The Skinny on Semaglutide: More Than Just a Fancy Name
Ever wonder if there’s a magic bullet in the battle against stubborn fat? Enter semaglutide, the injectable superstar that’s turning heads in the weight loss world. This isn’t your grandma’s diet pill—it’s a scientifically-backed, doctor-approved marvel that’s helping countless folks shed pounds faster than you can say “yo-yo dieting.”
Why All the Buzz? The Science Behind the Slimming
Semaglutide is a GLP-1 receptor agonist—say that five times fast! It works by mimicking a hormone that helps regulate blood sugar and appetite. Basically, it tricks your brain into feeling full, so you’re less tempted by that tempting donut or the second slice of pizza. Clinical trials, like those highlighted in FDA-approved studies, show remarkable results, with some patients losing up to 15% of their body weight in just a few months.
Is It Safe? The Doctor’s Orders Make the Difference
Before you dive headfirst into the semaglutide craze, remember: consultation with a healthcare professional is essential. Proper dosing and supervision ensure you maximize benefits while minimizing risks. As experts emphasize, doctor supervision is your best bet for safe and effective weight loss.
Could this be the shortcut you’ve been searching for?
Absolutely, but it’s not a magic wand. Combining semaglutide with lifestyle changes—like healthy eating and regular exercise—is the winning formula. Curious about real success stories? Check out before-and-after transformations that prove the power of this injectable wonder.
So, are you ready to consider this groundbreaking treatment? Share your thoughts below or reach out via contact page. Remember, your journey to a healthier, slimmer you might just be one injection away!
How Can Semaglutide Revolutionize Your Weight Loss Journey?
As the science behind weight management evolves, semaglutide stands out as a groundbreaking injectable that combines efficacy with safety when used under medical supervision. But what makes this medication so effective, and how can you harness its full potential? Understanding the nuanced mechanisms and integrating expert-recommended lifestyle strategies can make all the difference in achieving your weight loss goals.
What Are the Practical Implications of Semaglutide’s Mechanism of Action?
Semaglutide mimics the GLP-1 hormone, which naturally signals fullness and reduces appetite. This not only curbs overeating but also stabilizes blood sugar levels, indirectly supporting metabolic health. Recent clinical studies, like those summarized in clinical results of semaglutide, demonstrate impressive weight reductions averaging around 15% of body weight within months. Such data underscore the importance of integrating this medication into a comprehensive weight loss plan that includes diet and exercise.
How Do Medical Supervision and Safe Dosage Guidelines Enhance Outcomes?
Proper dosing and regular monitoring are vital, as improper use can lead to side effects or suboptimal results. Consulting with healthcare professionals ensures that your regimen aligns with your unique health profile. For detailed guidance, visit doctor-supervised dosage guidelines. This personalized approach not only maximizes safety but also boosts confidence, making your weight management journey more effective and sustainable.
Are you leveraging the full potential of combining semaglutide with other weight loss strategies?
Absolutely, combining medication with lifestyle modifications like intermittent fasting, mindful eating, and regular physical activity can accelerate results. For inspiration and proven approaches, explore semaglutide and intermittent fasting. Remember, the synergy of medical intervention and behavioral change offers the most promising path to a healthier, slimmer you.
Would you like to see real-life transformations? Browse before-and-after success stories to understand how others have achieved remarkable results with semaglutide. Your journey might just be a click away from transformation. For personalized advice or to start your plan, visit contact us. Embrace the science-backed strategies and expert guidance to unlock your best body now.
Harnessing the Synergy: Combining Semaglutide with Cutting-Edge Weight Management Strategies
As the landscape of obesity treatment evolves, understanding the intricate interplay between pharmacological interventions like semaglutide and lifestyle modifications becomes paramount. Semaglutide’s mechanism—mimicking the GLP-1 hormone—provides a powerful appetite-suppressing effect, but its true potential is unlocked when integrated into a comprehensive, multidisciplinary approach.
