Unlocking the Science Behind Fast Acting Semaglutide for Rapid Weight Loss
In 2025, the quest for effective, fast-acting weight loss solutions has taken a promising turn with semaglutide, a groundbreaking injectable medication originally developed for diabetes management. Its remarkable ability to curb appetite and accelerate fat loss is revolutionizing medical weight loss programs. Unlike traditional diets that often demand grueling discipline and yield slow results, semaglutide works by mimicking the glucagon-like peptide-1 (GLP-1) hormone, enhancing satiety and reducing cravings, thus offering a strategic advantage for fast fat burning.
Injectable Breakthrough: How Semaglutide Transforms Fat Loss Strategies
Semaglutide’s mode of action is nuanced yet highly effective. By binding to GLP-1 receptors in the brain, it modulates hunger signals and delays gastric emptying. This dual effect creates a natural reduction in calorie intake without the psychological strain typical of calorie-restrictive diets. Clinical studies, such as those reviewed by the New England Journal of Medicine, have demonstrated weight reductions averaging 15% or more within months when combined with lifestyle adjustments, making semaglutide a formidable tool for quick weight loss in 2025.
Synergizing Semaglutide with Lifestyle: What Maximizes Your Weight Loss Journey?
While semaglutide is potent alone, its effectiveness multiplies when paired with scientifically backed dietary strategies. For example, intermittent fasting protocols can harmonize with semaglutide’s appetite suppression to enhance fat burning and metabolic efficiency. Experts recommend integrating low-calorie, nutrient-dense meals during eating windows to sustain energy and prevent nutrient deficiencies. Want to explore the best semaglutide diet plans tailored for rapid fat loss? Check out our comprehensive guide on best semaglutide diet plans to support rapid weight loss in 2025.
How Quickly Can You Expect Results With Fast Acting Semaglutide?
Weight loss timelines vary by individual, but many patients report noticeable decreases in appetite and initial weight drops within the first 2 to 4 weeks of semaglutide treatment. By week 12, substantial fat loss is commonly observed, especially under medical supervision that ensures optimized dosing and lifestyle alignment. It’s important to understand that while semaglutide accelerates fat loss, sustainable results depend on consistent adherence to prescribed regimens and healthy habits. For detailed medical guidance, see our expert-reviewed doctor supervised semaglutide safe dosage guidelines.
Real-Life Transformations: Experience Speaks Louder Than Promises
Consider the case of Jane, a 45-year-old who struggled with persistent weight plateaus despite rigorous dieting. After beginning a medically supervised semaglutide program, she experienced a 20-pound loss within three months, coupled with improved energy and reduced binge-eating episodes. Her story, among many others, underscores the medication’s practical impact beyond clinical data. These inspiring testimonials can be explored further at real semaglutide success stories.
What Are the Key Considerations Before Starting Semaglutide?
Despite its efficacy, semaglutide is not a universal solution. Potential side effects like nausea and gastrointestinal discomfort can occur, especially during dosage escalation. Therefore, professional medical supervision is vital to tailor treatment and manage adverse effects. Additionally, semaglutide is contraindicated in individuals with certain thyroid conditions or personal/family history of medullary thyroid carcinoma, underscoring the importance of thorough medical evaluation prior to treatment.
Ready to take the next step in your weight loss journey? Contact our medical experts for personalized semaglutide treatment plans designed for rapid and safe fat loss.
Balancing Expectations: What I Learned About Semaglutide’s Pace and Persistence
When I first embarked on my semaglutide journey, I was excited by the prospect of rapid weight loss. However, what became clear over time is the importance of patience and gradual progress. While some experience swift results, others, like myself, notice a slower but steadier transformation. This taught me that semaglutide isn’t a magic wand but a catalyst that works best when combined with consistent lifestyle changes.
For instance, the initial weeks were marked by mild nausea and a fluctuating appetite, which my healthcare provider helped me manage through careful dose adjustments. These nuances made me appreciate the significance of doctor supervision — it’s not just about getting the drug but optimizing its use safely. If you want to dive deeper into safe and effective usage, doctor supervised semaglutide safe dosage guidelines provide invaluable insights.
Integrating Semaglutide with Everyday Habits: Small Changes, Big Impact
One key realization I had was how semaglutide enhanced my ability to make healthier choices effortlessly. With reduced cravings and a feeling of fullness, I found it easier to embrace balanced meals and control portion sizes. However, I also learned that pairing semaglutide with mindful eating and regular physical activity amplified its benefits.
