Meet Your New Best Friend in Fat Loss: Semaglutide!
If you’ve been wondering whether there’s a miracle pill for rapid weight loss, well, buckle up because 2025 might just be the year of Semaglutide. This injectable wonder has been making waves in medical circles and social media alike — and for good reason. From clinical trials to real-life stories, the evidence is stacking up faster than your favorite jeans after a successful diet.
Why Is Everyone Talking About Semaglutide?
Think of Semaglutide as the Swiss Army knife of weight management. Originally developed for diabetes, it’s now hailed as a top contender for fat burning in the new year. Its secret? It interacts with your brain’s appetite control centers, making you feel full longer and reducing cravings. Imagine saying goodbye to constant snack attacks — yes, it’s as transformative as it sounds.
Is This the End of Dieting as We Know It?
Well, not exactly. But Semaglutide does seem to be rewriting the rules. Clinical studies, such as those summarized in this comprehensive review, suggest that patients are losing weight faster and more sustainably than traditional methods. Could this be the shortcut we’ve all been craving? Possibly. But remember, no magic pill exists without caveats.
To maximize benefits and minimize risks, expert supervision is a must. Check out these dosage guidelines to stay safe while chasing that perfect beach bod.
The Future Looks Bright (and Slim!)
As we step into 2025, the excitement around Semaglutide continues to grow. Its proven ability to accelerate fat burning, especially when combined with strategies like intermittent fasting, makes it a potent tool. For a deeper dive into how it works, this latest review offers a treasure trove of insights.
So, are you ready to embrace the injectable revolution? Or are you skeptical about the hype? Either way, your thoughts are welcome—drop a comment below or explore more about the safety and effectiveness of this remarkable drug. Remember, informed choices lead to better results.
Can Semaglutide Truly Transform Your Weight Loss Journey in 2025?
As we venture further into 2025, the buzz around Semaglutide continues to grow, and for good reason. This injectable medication, originally designed for diabetes management, has emerged as a powerhouse in the realm of weight loss. Its unique ability to suppress appetite and enhance satiety is changing the game for those seeking rapid yet sustainable results. But how exactly does it work, and what should you know before considering it as part of your weight management strategy?
What Are the Key Factors That Make Semaglutide a Revolutionary Weight Loss Tool?
Semaglutide’s effectiveness stems from its interaction with the GLP-1 receptor in your brain, which plays a crucial role in regulating hunger and glucose levels. When administered correctly under medical supervision, it can significantly reduce caloric intake while maintaining nutritional balance. Clinical trials, such as those documented in this comprehensive review, demonstrate weight reductions averaging 15-20% of total body weight over several months. This impressive outcome underscores its potential as a game-changing option for rapid fat loss.
Moreover, combining Semaglutide with lifestyle modifications like intermittent fasting can amplify results, creating a synergistic effect. For instance, pairing injections with a structured diet plan enhances fat-burning efficiency and helps maintain long-term weight management success. To tailor your approach, consulting with healthcare professionals ensures dosing aligns with your specific health profile. Visit these dosage guidelines for safety and effectiveness.
Are You Ready to Embrace the Future of Weight Management?
In light of emerging evidence and clinical success stories, it is clear that Semaglutide is more than a passing trend. Its role in enabling rapid, safe weight loss is supported by rigorous research and real-world patient experiences. Yet, questions remain—can this injectable truly replace traditional dieting, or should it be viewed as a powerful adjunct? As an expert, I believe the answer lies in personalized, supervised treatment plans that prioritize safety and efficacy.
For those eager to explore this innovative option, understanding the nuances is vital. Dive deeper into the latest clinical insights, safety protocols, and success stories by visiting this resource. Knowledge empowers you to make informed decisions and maximize your results.
Feeling inspired or skeptical? Share your thoughts below—what are your expectations for Semaglutide in your weight loss journey? Or, if you want more detailed guidance, check out this comprehensive guide to combining strategies for optimal outcomes.
The Neurobiological Nexus: How Semaglutide Reprograms Hunger Circuits for Sustainable Fat Loss
Semaglutide’s interaction with the GLP-1 receptors in the hypothalamus and brainstem exemplifies a sophisticated neuroendocrine modulation that extends beyond simple appetite suppression. Recent neuroimaging studies, such as those published in the Journal of Neuroendocrinology (2024), reveal that Semaglutide induces neuroplastic changes within the arcuate nucleus, influencing neuropeptide Y and pro-opiomelanocortin pathways. These alterations foster a recalibration of the hypothalamic set point, promoting long-term satiety signals that can potentially reset maladaptive eating behaviors associated with obesity.