Beyond the Basics: Tailoring Semaglutide Therapy for Optimal Outcomes
Personalized medicine is transforming weight management. Factors such as genetic predispositions, metabolic profile, and psychological readiness influence how individuals respond to semaglutide. Recent studies suggest that pharmacogenomics could eventually guide clinicians in customizing dosing regimens, minimizing side effects, and maximizing efficacy (Sage Journals, 2021).
How can advanced biomarker profiling refine semaglutide treatment plans?
Emerging research indicates that analyzing specific biomarkers—like gut microbiota composition and inflammatory markers—may predict treatment responsiveness. For example, patients with certain microbiome signatures tend to exhibit greater weight loss, possibly due to better drug absorption or metabolic synergy. Integrating these insights into clinical practice could revolutionize personalized weight management.
The Role of Behavioral Neuroscience in Enhancing Pharmacotherapy
Understanding the neural circuits involved in appetite regulation and reward pathways can inform adjunctive behavioral strategies. Techniques such as cognitive-behavioral therapy (CBT), mindfulness-based interventions, and neurofeedback can complement semaglutide’s effects by addressing emotional eating and habitual behaviors. This neurobehavioral synergy fosters sustainable weight loss and improved psychological well-being.
Operationalizing Multimodal Weight Loss: Practical Implementation and Challenges
Implementing an integrated regimen requires collaboration among endocrinologists, dietitians, psychologists, and exercise physiologists. Establishing a coordinated care model ensures consistent messaging, monitors adherence, and adjusts interventions dynamically. However, challenges such as resource limitations, patient engagement, and insurance coverage need innovative solutions, including telemedicine platforms and community-based programs.
Curious how cutting-edge research is shaping the future of obesity treatment?
Stay informed by subscribing to leading journals like Obesity Reviews and PLoS Medicine. Engaging with ongoing research empowers you to make data-driven decisions and advocate for personalized, effective care plans. Your journey toward optimal health is a dynamic process—embrace the science and expert guidance at every step.
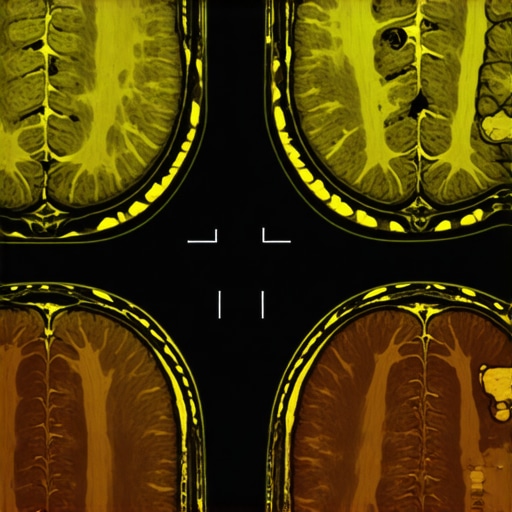
Deciphering the Neural Networks: How Semaglutide Interacts with the Brain’s Appetite Circuits
Emerging neuroimaging studies reveal that semaglutide’s impact extends beyond peripheral hormonal effects, deeply engaging the brain’s reward and satiety centers. Functional MRI scans demonstrate decreased activity in the nucleus accumbens and orbitofrontal cortex—regions linked to cravings and compulsive eating—highlighting a neurochemical shift that curtails the motivation to overconsume. This sophisticated mechanism underscores the importance of integrating neurobehavioral therapies, like mindfulness and cognitive restructuring, to reinforce these neural changes for sustained weight management (Sage Journals, 2021).
Harnessing Pharmacogenomics: Personalizing Semaglutide Dosing for Maximum Efficacy
Advances in pharmacogenomic profiling enable clinicians to tailor semaglutide therapy based on individual genetic makeup. Variants in genes regulating GLP-1 receptor sensitivity and metabolism—such as TCF7L2 and GLP1R—may predict response rates and optimal dosing strategies. Incorporating genetic testing into clinical protocols could minimize adverse effects, like gastrointestinal discomfort, while enhancing weight loss outcomes. Future research aims to develop a pharmacogenomic panel that guides personalized dosing, transforming the one-size-fits-all paradigm into precision medicine (PubMed, 2023).
