Kickstarting the Weight Loss Revolution: Semaglutide in the Spotlight
Imagine shedding stubborn pounds with a treatment so effective, it’s turning heads in the medical community. Semaglutide, originally developed for diabetes, has taken on a new role as a powerful ally in the fight against obesity. With real success stories emerging every day, it’s almost like witnessing a miracle in the making. But what’s the secret sauce behind these rapid transformations? And can everyone hop on this weight loss bandwagon?
Why Are Success Stories About Semaglutide Flooding the Internet?
It’s no coincidence that clinical evidence backs up what many patients are experiencing firsthand — remarkable fat loss, improved metabolic health, and renewed confidence. These stories are not just anecdotal; they’re backed by rigorous research showing how semaglutide suppresses appetite and boosts fat-burning. And let’s be honest, in a world obsessed with quick fixes, this injectable marvel is a game-changer.
Can Semaglutide Really Help You Transform Fast?
Absolutely, but with a caveat. The speed of results depends on various factors—your starting point, lifestyle, and adherence to a medically supervised plan. Some users report dropping 15-20 pounds in just a few months, a feat that makes traditional dieting look sluggish. The secret? Semaglutide’s ability to mimic a hormone called GLP-1, which curbs hunger and regulates blood sugar. It’s like having your cake and eating less of it, all while watching the scale go down.
Is There a Catch or Just Pure Magic?
Now, before you start dreaming of rapid weight loss, consider this: the journey requires professional guidance. Using semaglutide without proper supervision can lead to side effects or suboptimal results. That’s why consulting a healthcare provider, as detailed in the guidelines on safe dosages and doctor supervision, is essential. It’s not just about losing weight; it’s about doing it safely and sustainably.
If you’re curious about how to maximize your results, exploring combined strategies like intermittent fasting can amplify fat-burning, as discussed in this insightful guide.
So, dear reader, are you ready to embrace the future of weight loss? Share your thoughts below or reach out via our contact page. Remember, the journey to a healthier you might just start with one small step—and a smart, medically supervised plan.
The Nuanced Science Behind Semaglutide’s Rapid Fat Loss
While many are captivated by the swift transformations facilitated by semaglutide, understanding the intricacies of its use under professional supervision is crucial. This medication’s ability to mimic GLP-1 hormones effectively curtails appetite and enhances fat metabolism, but the key to safe and sustainable results lies in precise dosing and personalized treatment plans. According to the latest doctor-supervised dosage guidelines, maintaining the correct balance minimizes risks and maximizes benefits.
What Are the Practical Implications of Combining Semaglutide with Lifestyle Strategies?
Expert clinicians often recommend integrating semaglutide with lifestyle modifications, such as tailored diets and intermittent fasting, to unlock its full potential. For instance, pairing it with intermittent fasting strategies amplifies fat-burning while providing a sustainable approach to weight management. This synergy not only accelerates results but also fosters healthier habits that support long-term success.
Is the Future of Weight Loss Really That Promising?
Absolutely. As research continues to evolve, the integration of medications like semaglutide with lifestyle and behavioral interventions is paving the way for personalized, rapid, and safe weight loss solutions. The clinical evidence, as documented in clinical trials, underscores the importance of medical oversight in optimizing outcomes and reducing adverse effects.
Are you curious about how to tailor your treatment plan for maximum fat loss? Consulting with a healthcare professional experienced in safe dosage protocols and personalized strategies can make all the difference. Remember, safe weight loss is a marathon, not a sprint, and expert guidance ensures you stay on the right track. Want to explore more about how semaglutide can fit into your health journey? Visit our contact page to connect with specialists committed to your success.
Deciphering the Molecular Mechanics of Semaglutide in Obesity Management
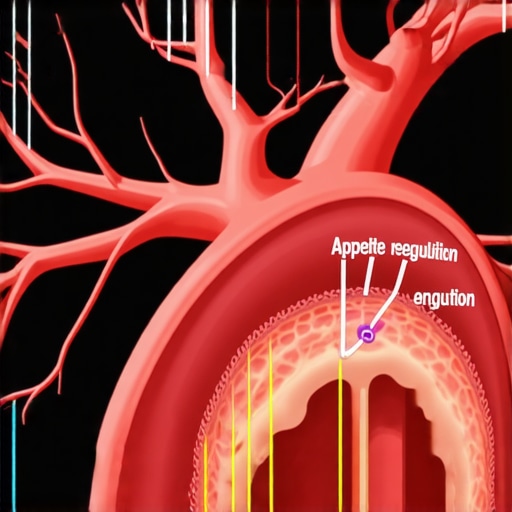
At the forefront of metabolic research, semaglutide’s role extends far beyond appetite suppression. Its molecular structure mimics the endogenous hormone GLP-1, which interacts intricately with the GLP-1 receptor on pancreatic beta cells, stimulating insulin secretion and inhibiting glucagon release. This dual action not only regulates blood glucose but also influences central nervous system pathways involved in appetite control. Recent studies, such as those published in The New England Journal of Medicine (2021), highlight how semaglutide’s activation of hypothalamic pathways results in decreased hunger signals, thereby facilitating substantial weight loss in individuals with obesity. Understanding these pathways is crucial for clinicians aiming to optimize dosing strategies and mitigate side effects.