For example, combining semaglutide with intermittent fasting created a powerful synergy that optimized fat burning. The fasting windows aligned naturally with the medication’s appetite-suppressing effects, making hunger pangs less daunting. If you’re curious about protocols that marry these two approaches effectively, our article on semaglutide and intermittent fasting best practices for fat loss offers practical guidance.
What Are the Real Challenges and How Can You Overcome Them?
Despite the promising science and my positive experience, I won’t sugarcoat that semaglutide comes with challenges. Side effects such as nausea, fatigue, and occasional digestive discomfort were part of my journey. It took time to adjust and find a routine that minimized these issues. Engaging openly with my healthcare team was crucial — it reminded me that personalized care is key.
Moreover, understanding that semaglutide is not a standalone fix but part of a holistic weight loss strategy helped me stay grounded. The medication supports, but doesn’t replace, the need for balanced nutrition and activity. According to a review in the National Institutes of Health, combining pharmacotherapy with lifestyle interventions yields the best long-term outcomes in weight management.
Have You Experienced Semaglutide? Share Your Story!
Weight loss journeys are deeply personal and unique. If you’re currently using semaglutide or considering it, I’d love to hear about your experiences, challenges, or questions. Sharing insights helps build a supportive community where we learn from each other’s paths.
Feel free to reach out or comment below with your story. Also, explore more inspiring transformations and expert tips in our real semaglutide success stories to keep motivated on your journey.
Optimizing Semaglutide Dosing: Precision Medicine Approaches for Enhanced Weight Loss Efficacy
While standard semaglutide protocols recommend gradual dose escalation to mitigate side effects, personalized dosing strategies are emerging as a frontier in maximizing therapeutic outcomes. Pharmacogenomic variations influence individual responses to GLP-1 receptor agonists, suggesting that tailoring dose increments based on genetic markers and metabolic profiling could optimize appetite suppression and minimize adverse events.
Recent clinical explorations have highlighted the potential of adaptive dosing regimens where real-time feedback on hunger scales, gastrointestinal tolerance, and metabolic parameters inform titration speed. This bespoke approach not only enhances patient adherence but also supports sustained weight loss beyond the typical 12- to 16-week window.
How can genetic and metabolic profiling refine semaglutide dose personalization?
Genetic polymorphisms affecting GLP-1 receptor expression and downstream signaling pathways modulate patient sensitivity to semaglutide. For example, variants in the GLP1R gene may predict differential appetite control and gastrointestinal side effect profiles. Metabolic markers such as baseline insulin resistance and gut hormone milieu further inform expected responsiveness.
