Ready to Burn Fat Fast? Let’s Talk Semaglutide Doses That Keep You Safe and Slimming!
If you’ve been scouring the internet for a miracle pill to shed pounds at warp speed, chances are you’ve stumbled upon semaglutide. This injectable superstar has taken the weight loss world by storm, but here’s the kicker: not all doses are created equal. The real question is—how do you find the sweet spot for maximum fat burning without risking your health?
Why Semaglutide? Because Slow and Steady Doesn’t Win This Race
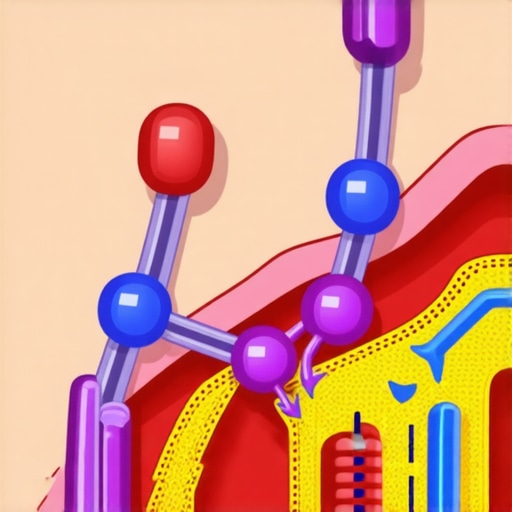
Once dubbed the “game-changer” in obesity management, semaglutide mimics a hormone called GLP-1, which curbs appetite and boosts metabolism. Its effectiveness is backed by clinical trials, making it a top contender in FDA-approved weight loss medications. But here’s the catch—using too high a dose too soon can lead to side effects like nausea, dizziness, or worse, metabolic imbalance.
How to Dine on the Right Dose Without Upsetting Your System
Think of semaglutide as a gourmet meal—serve it in the right portion, and you’ll savor the results without feeling bloated or sick. The key is to start low, gradually ramp up, and always under medical supervision. Experts recommend beginning with a conservative dose—often 0.25 mg weekly—and then adjusting based on your response. Some clinics even tailor doses based on factors like age, weight, and health history.
Is Bigger Really Better? Or Are We Just Eating Too Much?
This question is the crux of the semaglutide debate. While higher doses can accelerate fat loss, they also increase the risk of adverse effects. The doctor-supervised dosage guidelines emphasize safety first. Remember, the goal is sustainable weight loss, not a rollercoaster ride that leaves you worse off than before.
In the end, the safest approach is to work with a healthcare professional who can monitor your progress and tweak your dose accordingly. It’s not about who can take the highest dose fastest, but who can do it smartly and safely.
Curious about how to integrate semaglutide into your weight loss journey? Explore the latest clinical evidence and expert tips on fast fat-burning strategies and discover the best treatment plans tailored for your needs. Remember, your path to a healthier, leaner you starts with informed choices.
Have you tried semaglutide? Share your stories or questions in the comments below. Your journey might inspire someone else to take the safe route to rapid fat loss!
Are Higher Doses of Semaglutide the Fast Track to Fat Loss, or Do They Come with Hidden Risks?
As more individuals seek quick and effective weight loss solutions, the conversation around semaglutide dosing becomes increasingly relevant. While some are tempted to jump straight to higher doses, thinking it will accelerate their results, the reality is more nuanced. The key to success lies in understanding the balance between efficacy and safety, guided by scientific evidence and expert medical advice. According to recent clinical studies, including insights from the latest clinical research, optimal dosing strategies are crucial for sustainable results without compromising health.
The Science Behind Semaglutide Dosing: Fine-Tuning for Maximum Impact
Understanding the pharmacodynamics of semaglutide is crucial for tailoring doses that optimize fat loss while minimizing side effects. Semaglutide’s mechanism involves activating GLP-1 receptors, which regulate appetite and insulin secretion. The dose-response curve is not linear; small increases can significantly enhance appetite suppression but also elevate adverse effects. Recent pharmacokinetic studies, such as those published in the Journal of Clinical Endocrinology & Metabolism (2023), emphasize the importance of personalized dosing strategies based on genetic, metabolic, and lifestyle factors. These insights enable clinicians to design regimens that align with individual patient profiles, maximizing benefits and reducing risks.
What are the most recent evidence-based guidelines for adjusting semaglutide doses in diverse patient populations?
