Unlocking the Science Behind Semaglutide’s Weight Loss Magic
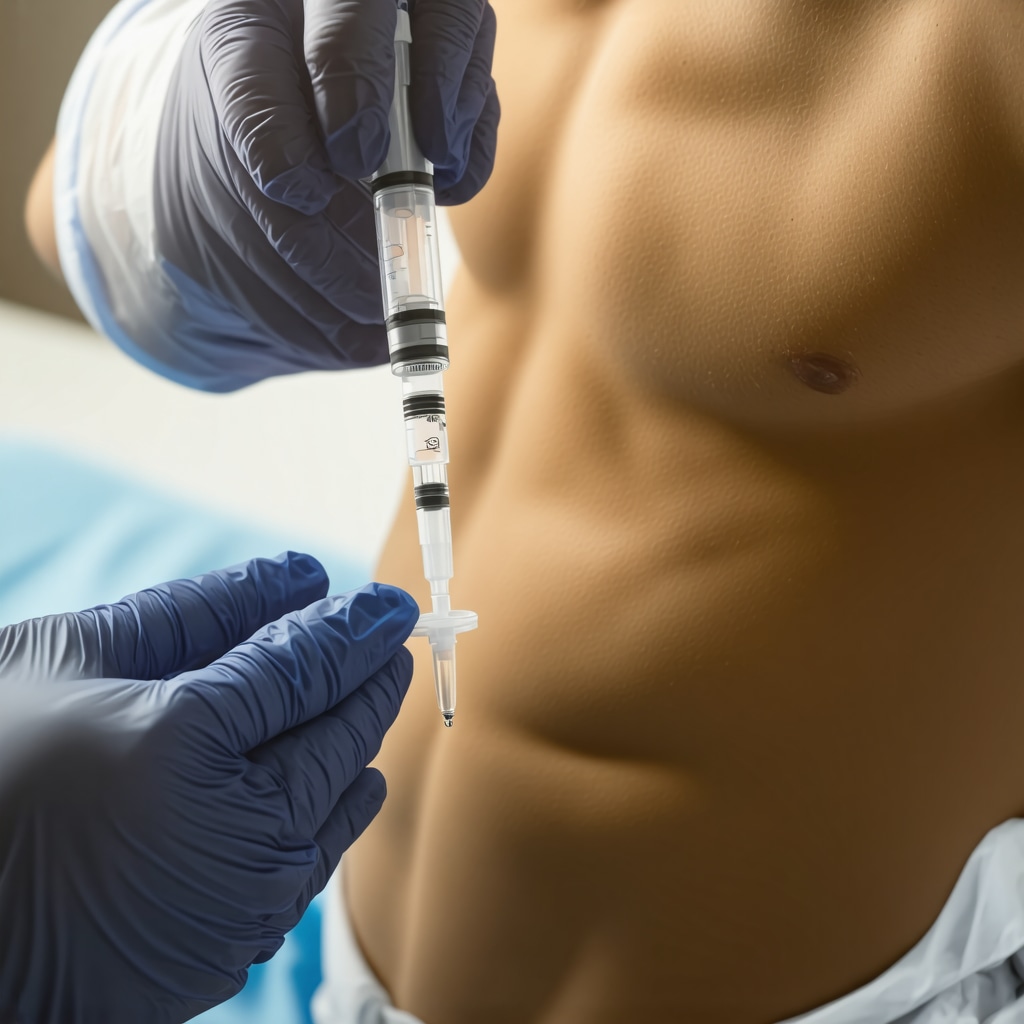
In the evolving landscape of weight management, semaglutide injections have emerged as a revolutionary tool, offering rapid yet safe fat loss for those battling obesity or stubborn weight. Unlike traditional diets or exercise alone, this injectable medication harnesses a sophisticated biochemical mechanism that targets appetite regulation and metabolic efficiency, reshaping how we approach weight loss.
