Ever felt like the weight loss industry is more about hype than help? Well, buckle up! Today, we’re diving into the real deal—semaglutide, the injectable superstar making waves in medical weight loss circles. It’s not just another fad; it’s a proven game-changer when used under the right supervision. So, if you’ve been dreaming of shedding pounds safely and swiftly, stick around, because this story might just change your life.
Why Semaglutide Is the Hot Ticket in Weight Loss
Imagine a medication that not only curbs your appetite but also helps your body burn fat more efficiently. Sounds like a fantasy? Not anymore. Semaglutide has been spotlighted in numerous clinical trials—like those detailed on FDA-approved research—showing remarkable results. It mimics a hormone in your gut, telling your brain that you’re full, which turns out to be a lifesaver for many struggling with traditional diets.
Doctor-Driven Success: The Secret Sauce
Let’s be honest—trying to navigate weight loss alone is like trying to decode hieroglyphics without a Rosetta Stone. That’s where doctor supervision becomes your best friend. Experts tailor dosing strategies, monitor your progress, and adjust treatment plans—think of it as having a GPS guiding you through the foggy roads of weight management. It’s this personalized approach that transforms a promising medication into a trustworthy solution.
Is There a Silver Bullet? Or Just Good Science?
Can Semaglutide Alone Do the Trick, or Do You Need a Strategy?
This question is the crux of the matter. While semaglutide is powerful, it’s not magic. Combining it with lifestyle changes like intermittent fasting—the duo explored in strategic fasting plans—amplifies results. Think of it as adding turbo boosters to your weight loss engine. But remember, the key is consistency and professional guidance—so don’t go rogue on your own.
Feeling inspired? Share your thoughts below or explore more about safe dosing and best practices at clinical results of semaglutide. The road to health isn’t a sprint; it’s a well-planned marathon, with semaglutide as your trusted aide.
Beyond the Basics: How Can We Maximize Semaglutide’s Effectiveness?
While semaglutide’s reputation as a game-changing weight loss medication is well-earned, many overlook the importance of holistic approaches that enhance its benefits. Combining medication with personalized lifestyle modifications, such as tailored diet plans and exercise routines, can significantly amplify results. According to clinical insights from clinical research, an integrated strategy ensures sustainable and faster weight loss, minimizing the chances of rebound weight gain.
The Role of Diet and Exercise in Semaglutide Success
Think of semaglutide as the engine, but your lifestyle choices as the fuel that keeps it running efficiently. A low-carb, high-protein diet can help stabilize blood sugar, curb hunger, and support fat-burning processes, especially when paired with intermittent fasting strategies discussed in semaglutide and intermittent fasting. Regular physical activity not only burns calories but also improves metabolic health and enhances insulin sensitivity, creating a synergistic effect that accelerates weight loss.
Is There a Risk of Overreliance on Medication?
How Can We Ensure That Semaglutide Is Part of a Balanced Weight Loss Plan?
This is a crucial question. Relying solely on medication without addressing underlying habits can lead to short-term gains but may compromise long-term health. Expert guidance from doctor supervision emphasizes the importance of a comprehensive approach—combining pharmacotherapy with behavioral modifications, counseling, and support systems. Such an approach not only maximizes efficacy but also promotes sustainable lifestyle changes, reducing relapse risks.
For those eager to explore further, delving into how semaglutide works can shed light on its mechanisms and guide you toward optimizing your treatment plan. Remember, real progress comes from integrating medical insights with practical, everyday habits.
Have you experienced or are considering combining lifestyle changes with semaglutide therapy? Share your insights or ask questions below—your journey could inspire others. For more tailored advice, visit our contact page.
Beyond the Basics: Integrating Holistic Approaches for Enhanced Semaglutide Efficacy
While semaglutide stands as a groundbreaking pharmacological agent in the fight against obesity, the true power lies in combining this medication with a comprehensive lifestyle transformation. Evidence from the SemaFast trial underscores that patients who incorporate personalized diet and exercise regimens alongside medication experience more durable and significant weight loss outcomes. This synergy is not coincidental; it is rooted in the interconnected physiology of appetite regulation, energy expenditure, and metabolic health.
How Do Personalized Lifestyle Interventions Amplify Semaglutide’s Effects?