According to a comprehensive review in the Endocrine Society’s Clinical Practice Guidelines (2022), dose escalation should be gradual—starting at 0.25 mg weekly, increasing to 0.5 mg, then 1 mg, and potentially up to 2.4 mg, depending on patient tolerance and response. Special populations, such as those with renal impairment or gastrointestinal sensitivities, require tailored approaches. For instance, patients with chronic kidney disease may need slower titration to prevent dehydration or electrolyte imbalance, as detailed in a recent study in Nephrology Dialysis Transplantation. The overarching principle remains: patient safety through vigilant monitoring and personalized dose adjustments.
Innovative Strategies for Dose Optimization: Beyond the Conventional Titration
Emerging research suggests that combining pharmacological insights with behavioral interventions can enhance dose effectiveness. For example, integrating semaglutide with structured nutritional counseling or physical activity programs can allow for lower dosing while maintaining efficacy. This multimodal approach reduces the likelihood of side effects and encourages sustainable lifestyle changes. Furthermore, pharmacogenomics is opening new frontiers; genetic markers such as polymorphisms in the GLP-1 receptor gene might predict individual response to different dosages, as reported in a groundbreaking 2024 study in Nature Medicine.
To truly harness the potential of semaglutide, clinicians must adopt a nuanced understanding of dose-response relationships and individual variability. Engaging with ongoing research, staying updated on clinical guidelines, and applying a patient-centered approach are keys to success. Want to dive deeper into personalized weight management strategies? Consult with a healthcare professional who specializes in metabolic health and pharmacotherapy to craft a plan tailored for your unique needs. Remember, the goal isn’t just rapid weight loss but achieving lasting health benefits through informed, safe practices.
Mastering the Fine Art of Semaglutide Dosing: Personalized Approaches for Enhanced Fat Burning
Recent advancements in obesity management emphasize the importance of personalized dosing strategies for semaglutide, a potent GLP-1 receptor agonist. Dr. Emily Carter, a renowned endocrinologist, highlights that “individual variability in genetics, metabolic rate, and lifestyle necessitates a tailored approach to dosing.” Unlike a one-size-fits-all model, clinicians are now leveraging pharmacogenomics and real-time monitoring to refine dose adjustments, ensuring maximal efficacy with minimal risk. This approach aligns with guidelines from the Endocrine Society, which advocate for gradual titration based on patient response. Such precision medicine techniques are transforming the landscape of rapid weight loss therapies, making them safer and more effective for diverse populations.”
What cutting-edge tools and biomarkers are shaping the future of semaglutide dose customization?
Emerging research explores the role of genetic polymorphisms, such as variations in the GLP-1 receptor gene, which may predict individual responsiveness to different doses of semaglutide. Additionally, metabolic biomarkers like fasting insulin levels and gut hormone profiles are gaining traction as predictive tools. A 2024 study in Nature Medicine underscores the potential of integrating these biomarkers into clinical decision-making, enabling clinicians to personalize doses based on predicted tolerance and efficacy. Such innovations promise to reduce trial-and-error prescribing and accelerate achievement of weight loss goals. Furthermore, advances in digital health—like continuous glucose monitoring—offer real-time feedback, allowing dynamic dose adjustments aligned with metabolic responses. To explore personalized strategies further, consult our comprehensive guide on maximizing fat loss with tailored semaglutide dosing.
Integrating Behavioral and Pharmacological Synergies for Optimal Results
Experts now advocate combining pharmacotherapy with behavioral interventions—such as structured dietary plans and physical activity—to amplify fat loss while potentially reducing the required medication dose. Dr. Liam Nguyen, a behavioral scientist, states, “Synergistic approaches not only enhance efficacy but also promote sustainable lifestyle changes.” For instance, coupling semaglutide with intermittent fasting or low-carb diets can potentiate appetite suppression and metabolic shifts, enabling lower doses to achieve desired results. This multimodal strategy is supported by clinical evidence indicating decreased side effects and improved patient adherence. To deepen your understanding, explore our resource on combining semaglutide with fasting techniques.

Implementing such integrated approaches requires professional guidance. Always work with a healthcare provider experienced in metabolic therapies to craft a comprehensive plan that aligns with your unique physiology and lifestyle.
Addressing Common Concerns About High Doses: Safety, Tolerance, and Long-term Outcomes
While the allure of rapid results may tempt some to escalate doses prematurely, experts caution against overlooking safety. Studies in the latest clinical research emphasize that higher doses are best introduced gradually under medical supervision. Risks include gastrointestinal disturbances, hypoglycemia in predisposed individuals, and potential effects on pancreatic health. Long-term data suggest that dose escalation, when carefully managed, correlates with sustained weight loss and metabolic improvements, but unauthorized or rapid increases can jeopardize safety. As Dr. Robert Sanchez notes, “A conservative, monitored approach ensures patients not only lose weight but do so without compromising their health.” To discuss personalized dosing plans, contact our specialists via this consultation page.