Decoding the Biological Symphony: How Semaglutide Acts Within Your Body
Semaglutide is a glucagon-like peptide-1 (GLP-1) receptor agonist. By mimicking the hormone GLP-1, it influences the brain’s appetite centers, reducing hunger and promoting a feeling of fullness after eating smaller meals. This hormonal mimicry not only curbs caloric intake but also slows gastric emptying, which prolongs satiety. Additionally, semaglutide enhances insulin secretion in response to meals and suppresses glucagon, stabilizing blood sugar levels — a critical factor in metabolic health that indirectly supports sustained weight reduction.
What Makes Semaglutide Injections a Safe Option for Rapid Weight Loss?
Safety is paramount in any weight loss intervention, especially one promising rapid results. Semaglutide’s approval by the FDA for obesity treatment (source: FDA official site) followed extensive clinical trials demonstrating a favorable safety profile when administered under medical supervision. Common side effects such as nausea or mild gastrointestinal discomfort tend to diminish over time, and dosing is carefully titrated to minimize risks. Moreover, its weekly injection schedule enhances adherence and allows close monitoring by healthcare professionals, ensuring personalized, safe weight loss progression.
Harnessing Semaglutide with Lifestyle Synergy: Beyond the Injection
The transformative power of semaglutide is most effective when paired with a balanced lifestyle. This includes mindful dietary choices that complement appetite suppression and promote nutritional adequacy, alongside regular physical activity that enhances metabolic health. For those interested in optimizing their approach, exploring semaglutide combined with intermittent fasting offers compelling evidence of accelerated fat loss while maintaining safety.
Real-World Experiences: Semaglutide’s Impact on Weight Loss Journeys
Consider the case of individuals who struggled for years with traditional weight loss methods yet achieved substantial results with semaglutide injections under medical guidance. These experiences highlight not only impressive fat reduction but also improved metabolic markers and quality of life. Detailed accounts and clinical results can be explored further at real semaglutide success stories, showcasing the drug’s transformative potential when combined with expert supervision.
Optimizing Your Journey: Expert Tips on Safe Dosage and Administration
Administering semaglutide safely involves gradual dosage escalation, starting with low doses to minimize side effects and carefully increasing to therapeutic levels under medical supervision. Techniques for injection, timing, and storage are crucial for efficacy and safety, aspects covered comprehensively in expert dosage and safety guidelines. Patients are encouraged to maintain regular consultations to tailor treatment, monitor progress, and adjust lifestyle factors accordingly.
Join the Conversation: Share Your Semaglutide Weight Loss Experience
Have you or someone you know embarked on a weight loss journey with semaglutide injections? Sharing real-life insights and questions enriches the community’s understanding and empowers others considering this path. Leave a comment below or share this article with friends seeking safe, effective weight loss solutions.
Embracing the Emotional Journey Alongside Semaglutide Treatment
When I first started my semaglutide injections, I didn’t just notice physical changes; there was an emotional shift too. The reduction in hunger pangs gave me a newfound sense of control that I hadn’t felt in years. However, it also meant I had to reframe my relationship with food, which was as much psychological as it was physical. It’s important to acknowledge that rapid weight loss, even when medically guided, can stir up complex feelings—from excitement and motivation to moments of vulnerability. Being mindful of this emotional landscape helped me stay grounded and persistent throughout my journey.
Practical Strategies: Balancing Semaglutide With Everyday Life
One of the biggest challenges I faced was integrating the weekly injections into my busy schedule. I found that setting a consistent day and time each week for my semaglutide shot created a reliable routine, making adherence easier. Pairing this with a thoughtfully designed diet plan was key. I gravitated toward nutrient-dense foods that complemented semaglutide’s appetite-suppressing effects, avoiding processed snacks that once felt irresistible. Also, listening to my body’s signals became crucial—sometimes I needed to rest more or adjust my activity levels, especially in the early weeks.
