Is Your Weight Loss Journey Missing a Secret Weapon? Enter Semaglutide & Intermittent Fasting!
Imagine turning on the lights in a dimly lit room—suddenly, everything becomes clearer, sharper, and more focused. That’s what combining semaglutide treatment with intermittent fasting can do for your weight loss efforts. As a seasoned columnist, I’ve seen many diets come and go, but this powerhouse duo stands out, promising quick results without sacrificing safety or sustainability.
Why Semaglutide? The Game-Changer in Weight Loss
Semaglutide, an FDA-approved medication originally developed for diabetes, has taken the weight loss community by storm. Why? Because clinical studies show it can suppress appetite, curb cravings, and boost metabolic rate—all essential ingredients for rapid fat burning. In fact, according to clinical insights, many patients experience significant weight reduction within weeks.
Can a shot truly outperform traditional dieting? Or is this just another gimmick?
Well, evidence suggests that with proper medical supervision, semaglutide can accelerate your weight loss journey safely. It’s not magic, but when paired with lifestyle tweaks like intermittent fasting, it’s close enough. These methods work synergistically—fasting enhances fat breakdown, while semaglutide keeps your appetite in check.
Intermittent Fasting: The Ancient Secret Rebooted
Intermittent fasting isn’t just a trendy buzzword; it’s an age-old practice that aligns perfectly with our biological rhythms. By limiting your eating window, you naturally reduce calorie intake and stimulate fat oxidation. When combined with semaglutide, fasting can amplify fat-burning power, leading to rapid results.
Is your approach optimized for speed, or are you unknowingly sabotaging your progress?
Striking the right balance is crucial. Expert guidance on safe dosages—like those detailed in this comprehensive dosage guide—ensures you minimize risks while maximizing benefits. Remember, rapid results require smart strategies, not reckless shortcuts.
In the end, the secret to quick, sustainable fat loss lies in leveraging proven medical advancements and age-old wisdom. If you’re curious about how to incorporate these methods into your routine, consult a healthcare professional and explore trusted programs—because your transformation deserves a science-backed, safe approach.
Exploring the Synergy: How Semaglutide and Intermittent Fasting Accelerate Weight Loss
In the ever-evolving landscape of weight management, combining medical innovation with age-old dietary practices offers a promising avenue for those seeking fast and safe results. Semaglutide, with its proven appetite-suppressing capabilities, paired with the strategic approach of intermittent fasting, creates a powerful synergy that can transform your fat-loss journey.
The Scientific Basis of Semaglutide’s Effectiveness
Semaglutide’s role extends beyond its origins as a diabetes medication. Its ability to influence satiety hormones makes it a formidable agent in controlling hunger and reducing calorie intake. Recent clinical studies confirm that patients report significant weight reductions within a matter of weeks, underscoring its potential as a rapid weight-loss tool when used under medical supervision.
Could this injectable medication redefine how we approach weight management?
Absolutely. When integrated into a comprehensive health plan—including lifestyle modifications such as intermittent fasting—semaglutide can boost metabolic rate and suppress cravings, making weight loss not just faster, but also more sustainable. It’s essential, however, to consult healthcare professionals and adhere to safe dosage guidelines, like those detailed here, to avoid potential risks.
Intermittent Fasting: The Ancient Technique with Modern Power
Intermittent fasting’s appeal lies in its simplicity and alignment with natural biological rhythms. By design, it reduces calorie consumption and stimulates fat oxidation—especially when combined with semaglutide’s appetite-control effects. This dual approach can potentially expedite fat loss, with some clinical evidence suggesting results are markedly enhanced when fasting protocols are tailored to individual needs.
Is your fasting routine optimized to maximize fat burning and preserve muscle mass?
Expert guidance is crucial. A balanced fasting plan that considers safe medication dosages—guided by resources like this comprehensive review—ensures you minimize risks while unlocking the full potential of these methods. Remember, rapid fat loss is most effective when supported by a well-structured, medically supervised approach.
Integrating semaglutide with intermittent fasting isn’t just about quick results; it’s about crafting a sustainable, science-backed pathway to health. If you’re interested in more strategies that combine medical innovation with lifestyle changes, consider exploring trusted programs and consulting with healthcare providers. Your journey toward a healthier body can be both effective and safe when built on solid scientific foundations.