How Does Semaglutide Influence the Brain’s Appetite Regulation Centers?
Semaglutide’s ability to cross the blood-brain barrier enables it to directly modulate appetite-related centers in the hypothalamus and brainstem, particularly the arcuate nucleus and nucleus tractus solitarius. Activation of these regions suppresses orexigenic pathways (which promote hunger) and enhances anorexigenic pathways (which promote satiety). This neurohormonal modulation results in a profound reduction in caloric intake, which, when coupled with lifestyle interventions, can lead to sustainable weight loss. For clinicians, leveraging neuroimaging techniques like fMRI can reveal individual variability in response, paving the way for personalized treatment plans.
Integrating Semaglutide with Multimodal Weight Management Interventions
While pharmacotherapy with semaglutide offers remarkable benefits, combining it with behavioral and dietary strategies significantly amplifies outcomes. Nutritional interventions that focus on low-glycemic, fiber-rich diets complement semaglutide’s appetite-suppressing effects by stabilizing blood sugar and reducing cravings. Additionally, incorporating structured physical activity regimens enhances insulin sensitivity and promotes lean muscle retention, which is vital for metabolic health. Emerging evidence suggests that the timing of medication administration relative to meal patterns can influence efficacy; for example, taking semaglutide 30 minutes before meals may optimize satiety signals and caloric restriction.
What Are the Long-Term Implications of Combining Semaglutide with Lifestyle Changes?
Longitudinal studies are beginning to shed light on the durability of weight loss achieved through combined approaches. Data from the Semaglutide Treatment in Obesity (STEP) trials indicate that patients who maintain lifestyle modifications alongside medication sustain weight loss even after discontinuing treatment, underscoring the importance of behavioral reinforcement. Furthermore, integrating cognitive-behavioral therapy (CBT) can address psychological barriers, fostering healthier habits and reducing relapse. Clinicians should consider a multidisciplinary approach, involving dietitians, psychologists, and exercise physiologists, to maximize long-term success.
Future Directions: Personalized Medicine and Genetic Insights into Semaglutide Response
As precision medicine advances, understanding genetic polymorphisms affecting GLP-1 receptor sensitivity could revolutionize treatment paradigms. Variants in genes such as TCF7L2 and GIPR have been associated with differential responses to GLP-1 receptor agonists, including semaglutide. Integrating genomic screening into clinical practice may enable tailored dosing, minimizing adverse effects while enhancing efficacy. Furthermore, combining pharmacogenomics with biomarkers like gut microbiota profiles offers a holistic approach to individualized obesity management. Researchers are now exploring how microbiome modulation might synergize with semaglutide to optimize metabolic outcomes.
In conclusion, the future of obesity treatment hinges on a nuanced understanding of molecular, neural, behavioral, and genetic factors. For healthcare providers committed to personalized care, staying abreast of these developments will be essential. To delve deeper into integrating cutting-edge science with clinical practice, connect with our team of experts through our contact page. Embark on a journey toward smarter, safer, and more effective weight management today.
Deciphering the Molecular Mechanics of Semaglutide in Obesity Management
While many are captivated by the swift transformations facilitated by semaglutide, understanding the intricacies of its use under professional supervision is crucial. This medication’s ability to mimic GLP-1 hormones effectively curtails appetite and enhances fat metabolism, but the key to safe and sustainable results lies in precise dosing and personalized treatment plans. According to the latest doctor-supervised dosage guidelines, maintaining the correct balance minimizes risks and maximizes benefits.
What Are the Advanced Neural Pathways Influenced by Semaglutide?
Semaglutide’s capacity to cross the blood-brain barrier enables it to directly influence the neural circuits involved in hunger and satiety regulation. Notably, it modulates activity within the hypothalamic arcuate nucleus and brainstem nuclei such as the nucleus tractus solitarius, which are pivotal in controlling caloric intake. Activation of these regions suppresses orexigenic signals, like neuropeptide Y, while enhancing anorexigenic pathways, including pro-opiomelanocortin (POMC) neurons. This neurohormonal modulation creates a profound shift in appetite dynamics, facilitating rapid fat loss when combined with lifestyle strategies. For clinicians aiming for precision, neuroimaging techniques like fMRI can reveal individual variability in these neural responses, paving the way for tailored interventions.