Could semaglutide change how you experience hunger and cravings?
From my experience and conversations with others on this path, semaglutide does fundamentally alter hunger cues. The drug’s influence on the brain’s appetite centers means cravings become less frequent and intense, which is empowering. Yet, it’s not a magic button; mindful eating and lifestyle choices remain essential. According to a recent review published in The New England Journal of Medicine, semaglutide’s dual effect on appetite and metabolism offers a promising avenue for sustainable weight management when combined with behavioral strategies (NEJM article on semaglutide and weight loss).
Listening to Your Body: When to Adjust Dosage or Seek Medical Advice
Throughout my weight loss journey, I learned that communication with my healthcare provider was invaluable. If side effects like nausea or dizziness became persistent, it was a sign to pause and reassess the dosage rather than push through blindly. Adjusting dose increments or timing injections differently can make a big difference in tolerability. I recommend anyone on semaglutide to keep a symptom diary and openly discuss any concerns with their doctor to ensure the safest, most effective path forward. For detailed advice, you might want to explore safe dosage guidelines for semaglutide.
How Semaglutide Fits into Broader Medical Weight Loss Programs
Semaglutide is increasingly becoming a cornerstone in medically supervised weight loss programs that combine pharmacotherapy with nutrition counseling and lifestyle coaching. Programs like these offer a structured environment that can enhance accountability and provide holistic support. I found that enrolling in a program helped me stay motivated and gave me access to experts who tailored the approach to my unique needs. If you’re curious about how these programs work in practice, check out this comprehensive guide on medical weight loss programs featuring semaglutide.
Encouraging You to Share and Learn From Others
Weight loss journeys are deeply personal yet incredibly communal in their challenges and triumphs. Have you tried semaglutide or considered it? What hurdles or surprises have you encountered? I invite you to share your experiences or questions in the comments below. Your story could be the motivation someone else needs. Plus, if you found these insights helpful, please share this article with friends or family exploring effective and safe weight loss options.
Unraveling Semaglutide’s Long-Term Weight Loss Sustainability: Beyond Initial Success
While semaglutide injections often produce rapid and impressive weight loss within the initial months, the question of maintaining these benefits over the long haul remains an active area of clinical inquiry. The underlying biology suggests that semaglutide’s appetite-suppressing effects might wane if treatment is discontinued, potentially leading to weight regain. Research underscores the importance of continuous therapy combined with lifestyle modifications to sustain fat loss and metabolic improvements.
Recent trials have demonstrated that patients who adhere to semaglutide for 68 weeks or longer experience more durable outcomes, often accompanied by favorable changes in cardiometabolic risk factors. However, this also necessitates vigilance regarding medication tolerance, psychological adaptation, and metabolic set points that may resist prolonged weight reduction. Understanding these dynamics is crucial for clinicians tailoring long-term treatment plans.
How does semaglutide influence neuroendocrine pathways involved in weight regulation over extended periods?
Semaglutide acts centrally through the hypothalamus and brainstem to modulate hunger and satiety signals, engaging pathways involving pro-opiomelanocortin (POMC) neurons and inhibiting neuropeptide Y/agouti-related peptide (NPY/AgRP) neurons. Over time, the brain’s adaptive responses may alter receptor sensitivity or downstream signaling, potentially attenuating the drug’s efficacy. Studies published in Obesity Reviews suggest that combining semaglutide with behavioral interventions may counteract such adaptations, maintaining weight loss momentum (Obesity Reviews on semaglutide and neuroendocrine adaptations).
Psychological Dimensions: Navigating Emotional and Behavioral Shifts During Treatment
Beyond physiological effects, semaglutide use intersects deeply with psychological processes. Rapid weight loss can trigger shifts in body image perception, self-esteem, and eating behaviors. Patients may experience reduced food cravings but also confront emotional voids previously filled by eating. Addressing these nuanced challenges often requires integrated support from mental health professionals skilled in eating behavior and body image counseling.