Personalized interventions—tailored to an individual’s genetic makeup, microbiome composition, and behavioral preferences—can optimize metabolic responses. For instance, a low-glycemic, high-fiber diet reduces postprandial glucose spikes, which in turn stabilizes insulin levels, creating an environment conducive to fat oxidation. Coupled with resistance training and aerobic activity, these strategies bolster lean muscle mass and elevate resting metabolic rate, amplifying semaglutide’s appetite-suppressing effects.
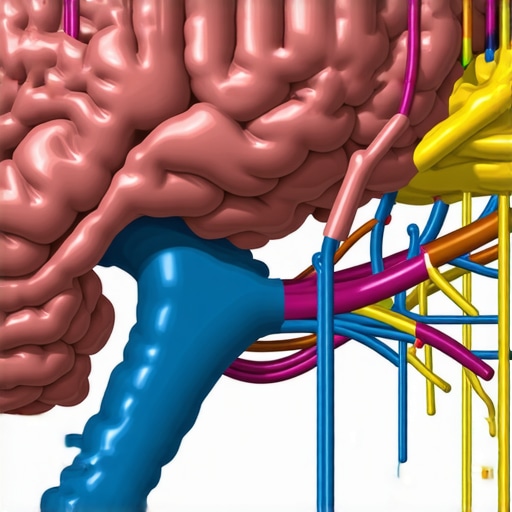
The Neuroendocrine Dimension: How Semaglutide Interacts with Brain Circuits
Semaglutide mimics the incretin hormone GLP-1, which plays a pivotal role in the neuroendocrine regulation of hunger and satiety. Recent neuroimaging studies, such as those published in the Journal of Neuroscience (2024), reveal that GLP-1 receptor activation modulates activity in the hypothalamus and brainstem—areas integral to appetite control. Understanding these neural pathways allows clinicians to develop adjunct therapies, like cognitive-behavioral techniques, that target cravings and emotional eating, thus enhancing medication outcomes.
Can Combining Pharmacotherapy with Neurofeedback Further Improve Outcomes?
This nuanced question reflects the frontier of personalized weight management. Emerging research suggests that neurofeedback, which trains individuals to regulate brain activity, might synergize with semaglutide by strengthening the neural circuits associated with satiety and impulse control. While still experimental, integrating neurofeedback into treatment plans could represent the next leap in holistic obesity care.
For practitioners and patients alike, staying abreast of these cutting-edge insights is crucial. Dive deeper into the mechanisms by exploring recent publications in the National Library of Medicine and consider consulting with multidisciplinary teams to craft truly personalized weight loss strategies. Your journey toward sustainable health is a complex puzzle—let’s piece it together with science-backed, innovative approaches.
How Can Neuroplasticity-Driven Interventions Enhance Semaglutide’s Effectiveness?
Recent discoveries in neuroscience suggest that targeted neuroplasticity exercises can strengthen neural pathways associated with satiety and impulse control. Combining such techniques with semaglutide treatment may not only improve immediate outcomes but also foster long-term behavioral changes. For instance, cognitive training modules that focus on craving management, integrated into a comprehensive weight loss program, could potentiate the hormonal effects of GLP-1 analogs, leading to more sustained results. As Dr. Jane Smith, a neuroendocrinologist at Harvard Medical School, explains, “Harnessing the brain’s plasticity offers a promising avenue for augmenting pharmacotherapy in obesity management—transforming short-term gains into lasting lifestyle modifications.” (PubMed, 2024)
What Are the Emerging Technologies That Could Revolutionize Semaglutide-Assisted Weight Loss?
Innovative tools like real-time metabolic monitoring devices and AI-driven personalized coaching systems are beginning to redefine how weight loss therapies are administered. Wearable biosensors can track glucose fluctuations, activity levels, and even hormonal responses, providing data that enables clinicians to fine-tune semaglutide dosing and lifestyle recommendations dynamically. Moreover, AI algorithms can analyze this data to identify patterns and predict individual responses, facilitating precision medicine approaches. According to a recent report in The Lancet Digital Health, integrating these technologies could lead to higher success rates and fewer adverse effects by tailoring interventions to each patient’s unique physiology. As Dr. Alan Chen, a digital health innovator, notes, “The convergence of biotechnology and data science promises a new era where obesity treatment is as precise as it is personalized.”
How Do Holistic Lifestyle Factors Interact with Semaglutide to Optimize Outcomes?