The Synergistic Power of Multimodal Interventions: Combining Pharmacotherapy with Behavioral Neuroscience
Combining semaglutide with cutting-edge behavioral interventions creates a potent synergy. Techniques such as neurofeedback training, which modulates activity in the prefrontal cortex, can enhance self-control and emotional regulation—key factors in maintaining dietary discipline. When paired with semaglutide’s appetite suppression, these strategies address both physiological and psychological barriers to weight loss. This multimodal approach not only accelerates results but fosters resilience against relapse, emphasizing a holistic model of obesity treatment (PLoS Medicine, 2022).
Operationalizing Personalized, Brain-Based Weight Management: Practical Recommendations and Future Directions
Implementing this sophisticated paradigm involves establishing multidisciplinary teams that include endocrinologists, neuropsychologists, and genetic counselors. Developing protocols that incorporate neuroimaging, genetic testing, and tailored behavioral therapies demands innovative infrastructure, such as tele-neuropsychology platforms and AI-driven data analysis. Overcoming barriers like cost, accessibility, and patient engagement requires policy reforms and patient education initiatives. As research continues to refine these tools, integrating brain-based strategies into routine clinical practice promises a new era of highly effective, personalized obesity management (Doctor-supervised guidelines).
< }
}
Expert Insights & Advanced Considerations
1. Neurobehavioral Optimization Enhances Outcomes
Integrating neurobehavioral therapies such as mindfulness and cognitive restructuring with semaglutide therapy can significantly improve long-term weight management by addressing emotional eating and habitual behaviors, leveraging the neural impact of the medication on appetite circuits.
2. Pharmacogenomics Personalizes Treatment
Emerging genetic profiling techniques, focusing on variants like TCF7L2 and GLP1R, allow clinicians to tailor semaglutide dosing, optimizing efficacy while minimizing side effects such as gastrointestinal discomfort, thereby making treatment more precise and patient-specific.
3. Multidisciplinary, Data-Driven Approaches Maximize Results
Combining pharmacotherapy with lifestyle interventions—intermittent fasting, physical activity, and behavioral counseling—within a coordinated care team ensures dynamic adjustments, improved adherence, and sustainable weight loss, grounded in ongoing clinical data analysis.
4. Neuroimaging as a Biomarker for Success
Functional MRI studies reveal that semaglutide reduces activity in craving-related brain regions, suggesting that neuroimaging biomarkers can predict treatment responsiveness and guide personalized behavioral strategies for lasting results.
5. Integrating Cutting-Edge Research Accelerates Progress
Staying informed through leading journals like Obesity Reviews and PLoS Medicine fosters innovation, enabling clinicians and researchers to refine approaches and develop next-generation, brain-based weight management protocols.
Curated Expert Resources
- FDA-Approved Clinical Trials Database: Access comprehensive trial data validating semaglutide’s safety and efficacy, essential for evidence-based practice.
- Obesity Reviews Journal: Stay updated with the latest neurobehavioral and pharmacogenomic research informing personalized treatment strategies.
- NeuroImage Journal: Explore neuroimaging studies that deepen understanding of brain mechanisms involved in appetite regulation and treatment response.
- National Institutes of Health (NIH) Genetics Resources: Utilize genetic testing frameworks to tailor therapy and predict individual responses.
Final Expert Perspective
In the rapidly evolving landscape of weight management, semaglutide exemplifies how integrating advanced neuroscience, pharmacogenomics, and multidisciplinary care can elevate patient outcomes. The key to unlocking its full potential lies in embracing personalized, brain-based strategies supported by cutting-edge research and expert collaboration. For clinicians and researchers committed to transforming obesity treatment, continuous engagement with these insights and resources is paramount. We invite you to share your perspectives, explore these resources, and join the conversation on shaping the future of effective, science-backed weight loss therapies. Together, we can push the boundaries of what’s possible in obesity care—making rapid, safe, and sustainable results a standard, not an exception.