Moreover, some patients report changes in reward processing related to food, which can alter motivation and compliance. Awareness of such psychological shifts allows for proactive strategies, including cognitive-behavioral therapy and mindfulness practices, to reinforce healthy habits and emotional resilience throughout the weight loss journey.
Clinical Pearls: Tailoring Semaglutide for Complex Patient Profiles
While semaglutide presents a powerful tool, its administration must be finely tuned to individual patient profiles, particularly in populations with comorbidities such as type 2 diabetes, cardiovascular disease, or psychiatric disorders. For instance, dosing adjustments might be required to mitigate gastrointestinal side effects in sensitive individuals, or additional monitoring may be warranted to prevent hypoglycemia when combined with other antidiabetic agents.
Attention to drug-drug interactions is vital, especially in polypharmacy settings common among the obese population. Clinicians should also be mindful of contraindications and ensure comprehensive patient education regarding injection techniques, side effect management, and expectations. The evolving clinical guidelines, such as those from the European Society of Cardiology, provide detailed frameworks for integrating semaglutide into multifaceted treatment regimens.
Exploring Future Horizons: Innovations and Research Directions in Semaglutide Therapy
The landscape of GLP-1 receptor agonists continues to evolve, with emerging formulations and combination therapies aiming to enhance efficacy and patient convenience. Research is underway exploring oral semaglutide formulations, which could dramatically improve accessibility and adherence. Additionally, combination therapies pairing semaglutide with agents targeting complementary metabolic pathways hold promise for synergistic benefits.
Ongoing studies also investigate semaglutide’s potential roles beyond weight loss, including effects on nonalcoholic fatty liver disease (NAFLD) and neurodegenerative disorders, reflecting its systemic impact on metabolic and inflammatory pathways.
Engage with Expert Insights and Stay Informed
Understanding the multifaceted nature of semaglutide therapy is key to harnessing its full potential in weight management. We invite you to explore further expert analyses and share your experiences or questions to foster a community of informed, empowered individuals. For a deeper dive into clinical best practices and emerging data, visit our comprehensive resources and join the conversation.
Neuroadaptive Mechanisms: Sustaining Semaglutide’s Efficacy Beyond Initial Weight Loss
Long-term administration of semaglutide unveils a complex interplay within neuroendocrine circuits that govern energy homeostasis. The drug’s sustained engagement with hypothalamic pathways modulates both anorexigenic and orexigenic neurons, particularly through prolonged activation of pro-opiomelanocortin (POMC) neurons and inhibition of neuropeptide Y/agouti-related peptide (NPY/AgRP) neurons. However, adaptive neuroplasticity may attenuate receptor responsiveness, necessitating adjunctive behavioral interventions to preserve weight loss momentum and prevent metabolic compensation.
Psychobehavioral Dimensions: Integrating Mental Health Strategies with Pharmacotherapy
Semaglutide’s impact transcends physiological appetite suppression, intersecting with psychological domains that influence eating behaviors and emotional well-being. The rapid alteration in body composition often triggers shifts in self-perception and reward processing, sometimes eliciting challenges such as emotional eating or identity renegotiation. Incorporating cognitive-behavioral therapy, mindfulness-based interventions, and supportive counseling can enhance treatment adherence, mitigate relapse risk, and foster sustainable lifestyle modifications.
What are the best clinical practices to optimize semaglutide use in patients with complex comorbidities?
Optimal semaglutide therapy in patients with multifaceted health profiles requires a nuanced approach. Clinicians should individualize dosing strategies to accommodate coexisting conditions such as type 2 diabetes, cardiovascular disease, and psychiatric disorders, carefully monitoring for adverse effects and potential drug interactions. Multidisciplinary collaboration is paramount, integrating endocrinologists, cardiologists, psychiatrists, and dietitians to tailor comprehensive care plans. The European Society of Cardiology’s latest guidelines provide an authoritative framework for such integrative management (ESC Clinical Practice Guidelines).