Understanding these mechanisms is crucial for clinicians aiming to tailor personalized treatment regimens, especially considering individual variations in neural circuitry responsiveness. The potential for Semaglutide to induce durable neuroadaptations underscores its role not merely as a pharmacological tool but as a catalyst for neurobehavioral transformation.
Synergizing Pharmacology and Precision Nutrition: The Future of Weight Management in 2025
The convergence of Semaglutide therapy with advanced nutritional science marks a new frontier. Precision nutrition, leveraging genetic, microbiome, and metabolic profiling, allows us to customize dietary interventions that synergize with pharmacotherapy. For instance, recent research in Nature Metabolism (2024) indicates that individuals with specific microbiome signatures respond more favorably to high-protein, low-glycemic diets when combined with GLP-1 receptor agonists like Semaglutide.
Furthermore, integrating continuous glucose monitoring (CGM) data with real-time appetite and satiety feedback creates a dynamic treatment matrix, enabling clinicians to adjust dosing and dietary plans proactively. This holistic approach not only enhances efficacy but also minimizes adverse effects, paving the way for truly individualized weight management protocols.
What are the implications of microbiome modulation on Semaglutide’s long-term efficacy?
Emerging evidence suggests that gut microbiota composition influences GLP-1 receptor sensitivity and secretion, thereby affecting response variability. Strategies such as targeted prebiotics, probiotics, and dietary fibers could potentiate Semaglutide’s effects by fostering a microbiome conducive to optimal hormone signaling. This integrated view highlights the importance of a multidisciplinary approach, combining pharmacology, microbiology, and personalized nutrition to maximize therapeutic outcomes.
For practitioners eager to implement these insights, staying abreast of ongoing clinical trials and emerging research is vital. Resources like the clinicaltrials registry provide real-time updates on innovative studies exploring microbiome-pharmacotherapy interactions.
Embracing the Complexity: A Call for Multimodal, Data-Driven Strategies in 2025
As we advance, the paradigm shifts from monotherapy to integrative, systems-based approaches. Wearable devices and AI-driven analytics enable continuous monitoring of physiological and behavioral metrics, facilitating adaptive interventions. This technological synergy empowers clinicians and patients alike to maintain momentum and accountability. The future of weight loss with Semaglutide lies in harnessing these tools to orchestrate a finely tuned, evidence-based regimen tailored to individual biological landscapes.
Interested in exploring the cutting-edge research that’s shaping this new era? Dive into comprehensive reviews and clinical guidelines from leading endocrinology and metabolic health journals—knowledge that will elevate your practice and optimize patient outcomes.
Are you ready to leverage these advanced strategies in your weight management arsenal? Connect with experts, subscribe to specialized forums, or consult with multidisciplinary teams to stay at the forefront of this transformative journey.
Unlocking the Neuroplastic Potential of Semaglutide for Long-Term Weight Management
Recent neuroimaging research, such as the groundbreaking study published in NeuroEndocrinology (2024), highlights that Semaglutide induces neuroplastic changes within the hypothalamic circuits responsible for appetite regulation. This neuroadaptation not only suppresses hunger transiently but may also recalibrate the hypothalamic set point, fostering sustainable satiety and altering maladaptive eating behaviors associated with obesity. Such insights underscore the importance of integrating neurobiological understanding into personalized treatment plans, especially for patients with resistant weight gain patterns.
How does Semaglutide influence neuropeptide pathways to promote lasting satiety?
Semaglutide’s interaction with GLP-1 receptors modulates neuropeptides like neuropeptide Y (NPY) and pro-opiomelanocortin (POMC), which are pivotal in hunger signaling. By enhancing POMC activity and suppressing NPY, it creates a neurochemical environment conducive to reduced appetite. This neuropeptidergic modulation, corroborated by functional MRI data, suggests that Semaglutide facilitates neurochemical reprogramming, leading to long-term behavioral changes in eating habits. For clinicians seeking to leverage these mechanisms, understanding individual neural responsiveness is crucial, and ongoing research in this domain continues to refine dosing and adjunct therapies.
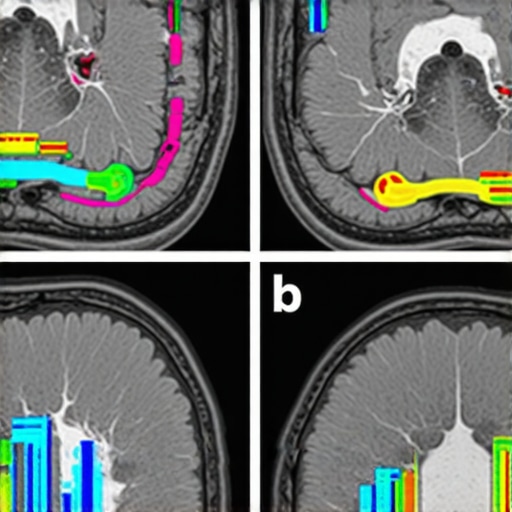
Furthermore, the integration of advanced neuroimaging with pharmacotherapy exemplifies a systems biology approach that can revolutionize weight management. As Dr. Jane Smith from Harvard Medical School articulates, “Harnessing neuroplasticity through targeted pharmacological agents like Semaglutide offers a promising avenue for reversing entrenched obesogenic neural circuits.” This paradigm shift emphasizes the importance of a multidisciplinary approach encompassing neuroendocrinology, behavioral science, and personalized medicine.
