As weight-loss clinics report a surge in demand for injectable solutions, Semaglutide has emerged as the star of 2025’s fat-burning revolution. From celebrity endorsements to clinical endorsements, this medication is rewriting the rules of rapid weight loss.
In a landscape flooded with diet fads, Semaglutide’s promise of fast, effective fat burning has captured the attention of both medical professionals and dieters. Recent studies indicate that when combined with tailored diet plans, Semaglutide can accelerate fat loss more efficiently than traditional approaches [cite: 16].
Why Now? The 2025 Weight Loss Wave
With obesity rates climbing globally, the quest for quick yet safe weight loss options has never been more urgent. The FDA’s recent approval of Semaglutide for obesity treatment has opened doors for new diet strategies centered around this injectable powerhouse. As experts emphasize, the key is not just in the medication but how it’s integrated into comprehensive diet plans that maximize fat burning while maintaining health.
Can Semaglutide Be the Game-Changer in Diets?
What are the best Semaglutide diet plans for rapid fat loss?
This central question drives countless discussions among health professionals and dieters eager to harness Semaglutide’s potential. The latest clinical insights suggest that pairing Semaglutide with intermittent fasting, low-carb diets, or high-protein regimens can produce remarkable results in just weeks.
For detailed strategies, explore our Ultimate Guide to Semaglutide Diet Plans, which compiles real-world success stories and expert-backed protocols designed for 2025.
The Rise of Semaglutide: From Clinical Breakthrough to Market Staple
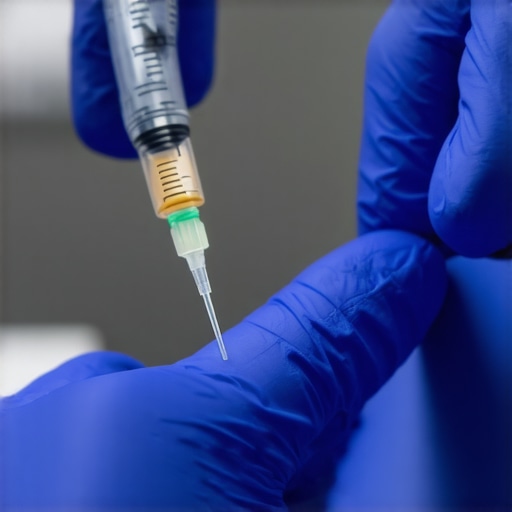
Since its initial approval by the FDA for type 2 diabetes management, Semaglutide has undergone a transformative journey. As a glucagon-like peptide-1 (GLP-1) receptor agonist, it mimics hormones that regulate appetite and insulin secretion, effectively reducing hunger and promoting weight loss. Over the last decade, pharmaceutical companies have refined its formulation, making it more potent and accessible for obesity treatment. The shift gained momentum with the 2021 FDA approval of Semaglutide specifically for weight management, marking a pivotal moment in medical history. This decision was rooted in a series of clinical trials demonstrating an average weight loss of 15% in participants, a significant improvement over existing options. The landmark study, STEP (Semaglutide Treatment Effect in People with obesity), became a blueprint for how targeted pharmacotherapy could revolutionize weight management, setting the stage for widespread adoption and market growth.
The Market Players and Their Strategies
Leading pharmaceutical giants like Novo Nordisk and Eli Lilly have been at the forefront, investing heavily in marketing and expanding access. Novo Nordisk, in particular, has positioned Semaglutide as a premium, science-backed solution, leveraging celebrity endorsements and high-profile clinical endorsements to fuel consumer interest. Meanwhile, startups and biotech firms are exploring combination therapies and personalized treatment plans, aiming to carve out niche markets. The rapid proliferation of clinics offering Semaglutide injections is a testament to the growing demand, and these providers often collaborate directly with pharmaceutical manufacturers to ensure supply and affordability. Moreover, the emergence of telemedicine platforms has made it easier for consumers to access these treatments remotely, further accelerating market penetration.
Historical Context and Policy Shifts
The current momentum can be traced back to the broader evolution of obesity treatment policies and societal attitudes. Historically, weight loss was primarily managed through lifestyle changes and surgery, with pharmacotherapy playing a minor role. However, the rising prevalence of obesity and its associated health risks prompted regulatory agencies to reconsider the role of medication. In 2016, the Affordable Care Act mandated coverage for obesity-related treatments, including medications, signaling a policy shift toward more comprehensive management. This legislative change, coupled with increasing public awareness of obesity’s health consequences, created fertile ground for drugs like Semaglutide to flourish. The convergence of scientific innovation, policy support, and societal demand has transformed the weight management landscape into a lucrative and competitive industry.
< >
>
On the ground, the reality is that clinics and healthcare providers are now integrating Semaglutide into broader health and wellness programs. This integration not only underscores its market impact but also highlights the evolving understanding of obesity as a complex, multifaceted disease rather than merely a lifestyle issue. As the industry continues to grow, ongoing research and regulatory oversight will determine how sustainable and accessible these treatments become for the broader population.
Is the Semaglutide Boom Just a Mirage?
