreover, considerations around long-term safety—particularly regarding pancreatic function and cardiovascular health—are central to ongoing clinical trials.
Importantly, expert consensus now advocates for dynamic dosing algorithms that adapt in real-time to patient response, ensuring maximal efficacy with minimized adverse events. This precision medicine approach exemplifies how endocrinology is evolving into a data-driven science, where treatment is tailored to individual biology rather than one-size-fits-all protocols.
What Are the Future Horizons for Semaglutide and Metabolic Disease?
The horizon is bright with possibilities. Researchers are exploring semaglutide’s potential in non-alcoholic fatty liver disease (NAFLD), polycystic ovary syndrome (PCOS), and even neurodegenerative conditions linked to metabolic dysfunction. These innovative directions could redefine the scope of GLP-1 receptor agonists as versatile metabolic modulators.
To stay at the forefront of this rapidly evolving field, clinicians and researchers must continuously engage with peer-reviewed journals and attend specialized conferences. The integration of genomics, microbiomics, and pharmacology promises a new era of personalized metabolic therapy—where rapid, safe, and sustainable weight management becomes universally accessible.
Curious about how these advanced strategies can be incorporated into your practice or personal health plan? Connect with specialized endocrinologists and metabolic health experts who are pioneering these innovations. Your journey toward optimized health with semaglutide might just be a consultation away.
Unlocking the Microbiome: How Semaglutide May Influence Gut Health for Enhanced Fat Loss
Emerging research indicates that semaglutide’s benefits may extend beyond appetite suppression and metabolic regulation, potentially altering the gut microbiota composition—a key player in obesity and insulin resistance. A recent study published in The Lancet Diabetes & Endocrinology (2024) highlights how GLP-1 receptor agonists can modulate microbial diversity, fostering a more resilient and metabolically favorable gut environment.
What Are the Implications of Microbiome Modulation for Long-Term Weight Management?
This interaction suggests that semaglutide’s efficacy might be bolstered by dietary strategies aimed at supporting microbiota health, such as prebiotic-rich foods and probiotic supplementation. Such an integrative approach could promote sustained weight loss even after discontinuing medication, reducing relapse rates and improving overall metabolic health. Clinicians are increasingly considering microbiome profiling to tailor interventions for optimal results, underscoring the importance of personalized medicine in obesity treatment.
For healthcare professionals interested in incorporating microbiota insights into their practice, current protocols recommend combining semaglutide therapy with dietary interventions that enhance microbial diversity. This synergy not only accelerates fat loss but also fortifies metabolic resilience against future weight regain, making the journey toward health more sustainable.
Navigating the Nuances of Dosing and Long-Term Use: Precision Medicine in Action
As the understanding of semaglutide deepens, so does the recognition that individualized dosing regimens are crucial for maximizing benefits while minimizing risks. Recent advances in pharmacogenomics allow clinicians to consider genetic and metabolic markers when titrating doses, aligning with the principles of precision medicine. This tailored approach helps mitigate side effects such as nausea or hypoglycemia, ensuring patient safety and adherence.
Moreover, long-term safety concerns—particularly regarding pancreatic function and cardiovascular health—are now at the forefront of ongoing research. The development of dynamic dosing algorithms that adapt in real-time to individual responses exemplifies how modern endocrinology is transforming into a data-driven science, personalizing therapies for each patient’s unique profile.
What Are the Future Horizons for Semaglutide in Broader Metabolic Disorders?
Looking ahead, researchers are exploring semaglutide’s potential in treating conditions such as non-alcoholic fatty liver disease (NAFLD), polycystic ovary syndrome (PCOS), and even neurodegenerative disorders linked to metabolic dysfunction. These innovative applications could expand the therapeutic scope of GLP-1 receptor agonists, positioning them as versatile tools in metabolic medicine.
Staying abreast of these developments requires continuous engagement with peer-reviewed journals and participation in specialized conferences. The convergence of genomics, microbiomics, and pharmacology heralds a new era where rapid, safe, and sustainable weight management becomes accessible to all. Interested practitioners and patients alike should consider consulting with endocrinologists and metabolic health experts pioneering these advancements, as personalized strategies will likely define the future of obesity treatment.
Expert Insights & Advanced Considerations
1. Precision Medicine is the Future of Weight Management
Emerging research emphasizes tailoring semaglutide treatments based on genetic and metabolic profiles. Personalized dosing and monitoring can optimize outcomes while minimizing side effects, representing a significant leap forward in obesity therapy.
2. Gut Microbiota Modulation Enhances Long-Term Results
Semaglutide’s influence on gut microbiota diversity offers promising avenues for sustained weight loss. Combining pharmacotherapy with dietary strategies that support microbiome health, such as prebiotics and probiotics, could reduce relapse rates and improve metabolic resilience.
3. Integrating Microbiome Profiling in Clinical Practice
Practitioners are now considering microbiota profiling as part of a comprehensive approach. This enables more precise interventions and opens new possibilities for managing obesity and related metabolic disorders.
4. Dynamic Dosing Algorithms Powering Safety and Efficacy
Advances in pharmacogenomics facilitate real-time dose adjustments, ensuring maximum benefit while safeguarding patient health. Such data-driven, adaptive protocols exemplify the evolution of endocrinology into a personalized science.
5. Expanding Therapeutic Horizons
Research into semaglutide’s potential in treating NAFLD, PCOS, and neurodegenerative diseases suggests a versatile future. These innovative applications could redefine the scope of metabolic medicine in the coming years.
Curated Expert Resources
- ClinicalTrials.gov: An authoritative database for ongoing and completed clinical trials, offering detailed information on semaglutide studies, including dosing, safety, and efficacy data.
- The Lancet Diabetes & Endocrinology (2024): A peer-reviewed journal publishing cutting-edge research on microbiome modulation and metabolic therapies, essential for staying updated on innovative findings.
- FDA Official Website: The definitive source for approved indications, safety guidelines, and updates on semaglutide and related treatments, ensuring clinical compliance and informed decision-making.
- Endocrinology Journals and Conferences: Platforms like the Journal of Clinical Endocrinology & Metabolism and professional events provide insights into evolving personalized treatment strategies and future directions.
Final Expert Perspective
As we advance into 2025, the integration of semaglutide into personalized metabolic health strategies exemplifies the power of precision medicine. Its multifaceted role in rapid weight loss, microbiome modulation, and expanding therapeutic horizons signals a new era where science and individualized care converge. For clinicians and patients alike, staying informed through authoritative sources and embracing innovative approaches will be crucial. If you’re ready to explore these cutting-edge strategies further or contribute your insights, engaging with expert networks and research communities can accelerate your journey toward optimal health. The future of rapid, safe, and sustainable weight management is here—are you prepared to be part of it?


This post provides a comprehensive overview of semaglutide’s emerging role in rapid weight loss, especially with the latest clinical data from 2025. I find it fascinating how the integration of microbiome research is opening up new avenues for personalized treatment approaches. Having seen patients struggle with traditional diets and lifestyle changes, the prospect of combining pharmacotherapy with microbiota-focused strategies is promising for sustainable outcomes. However, I wonder about the practical implementation—how feasible is microbiome profiling in general clinical practice at this stage? Also, considering the long-term safety concerns, especially regarding pancreatic function, what should patients and clinicians be most vigilant about during extended therapy? I believe ongoing research and real-world evidence will be vital in shaping best practices. I’d love to hear from professionals who are already adopting such integrated approaches—what hurdles have you encountered, and how are you addressing them?