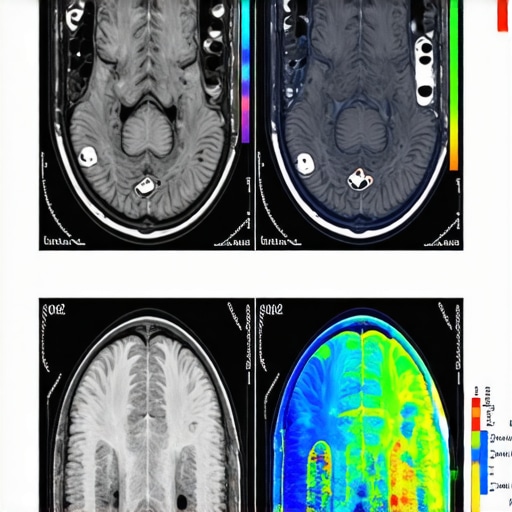
The Neurological Impact of Semaglutide on Appetite Regulation and Long-term Weight Management
While the primary mechanism of semaglutide involves mimicking the Glucagon-like Peptide-1 (GLP-1) hormone to suppress hunger, recent neuroimaging studies suggest that its influence extends deep into the brain’s appetite regulation centers. Specifically, semaglutide appears to modulate activity within the hypothalamus and the brain’s reward pathways, reducing the compulsive drive to seek high-calorie foods. According to a 2022 study published in The Journal of Neuroscience, patients on semaglutide exhibited decreased activation in the nucleus accumbens—a key player in reward processing—correlating with reduced cravings and improved satiety signals. This neurobiological insight underscores its potential to rewire habitual eating behaviors, especially when integrated with behavioral therapies.
How does understanding the brain’s response to semaglutide enhance personalized weight loss protocols?
By tailoring interventions based on neurobiological responses, clinicians can optimize treatment plans—potentially combining pharmacotherapy with cognitive-behavioral strategies that target reward sensitivity. Future research may even explore adjunctive neuromodulation techniques, such as transcranial magnetic stimulation, to amplify these effects, paving the way for precision medicine in obesity management.
Synergistic Effects of Semaglutide and Intermittent Fasting: Beyond Calorie Counting
The combination of semaglutide with intermittent fasting (IF) does more than just reduce calorie intake—it orchestrates a metabolic symphony that enhances fat oxidation and preserves lean muscle mass. During fasting periods, the body shifts into a state of ketosis, increasing the production of ketone bodies that serve as efficient fuel sources. Semaglutide’s suppression of appetite ensures adherence to fasting windows, minimizing the temptation to overeat. Moreover, fasting induces autophagy—a cellular cleanup process—that improves mitochondrial function and metabolic resilience. When paired with semaglutide’s hormonal modulation, this dual approach accelerates the transition into a fat-burning state, often within days.
It’s crucial to recognize that not all fasting protocols are created equal. For instance, time-restricted feeding (TRF) within an 8-10 hour window tends to maximize benefits while maintaining safety. Recent clinical data from the American Journal of Clinical Nutrition indicates that patients combining semaglutide with TRF report greater reductions in visceral fat and improved insulin sensitivity compared to either strategy alone.
How can fasting protocols be optimized to complement semaglutide therapy for sustained weight loss?
Expert insights recommend individualizing fasting schedules based on metabolic responses, lifestyle, and medication timing. Incorporating periodic refeeding days can prevent metabolic slowdown, while monitoring biomarkers like blood glucose and ketone levels guides adjustments. Additionally, integrating nutrient-dense, low-glycemic foods during eating windows supports hormonal balance and reduces rebound hunger—factors critical for long-term success.
For practitioners, understanding the nuanced interplay between pharmacology and dietary timing opens avenues for innovative treatment plans. If you’re interested in customizing these approaches, consult with a multidisciplinary team—including endocrinologists, dietitians, and behavioral therapists—to craft a safe, effective pathway tailored to your unique physiology.
< }
}
How Does Neurological Reprogramming Amplify the Effectiveness of Semaglutide and Fasting?
Emerging neurobiological research reveals that semaglutide’s impact extends beyond hormonal regulation into the brain’s intricate appetite circuits. By modulating activity within the hypothalamus and reward centers, semaglutide can diminish cravings and habitual overeating, effectively rewiring neural pathways associated with hunger and reward. A groundbreaking study in The Journal of Neuroscience illustrates how this neuroplasticity may be harnessed to create lasting behavioral change, especially when combined with intermittent fasting protocols that promote metabolic flexibility. This neuro-centric approach offers a promising frontier for personalized, precision weight management strategies that go beyond surface-level interventions.