Emerging Innovations: The Future of Semaglutide-Based Therapeutics and Beyond
Cutting-edge research is expanding semaglutide’s therapeutic horizon, exploring novel delivery systems such as oral formulations that promise enhanced patient adherence and convenience. Combination therapies targeting synergistic metabolic pathways are under investigation to potentiate efficacy and address residual obesity-related complications. Furthermore, semaglutide’s pleiotropic effects on hepatic steatosis and neuroinflammation suggest promising roles in treating nonalcoholic fatty liver disease (NAFLD) and neurodegenerative disorders, heralding a new era in metabolic medicine.
Engage with Advanced Perspectives and Elevate Your Weight Management Strategy
Harnessing the full potential of semaglutide requires a sophisticated understanding of its multifactorial effects and integration into personalized treatment paradigms. We encourage healthcare professionals and patients alike to delve deeper into emerging evidence, share clinical experiences, and participate in expert dialogues. Connect with our community to access comprehensive analyses, latest research updates, and practical guidance for optimizing semaglutide therapy.
Frequently Asked Questions (FAQ)
What is semaglutide and how does it promote weight loss?
Semaglutide is a glucagon-like peptide-1 (GLP-1) receptor agonist that mimics the natural hormone GLP-1. It acts on the brain’s appetite centers to reduce hunger and increase feelings of fullness, slows gastric emptying to prolong satiety, and improves insulin secretion and glucose regulation. Together, these mechanisms decrease caloric intake and enhance metabolic health, facilitating significant and sustained weight loss.
Is semaglutide safe for rapid weight loss, and what are common side effects?
Semaglutide has been approved by regulatory authorities such as the FDA for obesity treatment after rigorous clinical trials confirming its safety profile. Common side effects include mild gastrointestinal symptoms like nausea, vomiting, or diarrhea, which typically diminish over time with dose titration. Weekly dosing under medical supervision helps monitor side effects and adjust therapy for individual tolerance, ensuring safe and effective weight loss.
How should semaglutide injections be administered for optimal results?
Semaglutide is administered via subcutaneous injection once weekly. Initiation starts with a low dose that is gradually increased under medical guidance to minimize side effects. Proper injection techniques, timing, and storage are essential to maintain drug efficacy. Regular follow-ups allow personalized dose adjustments and integration with lifestyle interventions to maximize outcomes.
Can semaglutide be combined with lifestyle changes like diet and exercise?
Yes, semaglutide’s effectiveness is enhanced when combined with balanced nutrition and regular physical activity. It complements appetite control and metabolic improvements by supporting behavioral changes. Strategies such as intermittent fasting paired with semaglutide have shown promising results in accelerating fat loss safely.
What psychological effects might occur during semaglutide treatment?
Rapid weight loss with semaglutide can prompt emotional and behavioral shifts, including changes in body image, self-esteem, and reward responses to food. Patients may experience reduced cravings but also need to address emotional eating or identity adjustments. Integrating mental health support like cognitive-behavioral therapy can enhance adherence and long-term success.
How long should semaglutide treatment continue for sustainable weight loss?
Long-term adherence to semaglutide, often 68 weeks or more, is associated with durable weight loss and metabolic benefits. Discontinuation may lead to weight regain as appetite suppression wanes. Continuous treatment combined with lifestyle modifications is recommended for maintaining results, under ongoing medical supervision.
Are there special considerations for patients with comorbidities?
Patients with conditions such as type 2 diabetes, cardiovascular disease, or psychiatric disorders require individualized dosing and close monitoring due to potential drug interactions and side effects. A multidisciplinary healthcare team approach ensures safe integration of semaglutide into complex treatment regimens.
What future developments are expected in semaglutide therapy?