Integrating such biomarkers into clinical decision-making facilitates a stratified medicine model, enabling clinicians to identify candidates who may benefit from accelerated dose escalation or require slower titration to manage tolerance. This precision approach aligns with recent findings published in Nature Medicine (2023) emphasizing biomarker-guided interventions for obesity pharmacotherapy.
Neuroendocrine Interactions: Unveiling Semaglutide’s Influence on Central Appetite Circuits Beyond GLP-1
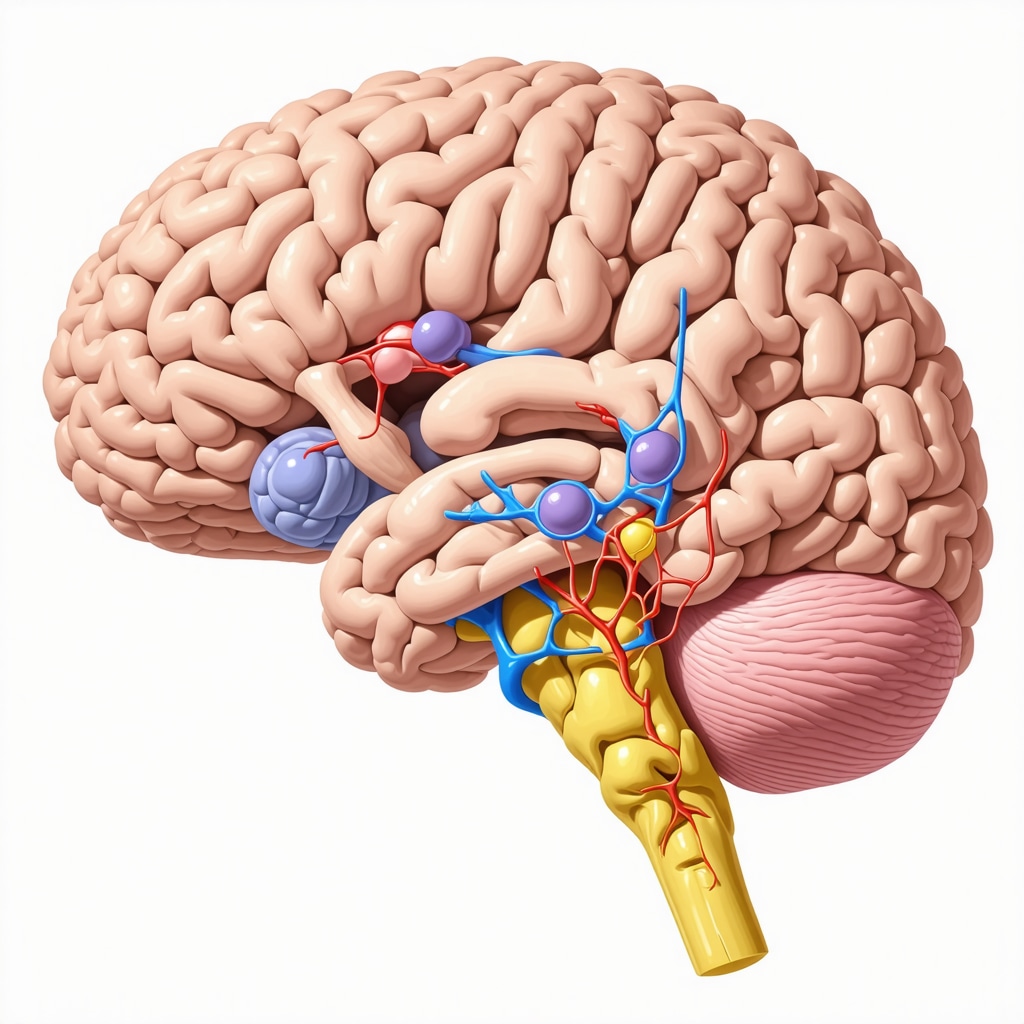
Semaglutide’s anorectic effects extend beyond classical GLP-1 receptor activation, engaging a complex web of neuroendocrine pathways that regulate hunger and energy expenditure. Emerging neuroimaging studies reveal that semaglutide modulates activity in hypothalamic nuclei, including the arcuate nucleus and paraventricular nucleus, which integrate peripheral signals like leptin and insulin.
This crosstalk leads to suppression of orexigenic neurons, such as those producing neuropeptide Y (NPY) and agouti-related peptide (AgRP), while enhancing anorexigenic signals from pro-opiomelanocortin (POMC) neurons. The result is a coordinated downregulation of appetite and an increase in energy utilization, contributing to the medication’s potent fat loss effects.
Addressing Long-Term Weight Maintenance: Strategies to Sustain Semaglutide-Induced Fat Loss
One critical challenge in obesity management is the common phenomenon of weight regain after cessation of pharmacotherapy. Semaglutide’s effects on appetite regulation and metabolism are profound but may wane if treatment stops prematurely. Therefore, establishing maintenance strategies is essential to solidify gains.
Approaches include gradual dose tapering combined with behavioral interventions that reinforce dietary mindfulness and physical activity. Additionally, adjunctive therapies targeting complementary pathways, such as SGLT2 inhibitors or amylin mimetics, are under investigation to support weight maintenance post-semaglutide.
Longitudinal studies underscore the importance of ongoing medical follow-up to detect and address metabolic adaptations that predispose to weight rebound, ensuring that the initial rapid fat loss translates into durable health benefits.
Integrating Semaglutide into Comprehensive Metabolic Health Programs: Beyond Weight Loss
Weight loss is often the initial goal, but the broader metabolic improvements conferred by semaglutide warrant attention. Semaglutide improves glycemic control, lipid profiles, and inflammatory markers, thus reducing cardiovascular risk factors commonly associated with obesity.
Incorporating semaglutide into multidisciplinary metabolic clinics allows for synchronized management of comorbidities such as type 2 diabetes, hypertension, and non-alcoholic fatty liver disease. Such holistic care models enhance patient outcomes beyond the scale, addressing root causes of metabolic dysfunction.
For clinicians and patients seeking to harness semaglutide’s full potential, exploring integrative protocols and continuous metabolic monitoring is advisable. Our expert team is available to guide you through personalized program design tailored to your unique health profile.
Ready to elevate your fat loss journey with cutting-edge, science-backed strategies? Connect with our specialists today for individualized semaglutide optimization and metabolic health planning.