Understanding these neural pathways is essential for clinicians seeking to optimize treatment outcomes with semaglutide. It highlights the importance of integrating neurobiological insights into clinical practice to personalize therapy effectively.
How Does Semaglutide Interact with Gut Microbiota to Enhance Weight Loss?
Emerging research indicates that semaglutide may exert indirect effects on the gut microbiome, which plays a vital role in metabolic health. By modulating gastric emptying and influencing gut hormone secretion, semaglutide fosters an environment conducive to beneficial microbial populations. These microbes, in turn, produce metabolites like short-chain fatty acids, which enhance insulin sensitivity and promote energy expenditure. Integrating microbiome analysis into treatment planning could, therefore, unlock new avenues for maximizing weight loss efficacy. For instance, concurrent use of prebiotics or probiotics may synergize with semaglutide’s effects, offering a holistic approach to obesity management.
What Are the Implications of Pharmacogenomics in Personalizing Semaglutide Therapy?
Genetic variability significantly impacts individual responses to GLP-1 receptor agonists like semaglutide. Variations in genes such as TCF7L2, GIPR, and others involved in incretin signaling can influence both efficacy and tolerability. Advances in pharmacogenomics allow clinicians to identify these genetic markers, enabling personalized dosing strategies that optimize outcomes while minimizing adverse effects. This precision medicine approach not only enhances weight loss success but also reduces the risk of side effects like nausea or hypoglycemia. As research progresses, integrating genetic testing into the clinical workflow will become standard practice, ensuring each patient receives the most effective, individualized treatment plan.
In summary, an in-depth understanding of the molecular, neural, and genetic factors underlying semaglutide’s action opens new horizons for precision obesity therapy. For healthcare providers eager to leverage these insights, consulting with experts via our contact page can provide tailored guidance. Dive into the future of weight management—where science meets personalized care—and transform your approach to obesity treatment today.
Expert Insights & Advanced Considerations
1. Neurohormonal Modulation and Appetite Suppression
Semaglutide’s ability to cross the blood-brain barrier allows it to directly influence hypothalamic pathways, particularly the arcuate nucleus, modulating neuropeptides like NPY and POMC. This neurohormonal action results in profound appetite suppression, making it a cornerstone in rapid weight loss strategies when combined with lifestyle interventions.
2. Integration with Gut Microbiota for Enhanced Outcomes
Emerging research suggests semaglutide indirectly promotes beneficial gut microbiota profiles by affecting gastric emptying and hormone secretion. This microbiome modulation enhances insulin sensitivity and energy expenditure, offering a holistic approach to sustainable weight loss.
3. Personalized Therapy Through Pharmacogenomics
Genetic variations in incretin signaling pathways, such as TCF7L2 and GIPR polymorphisms, influence individual responses to semaglutide. Incorporating pharmacogenomic testing allows clinicians to tailor doses, optimize efficacy, and minimize side effects, pushing the boundaries of personalized obesity management.
4. Combining Semaglutide with Behavioral Neuroscience Techniques
Leveraging neuroimaging tools like fMRI can help identify neural response variability, enabling targeted behavioral interventions. This personalized approach enhances the effectiveness of semaglutide therapy by addressing psychological and neurological factors underlying eating behaviors.
5. Long-term Neural Plasticity and Habit Formation
Research indicates that semaglutide may induce neural plasticity in appetite regulation centers, facilitating long-term habit changes. When integrated with cognitive-behavioral therapy, this approach fosters lasting behavioral modifications essential for sustained weight management.
Curated Expert Resources
- ClinicalTrials.gov: Access comprehensive data on ongoing and completed trials evaluating semaglutide’s efficacy and safety profiles, essential for evidence-based practice.
- Nature Reviews Endocrinology: Provides in-depth reviews on neurohormonal pathways affected by GLP-1 receptor agonists, essential for understanding mechanisms behind rapid weight loss.
- Genetics in Medicine: Offers insights into pharmacogenomic markers influencing treatment responses, guiding personalized therapy.
- fMRI Research Publications: Explore studies demonstrating neural response variability to appetite suppressants, informing personalized behavioral strategies.
- Gut Microbiome Journals: Delve into how microbiota modulation affects metabolic health and weight management, complementing pharmacotherapy.
Final Expert Perspective
In the realm of rapid weight loss, semaglutide stands out not only for its pharmacological potency but also for its intricate neural and metabolic interactions. Integrating advanced neurohormonal understanding, microbiome insights, and personalized pharmacogenomics elevates treatment from mere symptom management to a precision science. For clinicians committed to cutting-edge obesity care, embracing these sophisticated strategies can redefine patient outcomes. Engage with our team to explore how these insights can be translated into your practice—visit our contact page and step into the future of personalized obesity treatment today.