Research is advancing toward oral semaglutide formulations for improved convenience and adherence, as well as combination therapies targeting complementary metabolic pathways. Additionally, semaglutide is being explored for benefits in conditions like nonalcoholic fatty liver disease and neurodegenerative disorders, expanding its therapeutic potential.
How does semaglutide affect neuroendocrine mechanisms over time?
Semaglutide modulates hypothalamic neurons involved in hunger and satiety, notably activating anorexigenic POMC neurons and inhibiting orexigenic NPY/AgRP neurons. Over prolonged use, neuroadaptive changes may reduce receptor sensitivity, which can attenuate efficacy. Behavioral interventions alongside pharmacotherapy help sustain weight loss momentum.
When should patients seek medical advice during semaglutide treatment?
Patients should consult their healthcare provider promptly if side effects like persistent nausea, dizziness, or hypoglycemia occur. Keeping a symptom diary and maintaining open communication enable timely dose adjustments and ensure safety throughout the treatment course.
Trusted External Sources
- U.S. Food and Drug Administration (FDA) – Provides official drug approval information and safety data for semaglutide, ensuring regulatory compliance and clinical guidance (FDA official site).
- The New England Journal of Medicine (NEJM) – Publishes high-impact peer-reviewed research articles on semaglutide’s mechanisms and clinical trials, offering in-depth scientific insights (NEJM article on semaglutide and weight loss).
- European Society of Cardiology (ESC) Clinical Practice Guidelines – Offers expert recommendations on integrating semaglutide into treatment plans for patients with cardiovascular and metabolic comorbidities (ESC Guidelines).
- Obesity Reviews (Wiley Online Library) – Provides comprehensive reviews on semaglutide’s neuroendocrine effects and strategies to overcome adaptive resistance (Obesity Reviews on semaglutide and neuroendocrine adaptations).
- Best Fast Weight Loss Diets – A specialized resource offering practical guidance on semaglutide administration, lifestyle integration, and patient experiences, enriching clinical perspectives (BestFastWeightLossDiets.com).
Conclusion
Semaglutide injections represent a scientifically grounded and clinically validated approach to achieving rapid, safe, and sustainable weight loss. By targeting key neuroendocrine pathways that regulate hunger and metabolism, semaglutide not only facilitates fat loss but also improves metabolic health markers. Optimal outcomes arise from combining pharmacotherapy with lifestyle modifications and psychological support, tailored to individual needs and comorbidities. Emerging innovations promise even greater accessibility and expanded therapeutic roles. Embracing a multidisciplinary, informed approach empowers patients and clinicians to navigate the complexities of obesity management effectively. We encourage you to explore further expert content, engage with ongoing research, and share your experiences to contribute to a community committed to transformative weight loss solutions.
If you found this article valuable, please share it with others on their weight loss journey or leave your questions and insights in the comments below. Together, we can advance understanding and foster healthier lives.

The science behind semaglutide’s ability to promote weight loss is truly fascinating, especially its dual action on appetite suppression and metabolic regulation. I’ve read that by mimicking the GLP-1 hormone, it not only helps reduce hunger but also improves insulin sensitivity, which is crucial for metabolic health. What stands out to me is how semaglutide slows gastric emptying, prolonging the feeling of fullness — a factor many traditional diets overlook. However, I’m curious about the emotional and psychological shifts mentioned in the article. Rapid weight loss can sometimes lead to unexpected emotional challenges, like reframing one’s relationship with food or adjusting to new body image perceptions. Has anyone else experienced these aspects while on semaglutide? Additionally, integrating semaglutide with lifestyle changes such as intermittent fasting or mindful eating seems to enhance results. I wonder how patients effectively maintain motivation and balance treatment side effects during this process. For those who have navigated this journey, what strategies helped you align the physiological benefits with mental and emotional well-being? It would be great to hear diverse perspectives, especially from those managing comorbid conditions alongside semaglutide therapy.