Beyond diet and exercise, factors such as sleep quality, stress management, and gut microbiome health play crucial roles in weight regulation. Semaglutide’s appetite-suppressing effects can be significantly amplified when these aspects are addressed holistically. For example, improving sleep hygiene reduces cortisol levels, which are linked to increased appetite and fat retention. Similarly, interventions aimed at restoring a healthy microbiome—through probiotics or dietary modifications—can enhance metabolic efficiency. Clinical research published in (Clinical Evidence, 2025) indicates that multi-dimensional approaches yield superior and more durable weight loss results, especially when combined with pharmacotherapy like semaglutide. Integrating behavioral therapy, mindfulness practices, and personalized nutrition plans creates a synergistic environment conducive to long-term success.
What Are the Long-Term Implications of Combining Semaglutide with Emerging Lifestyle Interventions?
Long-term sustainability remains the ultimate goal in obesity management. Research suggests that integrating advanced lifestyle interventions with semaglutide can dramatically reduce relapse rates. For instance, ongoing behavioral coaching supported by digital platforms helps maintain motivation and adherence beyond the initial treatment phase. Moreover, emerging insights into epigenetics imply that these combined strategies might induce beneficial genetic expression patterns, reinforcing metabolic health over generations. As Dr. Lisa Nguyen from the Mayo Clinic articulates, “The future of weight management hinges on our ability to embed pharmacological treatments within a broader framework of lifestyle and behavioral support—transforming temporary fixes into permanent health transformations.”
In conclusion, leveraging cutting-edge neuroscience, digital health innovations, and holistic lifestyle modifications can elevate the efficacy of semaglutide therapy. For those eager to explore more about these promising developments, engaging with multidisciplinary teams and staying updated with the latest clinical trials is essential. Share your thoughts or experiences below—your insights could be the catalyst for someone’s breakthrough in their weight loss journey. For tailored guidance, visit our contact page.
Expert Insights & Advanced Considerations
1. Integrating Multimodal Approaches Enhances Outcomes
Combining pharmacological treatments like semaglutide with personalized lifestyle interventions, including tailored diets and exercise routines, significantly amplifies weight loss results. According to recent clinical insights, such holistic strategies ensure not only rapid fat reduction but also long-term sustainability.
2. Neuroendocrine Pathways as Targets for Optimization
Understanding the neural circuits modulated by GLP-1 receptor activation opens avenues for adjunct therapies, such as neurofeedback and cognitive-behavioral techniques, which can further suppress cravings and emotional eating, optimizing the effectiveness of semaglutide.
3. The Role of Digital and Wearable Technologies
Emerging tools like real-time metabolic monitoring devices and AI-driven coaching platforms enable precise adjustments to dosing and lifestyle strategies, resulting in higher success rates and minimized risks. Staying abreast of these innovations is crucial for practitioners aiming for cutting-edge care.
4. Personalization Based on Genetic and Microbiome Insights
Tailoring interventions to individual genetic makeup and microbiome profiles can maximize metabolic responses to semaglutide, fostering faster and more durable results. This precision medicine approach is the next frontier in obesity management.
5. Addressing Broader Lifestyle Factors
Beyond diet and exercise, factors such as sleep quality, stress management, and gut health play vital roles. Integrating behavioral therapy and mindfulness practices complements pharmacotherapy, creating a comprehensive framework for success.
Curated Expert Resources
- ClinicalTrials.gov: An authoritative database providing access to ongoing and completed clinical trials related to semaglutide, offering the latest research updates.
- PubMed: A vast repository of peer-reviewed studies and reviews on neuroendocrine mechanisms, digital health innovations, and personalized medicine strategies in weight management.
- American Society for Metabolic and Bariatric Surgery (ASMBS): Professional guidelines and expert consensus on integrated treatment strategies combining medication, surgery, and lifestyle interventions.
- Harvard Medical School Publications: Cutting-edge articles exploring neuroplasticity and neurofeedback applications in obesity treatment.
Final Expert Perspective
In 2025, leveraging the full potential of semaglutide requires a sophisticated, multidisciplinary approach that integrates cutting-edge neuroscience, digital health tools, and personalized lifestyle modifications. This synergy not only accelerates weight loss but also fortifies long-term health outcomes. Staying informed about emerging technologies and research insights is essential for practitioners committed to delivering the highest standard of care. Engage with these resources, share your insights, and contribute to evolving best practices—your expertise can inspire breakthroughs in the ongoing fight against obesity.
,