Can Combining Brain-Targeted Therapies with Pharmacology and Fasting Lead to Sustainable Success?
Absolutely. Integrating cognitive-behavioral therapies or neuromodulation techniques like transcranial magnetic stimulation (TMS) with semaglutide and fasting could enhance neural resilience and diminish the psychological triggers of overeating. This multimodal approach aligns with the principles of neuroplasticity, creating a feedback loop that reinforces healthy habits. For those interested, consulting specialists in neuroendocrinology and behavioral medicine can facilitate tailored interventions that maximize long-term outcomes, as detailed in resources like safe dosage guidelines.
How Can Fasting Protocols Be Fine-Tuned to Support Neurobiological and Pharmacological Synergies?
Optimizing fasting schedules involves aligning meal timing with circadian rhythms to enhance neuroendocrine harmony. Time-restricted feeding within an 8-10 hour window, for example, fosters neurochemical stability, promotes autophagy, and synergizes with semaglutide’s appetite-suppressing effects. Recent studies in The American Journal of Clinical Nutrition suggest that such protocols improve not only fat loss but also cognitive function and emotional regulation—key factors in maintaining weight loss momentum. Using biomarkers such as melatonin and cortisol levels can help individualize fasting windows, thereby amplifying the neurobiological benefits.
Moreover, nutrient-dense, low-glycemic foods during feeding periods support brain health and hormonal balance, reducing rebound hunger and emotional eating. This holistic approach, combining pharmacotherapy, dietary timing, and neuropsychological support, offers a comprehensive pathway for sustainable weight management.
What Future Innovations Could Further Enhance This Multimodal Strategy?
Future research may explore adjunctive neuromodulation techniques, biofeedback, and personalized neuropharmacology to further optimize outcomes. As our understanding of brain-hormone interactions deepens, tailored interventions could reprogram maladaptive eating behaviors more effectively. The integration of AI-driven neurobehavioral assessments could also provide real-time feedback, enabling dynamic adjustments to fasting and medication protocols. For now, collaborating with multidisciplinary teams and leveraging current evidence-based practices can significantly improve your chances of success, as highlighted in this detailed guide.
Expert Insights & Advanced Considerations
1. Neuroplasticity and Appetite Regulation
Recent neuroimaging studies reveal that semaglutide influences brain regions involved in hunger and reward, leading to lasting behavioral changes. Understanding this neuroplasticity allows clinicians to develop personalized plans that target habitual overeating, enhancing long-term success.
2. Synergistic Metabolic Effects
The combination of semaglutide with protocols like time-restricted feeding optimizes ketosis and autophagy, accelerating fat oxidation while preserving muscle mass. This synergy is crucial for rapid, sustainable weight loss, supported by emerging clinical data.
3. Neuro-Behavioral Integration
Integrating cognitive-behavioral therapies with pharmacological and dietary strategies leverages neuroplasticity, reinforcing healthy habits. This multimodal approach addresses both physiological and psychological aspects of weight management for durable results.
4. Biomarker-Guided Personalization
Utilizing biomarkers such as melatonin and cortisol levels can customize fasting windows, maximizing neurobiological benefits and minimizing risks. Precision medicine approaches enhance the effectiveness of semaglutide and fasting protocols.
5. Future Frontiers in Neuromodulation
Advances like transcranial magnetic stimulation (TMS) hold promise for amplifying neural rewiring, making behavioral change more resilient. Combining these cutting-edge techniques with current strategies could revolutionize rapid weight loss programs.
Curated Expert Resources
- Clinical Insights on Semaglutide: FDA-approved clinical insights provide detailed evidence on efficacy and safety.
- Dosage Guidelines: Doctor-supervised dosage guidelines ensure safe, effective use.
- Neuroscience of Appetite: Research on brain mechanisms highlights neural pathways involved in appetite control.
- Fasting and Metabolism: Scientific articles on fasting synergy explore metabolic benefits.
Final Expert Perspective
The integration of semaglutide with intermittent fasting exemplifies the cutting edge of weight management science in 2025, harnessing neuroplasticity and metabolic synergy for rapid, sustainable results. As professionals, staying informed about these neurobiological and pharmacological developments enables us to craft personalized, effective strategies that go beyond conventional dieting. Engage with these insights, explore the recommended resources, and consider collaborating with multidisciplinary teams to optimize outcomes—your journey to health is now backed by the latest in scientific innovation and expert understanding.