Precision Medicine in Semaglutide Therapy: Tailoring Dosage for Optimal Outcomes
Recent advances in obesity pharmacotherapy have spotlighted the importance of individualized semaglutide dosing strategies. Beyond conventional dose escalation, leveraging genetic and metabolic profiling allows clinicians to customize titration schedules that maximize efficacy while minimizing adverse effects. Such precision medicine approaches consider polymorphisms in the GLP1R gene and metabolic biomarkers like insulin sensitivity, facilitating a nuanced understanding of patient responsiveness.
Adaptive dosing protocols guided by real-time monitoring of appetite suppression and gastrointestinal tolerance represent a paradigm shift, enabling sustained adherence and enhanced weight loss beyond typical treatment durations.
How can genetic and metabolic profiling refine semaglutide dose personalization?
Exploring the interplay between genetic variants and metabolic status illuminates why semaglutide’s appetite-suppressing effects and side effect profiles vary among individuals. For instance, patients with specific GLP1R polymorphisms may experience differential receptor sensitivity, influencing therapeutic response and gastrointestinal tolerability. Integrating these insights into clinical practice empowers stratified dosing regimens, optimizing treatment outcomes as emphasized in the Nature Medicine (2023) study on biomarker-guided obesity pharmacotherapy.
Neuroendocrine Dynamics: Semaglutide’s Multidimensional Appetite Modulation
Semaglutide orchestrates complex neuroendocrine interactions beyond GLP-1 receptor activation, engaging hypothalamic networks integral to energy homeostasis. Functional neuroimaging reveals modulation of arcuate and paraventricular nuclei, where suppression of orexigenic neuropeptides such as NPY and AgRP coincides with enhanced anorexigenic POMC signaling. This multifaceted neural regulation not only diminishes hunger but also promotes increased energy expenditure, a dual mechanism critical for effective fat loss.
Sustaining Fat Loss: Long-Term Strategies Post Semaglutide Treatment
The challenge of weight regain post-pharmacotherapy necessitates strategic maintenance planning. Gradual dose tapering combined with robust behavioral interventions—emphasizing dietary mindfulness and physical activity—can consolidate weight loss. Emerging adjunctive pharmacotherapies targeting complementary metabolic pathways are under investigation to support durable outcomes. Continuous monitoring for metabolic adaptations is imperative to preempt rebound weight gain, ensuring longevity of semaglutide-induced benefits.
Beyond Weight Loss: Integrating Semaglutide into Comprehensive Metabolic Care
Semaglutide’s therapeutic impact extends to improving glycemic control, lipid metabolism, and systemic inflammation, thereby mitigating cardiovascular risk factors prevalent in obesity. Incorporating semaglutide within multidisciplinary metabolic health programs enables holistic disease management encompassing type 2 diabetes, hypertension, and non-alcoholic fatty liver disease. This integrative paradigm fosters superior patient outcomes by addressing the multifactorial nature of metabolic dysfunction.
For tailored guidance on optimizing semaglutide therapy within broader metabolic frameworks, connect with our specialists today and harness cutting-edge, evidence-based strategies designed to elevate your therapeutic journey.
Frequently Asked Questions (FAQ)
What is semaglutide and how does it aid in rapid weight loss?
Semaglutide is a GLP-1 receptor agonist originally developed for type 2 diabetes management. It promotes rapid weight loss by mimicking the glucagon-like peptide-1 hormone, which reduces appetite, slows gastric emptying, and modulates central appetite circuits, resulting in decreased calorie intake and enhanced fat burning.
How quickly can I expect to see weight loss results with semaglutide?
Most individuals notice appetite suppression and initial weight loss within 2 to 4 weeks of starting semaglutide. Significant fat loss, often around 15% or more of body weight, is typically observed by 12 weeks when combined with lifestyle modifications and under medical supervision.
Are there common side effects, and how can they be managed?
Common side effects include nausea, fatigue, and gastrointestinal discomfort, especially during dose escalation. These symptoms often diminish over time. Managing side effects involves gradual dose titration, close medical supervision, and personalized adjustments to optimize tolerance.
Is semaglutide suitable for everyone seeking weight loss?
No. Semaglutide is contraindicated in individuals with a history of medullary thyroid carcinoma, multiple endocrine neoplasia syndrome type 2, or certain thyroid conditions. A thorough medical evaluation is essential to determine suitability and safely tailor treatment.