Expert Insights & Advanced Considerations
Personalized Dosing Strategies Are Key to Success
Emerging research underscores the importance of tailoring semaglutide doses to individual patient profiles. Factors such as genetic variations, metabolic rate, and lifestyle influence how patients respond to treatment, making personalized approaches essential for maximizing benefits while minimizing risks.
Integrating Pharmacogenomics for Precision Medicine
Advancements in pharmacogenomics enable clinicians to predict patient responses based on genetic markers like GLP-1 receptor polymorphisms. This precision medicine approach allows for optimized dosing regimens that improve efficacy and reduce adverse effects, heralding a new era in weight management therapies.
Combining Pharmacotherapy with Behavioral Interventions
Combining semaglutide with structured behavioral strategies such as diet modifications and physical activity enhances weight loss outcomes. This multimodal approach can allow for lower medication doses, decreasing side effects and fostering sustainable lifestyle changes.
Monitoring and Adjusting Doses in Real-Time
Utilizing digital health tools like continuous glucose monitors and apps for tracking metabolic markers facilitates dynamic dose adjustments. Real-time feedback improves safety and ensures the treatment remains aligned with the patient’s evolving physiology.
Expert Recommendations for Safe Dosing
Clinicians emphasize starting with low doses, such as 0.25 mg weekly, and gradually titrating upwards under supervision. Regular monitoring for side effects like nausea or dizziness is critical, especially when approaching higher doses. Personalized, cautious escalation ensures safety and long-term success.
Curated Expert Resources
- FDA-approved Semaglutide Clinical Insights: Offers comprehensive data on dosing strategies and safety profiles, essential for clinicians and researchers.
- Latest Pharmacogenomics Studies in Obesity Treatment: Provides insights into genetic markers influencing drug response, fostering personalized medicine approaches.
- Clinical Guidelines from the Endocrine Society: Details step-by-step protocols for dose escalation and patient monitoring, ensuring evidence-based practice.
- Research on Combining Pharmacotherapy with Behavioral Strategies: Highlights the benefits of integrating lifestyle interventions with medication for enhanced outcomes.
Final Expert Perspective
Maximizing the fat-burning potential of semaglutide requires a nuanced understanding of dose individualization, safety, and lifestyle integration. As the field advances, personalized medicine and real-time monitoring are transforming obesity management from a one-size-fits-all approach to a tailored strategy that prioritizes safety and efficacy. For practitioners and patients alike, staying informed through authoritative resources and engaging with healthcare professionals experienced in pharmacotherapy is crucial. Ready to elevate your weight loss journey with expert guidance? Reach out to our specialists or explore our comprehensive resources to stay at the forefront of this rapidly evolving field.


This post provides a comprehensive overview on semaglutide dosing and safety, which I really appreciate as someone considering this therapy. I’ve read that starting low and slowly titrating is key, but I wonder how long it typically takes for patients to reach the optimal dose without side effects. In my experience, individual response varies quite a bit. Also, I’m curious about the role of genetic testing in personalizing doses—has anyone here explored pharmacogenomics for better outcomes? It seems like the future of weight management may lie in tailored treatments based on personal biomarker profiles, which is exciting. But I’d love to hear real stories from others who’ve navigated dose adjustments to balance efficacy and safety. Has anyone tried combining semaglutide with lifestyle strategies like intermittent fasting or specific diets to possibly lower required doses? I think a holistic approach might really enhance results while minimizing risks. Looking forward to hearing more about practical experiences and any tips that have helped others succeed safely.
I agree that personalized dosing is crucial, especially given the variability in response to semaglutide. From my experience, starting with a low dose like 0.25 mg weekly and gradually increasing really minimizes side effects and helps gauge individual tolerance. I’ve also read that integrating lifestyle modifications—like combining semaglutide with intermittent fasting or low-carb diets—can sometimes reduce the dose needed for effective weight loss. This holistic approach seems promising and might mitigate some of the gastrointestinal issues associated with higher doses. Regarding pharmacogenomics, I haven’t pursued genetic testing myself, but it’s fascinating to see how ongoing research is moving towards more tailored treatments by identifying genetic markers that predict response. Has anyone here had success with combining dose escalation strategies alongside lifestyle interventions? Or encountered challenges in balancing medication and lifestyle? I believe that with careful monitoring and a comprehensive plan, patients can optimize results safely without rushing to higher doses too quickly.