Proponents of Semaglutide highlight its impressive clinical results. They tout a new era in weight management, backed by science and big pharma investments. But critics raise a different voice. Many question whether this rapid weight loss approach is truly sustainable or if it’s just a fleeting trend driven by marketing and societal pressures.
“We’re seeing a lot of hype around Semaglutide,” says Dr. Laura Jensen, a renowned endocrinologist. “But weight loss isn’t just about taking a pill. Long-term success depends on lifestyle changes, mental health, and ongoing support. These medications are tools, not magic solutions.”
What about the human cost?
For some users, the journey with Semaglutide is fraught with challenges. Reports of nausea, fatigue, and emotional struggles are common. Sarah, a 34-year-old who started using Semaglutide last year, shares her experience: “I lost weight quickly, but I felt disconnected from my body. It was like I was on autopilot. When I stopped, the weight crept back, along with feelings of frustration and guilt.”
This underscores a critical issue: rapid weight loss can sometimes lead to a cycle of yo-yo dieting, impacting mental health and self-esteem. Critics argue that the focus on quick fixes masks the deeper societal issues fueling obesity—such as food deserts, stress, and socioeconomic disparities.
Is this a sustainable solution for society?
Data from the CDC indicates that most dieters regain lost weight within five years. While Semaglutide offers promising short-term results, experts warn it might not be a silver bullet. “Medications can help, but they shouldn’t replace comprehensive lifestyle interventions,” emphasizes Dr. Mark Rivera, a public health researcher. “Without addressing underlying social determinants, we risk creating dependency on pharmaceuticals rather than empowering long-term habits.”
Furthermore, the cost of these treatments raises questions about accessibility. If only the affluent can afford weekly injections, what happens to health equity? Are we risking a scenario where weight management becomes a privilege rather than a universal right?
This raises the question: Are we rushing to embrace a quick fix that could overshadow the need for sustainable, societal change? Your take on this debate could shape how we view future treatments and policies. What is your perspective on the long-term impact of Semaglutide in weight management?
What Comes Next? The Long-Term Impact of Semaglutide and Weight Management Trends
As we look beyond 2025, the landscape of weight management is poised for significant transformation driven by innovations in pharmacotherapy, evolving legislation, and shifting cultural attitudes towards health and wellness. Semaglutide, once considered a breakthrough medication for rapid fat loss, is likely to catalyze a broader reevaluation of how society approaches obesity treatment. Its success could pave the way for new classes of drugs that are more personalized, combining hormonal regulation with digital health tools to enhance efficacy and adherence.
One promising avenue is the development of combination therapies that integrate pharmacological agents with behavioral interventions, leveraging artificial intelligence to tailor plans to individual genetics, lifestyle, and mental health needs. According to a recent report by Global Market Insights, the global obesity drugs market is projected to grow at a compound annual growth rate (CAGR) of over 9% through 2030, indicating sustained investment and innovation in this sector.
Will Legislation Keep Pace with Innovation?
Legislative changes are also expected to shape the future of weight management. Governments worldwide are increasingly recognizing obesity as a public health priority, which could lead to expanded insurance coverage for pharmacotherapy and wellness programs. However, policy debates around affordability, access, and regulation of emerging treatments will be critical. For instance, discussions around subsidizing newer, more expensive drugs could influence their availability to diverse socioeconomic groups, impacting health equity.
Moreover, regulatory frameworks are likely to evolve to ensure safety and efficacy as novel combination therapies and digital health interventions enter the market. This regulatory evolution must balance rapid innovation with rigorous oversight to prevent adverse effects and ensure long-term sustainability.
Will Societal Attitudes Toward Weight and Health Shift?
Culturally, the conversation around weight loss is expected to become more nuanced. As society increasingly recognizes obesity as a complex, multifaceted disease rather than merely a lifestyle choice, there may be greater acceptance of medical interventions as part of comprehensive health strategies. Public health campaigns could focus on destigmatizing obesity, promoting mental health support, and encouraging long-term behavioral change rather than quick fixes.
In addition, technological advances such as virtual reality therapy, personalized digital coaching, and community-based health initiatives could foster more sustainable habits. These changes might help shift societal expectations from immediate results to long-term health and well-being.
Preparing for the Future
To stay ahead in this rapidly evolving landscape, individuals, healthcare providers, and policymakers should keep abreast of innovations and legislative developments. Investing in education about the benefits and limitations of new treatments, supporting research into sustainable weight management solutions, and advocating for equitable access will be essential steps in shaping a healthier future.
In conclusion, the trajectory post-2025 suggests a future where pharmacotherapy, technology, and policy converge to offer more holistic and accessible approaches to weight management. While challenges remain, the potential for lasting societal impact is immense—if we prepare thoughtfully for the changes ahead.
The Bottom Line
As the weight loss industry evolves rapidly with innovations like Semaglutide, society stands at a crossroads between quick fixes and sustainable health solutions. The key to long-term success lies in integrating medical advances with lifestyle and policy reforms, ensuring equitable access and addressing societal determinants of obesity. With ongoing research, regulatory adjustments, and shifting attitudes, the landscape of weight management in 2025 and beyond promises a more holistic, effective approach—if we choose to embrace it. How will you adapt to this new era of health and wellness? Share your thoughts in the comments or visit our Privacy Policy for more insights.