Can semaglutide be combined with other weight loss strategies?
Yes. Semaglutide’s effectiveness increases when combined with dietary strategies such as intermittent fasting and nutrient-dense, low-calorie meals, as well as regular physical activity. Integration into comprehensive metabolic health programs further optimizes outcomes.
How does genetic and metabolic profiling influence semaglutide dosing?
Genetic variations, particularly in the GLP1R gene, and metabolic markers like insulin sensitivity affect individual responsiveness and side effect profiles. Profiling these factors enables personalized dose titration to maximize efficacy and minimize adverse effects, embodying precision medicine in obesity pharmacotherapy.
What neuroendocrine mechanisms underlie semaglutide’s appetite suppression?
Semaglutide modulates hypothalamic nuclei by suppressing orexigenic neurons producing neuropeptide Y (NPY) and agouti-related peptide (AgRP), while enhancing anorexigenic pro-opiomelanocortin (POMC) neuron activity. This coordinated neuroendocrine regulation decreases hunger and increases energy expenditure.
How can weight loss be sustained after discontinuing semaglutide?
Weight maintenance requires gradual dose tapering, continued adherence to behavioral interventions emphasizing mindful eating and physical activity, and potentially adjunctive pharmacotherapies targeting complementary metabolic pathways. Ongoing medical monitoring is critical to prevent rebound weight gain.
Beyond weight loss, what metabolic benefits does semaglutide provide?
Semaglutide improves glycemic control, lipid metabolism, and reduces systemic inflammation, thereby lowering cardiovascular risk factors. Its integration into multidisciplinary metabolic care supports holistic management of obesity-related comorbidities such as type 2 diabetes and non-alcoholic fatty liver disease.
Where can I find expert guidance for semaglutide treatment plans?
Consulting specialized medical providers experienced in obesity pharmacotherapy is recommended. Personalized plans should include safe dosing schedules, lifestyle integration, and continuous monitoring. Our expert team is available for individualized semaglutide optimization and metabolic health programming.
Trusted External Sources
- New England Journal of Medicine (NEJM) – Provides seminal clinical trial data on semaglutide’s efficacy and safety in weight management, adding robust evidence to pharmacotherapy approaches.
- Nature Medicine (2023) – Features cutting-edge research on biomarker-guided precision dosing of GLP-1 receptor agonists, advancing personalized obesity treatments.
- National Institutes of Health (NIH) – National Library of Medicine – Offers comprehensive reviews on obesity pharmacotherapy, integrating pharmacological and behavioral strategies for sustainable weight loss.
- Endocrine Society Clinical Practice Guidelines – Authoritative recommendations on obesity management including pharmacotherapy protocols and contraindications.
- American Diabetes Association (ADA) – Provides insights into metabolic benefits of GLP-1 receptor agonists beyond glycemic control, supporting integrated metabolic health care.
Conclusion
Fast acting semaglutide represents a transformative advancement in weight loss pharmacotherapy, leveraging sophisticated neuroendocrine mechanisms to suppress appetite and promote sustained fat loss. Its integration with personalized dosing strategies, informed by genetic and metabolic profiling, marks a new era of precision medicine in obesity care. While semaglutide offers rapid and substantial results, long-term success hinges on combining pharmacological intervention with holistic lifestyle changes and ongoing medical support. Beyond shedding pounds, semaglutide contributes to comprehensive metabolic health improvements, underscoring its role within multidisciplinary treatment frameworks. Embracing these evidence-based insights empowers individuals and clinicians to optimize fat loss journeys safely and effectively. Ready to take your weight management to the next level? Share your experiences, ask questions, and explore our expert resources to harness the full potential of semaglutide today.


Reading about semaglutide’s ability to mimic GLP-1 hormone and naturally suppress appetite is fascinating. I appreciate how it provides a more physiological approach to weight loss rather than just focusing on calorie cutting, which can be mentally exhausting. In my experience, the hardest part of dieting has always been managing constant hunger and cravings, so something that targets those signals directly seems promising. The article’s points about semaglutide delaying gastric emptying and communicating with brain receptors offer solid insight into why it feels different from traditional diet methods. However, I wonder about the balance between relying on a medication like this and developing sustainable habits. While semaglutide seems to provide a helpful head start, does anyone here have experience maintaining weight loss after stopping it? Also, how do you think this approach compares to newer lifestyle interventions focused solely on holistic behavioral change? It would be great to hear others’ perspectives on integrating these new pharmacological tools with long-term health strategies.