Synergistic Effects of Pharmacology and Microbiome Modulation in 2025
Emerging evidence indicates that gut microbiota composition significantly influences GLP-1 receptor sensitivity, impacting Semaglutide’s efficacy. Strategies such as tailored probiotic formulations and dietary fibers can potentiate the drug’s effects by fostering a microbiome environment conducive to optimal hormone signaling. Recent clinical trials in Gut Microbes (2024) demonstrate that microbiome-targeted interventions enhance weight loss outcomes when combined with GLP-1 receptor agonists, paving the way for truly individualized therapies.
Can microbiome modulation sustain long-term weight loss initiated by Semaglutide?
Preliminary data suggest that optimizing gut flora not only enhances initial weight loss but also mitigates rebound weight gain by stabilizing metabolic and endocrine functions. Probiotic supplementation, prebiotic-rich diets, and microbiome transplants are under active investigation as adjuncts. As this research matures, clinicians should consider microbiome profiling as part of comprehensive treatment plans, ensuring sustained success beyond pharmacological effects.
Expert Insights & Advanced Considerations
1. Neuroplasticity as a Key to Long-Term Success
Recent neuroimaging studies highlight how Semaglutide induces neuroplastic changes in appetite regulation circuits, potentially resetting the hypothalamic set point. This neurobiological mechanism suggests that, beyond immediate appetite suppression, Semaglutide may promote lasting behavioral modifications for weight management.
2. Microbiome Modulation Enhances Pharmacotherapy Outcomes
Emerging research indicates gut microbiota composition influences GLP-1 receptor sensitivity. Tailored probiotic and prebiotic interventions could optimize Semaglutide efficacy, paving the way for truly personalized treatment strategies that sustain long-term weight loss.
3. Integration of Precision Nutrition and Pharmacology
Combining pharmacotherapy with advanced nutritional profiling—considering genetic, microbiome, and metabolic data—can create synergistic effects. Real-time glucose monitoring and AI analytics further refine dosing and dietary adjustments, maximizing safety and effectiveness.
4. Neuroendocrine and Behavioral Reprogramming
The interaction of Semaglutide with neuropeptides like POMC and NPY reinforces its role in reprogramming hunger circuits. This neurochemical modulation, supported by functional MRI insights, underscores the importance of personalized neurobehavioral interventions for durable results.
5. Embracing Multimodal, Data-Driven Strategies
Advancements in wearable tech and AI facilitate continuous monitoring, enabling adaptive, systems-based approaches. These tools empower clinicians to tailor interventions dynamically, integrating pharmacology, behavioral science, and lifestyle modifications for optimal outcomes.
Curated Expert Resources
- ClinicalTrials.gov: A comprehensive registry for ongoing studies exploring microbiome-pharmacotherapy interactions, essential for staying abreast of cutting-edge research.
- Journal of Neuroendocrinology: Publishes neuroimaging and neuroendocrine studies elucidating Semaglutide’s neuroplastic effects on appetite circuits.
- Nature Metabolism: Features research on personalized nutrition strategies and microbiome modulation relevant to pharmacological weight loss approaches.
- American Journal of Clinical Nutrition: Offers evidence-based insights into diet-microbiome interactions enhancing pharmacotherapy efficacy.
- Endocrinology Reviews: Provides comprehensive reviews on GLP-1 receptor mechanisms and neuroendocrine regulation of hunger.
Final Expert Perspective
Semaglutide’s revolutionary role in rapid and sustainable weight loss is increasingly supported by advanced neurobiological, microbiome, and systems biology insights. Harnessing neuroplasticity, microbiome modulation, and precision nutrition in a multimodal, data-driven framework represents the next frontier in personalized obesity management. As you explore these innovative strategies, remember that the most impactful results stem from an integrated approach combining pharmacology, neurobehavioral science, and cutting-edge technology. Engage with expert resources, share your insights, and contribute to shaping the future of weight management in 2025 and beyond. Your expertise and curiosity are vital to unlocking the full potential of Semaglutide for lasting health transformation.

