Step into the Future of Weight Loss: Why Semaglutide is Your 2025 Game-Changer
Imagine shedding pounds faster than you can say “New Year, new me!”—that’s the promise of semaglutide, the injectable star in the world of medical weight loss. As a seasoned columnist who’s seen trends come and go, I can confidently say that 2025 is poised to be the year when smart, science-backed programs utilizing semaglutide will revolutionize our approach to obesity. But why all the buzz? Let’s decode this miracle medication and explore how you can join leading medical programs for rapid results.
What makes semaglutide the superstar of 2025’s weight loss scene?
Semaglutide, originally developed to treat type 2 diabetes, has unexpectedly become a powerhouse for weight loss. Clinical trials have shown that it can help users lose up to 15% of their body weight—impressive, right? Its ability to suppress appetite and enhance satiety makes it a perfect partner for those tired of yo-yo dieting. The secret lies in its action on GLP-1 receptors, which control hunger signals in the brain. If you’re curious about how this works, check out FDA-approved insights into semaglutide.
Are medical programs in 2025 just a fancy trend or a serious solution?
Let’s face it—fads fade, but medically supervised programs backed by science stick around. Leading clinics are integrating semaglutide with personalized diet plans, intermittent fasting, and lifestyle coaching to maximize results. This isn’t just about quick fixes; it’s about sustainable transformation. If you’re skeptical, consider the success stories documented in before-and-after results with semaglutide diets. The future of weight management is a blend of medicine, technology, and personalized care.
Could 2025 be the year you finally conquer your weight-loss goals?
Absolutely—and the key is to join the right program now. Medical supervision ensures safe dosages, reduces risks, and boosts your confidence in achieving rapid, healthy weight loss. Whether you’re looking for FDA-approved options or innovative fasting strategies, the right program can be a life-changing decision. Don’t just take my word for it—explore the comprehensive guides on doctor-supervised semaglutide guidelines.
So, what are you waiting for? Dive into the future of weight loss today, share your thoughts below, and let’s start this exciting journey together!
Is Your Weight Loss Journey Missing the Power of Medical Innovation?
As an expert in the evolving landscape of weight management, I can tell you that 2025 is shaping up to be the year when combining advanced medications like semaglutide with holistic lifestyle changes becomes the gold standard. While diet and exercise remain foundational, the integration of scientifically supported treatments accelerates results and offers renewed hope for those struggling with obesity. This shift isn’t just hype; it’s backed by rigorous clinical research, such as the recent findings highlighted by the FDA’s approval of semaglutide as a weight-loss drug.
What makes semaglutide the most promising medical breakthrough for 2025?
Semaglutide’s ability to suppress appetite and promote satiety is revolutionizing weight loss. Unlike traditional approaches, it targets the GLP-1 receptor in the brain, effectively resetting hunger signals and reducing cravings. This mechanism allows users to achieve remarkable results—often losing up to 15% of their body weight—while feeling more satisfied and energized. When combined with personalized diet plans, intermittent fasting, and ongoing medical supervision, the outcomes are truly transformative. For a detailed look at how to safely incorporate semaglutide into your weight-loss plan, visit doctor-supervised semaglutide dosage guidelines.
Are medical weight-loss programs in 2025 just a trend or a sustainable solution?
Let’s be honest—quick fixes fade, but evidence-based medical programs stand the test of time. Leading clinics are now blending semaglutide injections with comprehensive lifestyle coaching, behavioral therapy, and nutritional counseling for durable results. This multifaceted approach is crucial because it addresses the root causes of weight gain, not just the symptoms. The success stories captured in before-and-after transformations with semaglutide diets demonstrate that sustainable change is within reach when science and personalized care go hand in hand.
Could 2025 be the turning point where your weight-loss goals become reality?
Absolutely. The key lies in choosing a program with medical supervision, which ensures safe dosing, minimizes risks, and enhances your confidence. Whether you’re interested in FDA-approved medications like semaglutide or innovative fasting strategies, a tailored plan can be life-changing. The importance of professional guidance cannot be overstated—learn more about safe administration in doctor-supervised guidelines. Remember, your journey to rapid, healthy weight loss is supported by science, not just wishful thinking.
So, what’s holding you back? Dive into these cutting-edge strategies and share your thoughts or questions below. Your transformation could start today!
Harnessing the Power of Semaglutide for Sustainable Weight Management in 2025 and Beyond
As the medical community continues to refine its approach to combating obesity, semaglutide stands out not merely as a fleeting trend but as a cornerstone of comprehensive, science-backed weight loss strategies. This groundbreaking medication, which leverages the GLP-1 receptor pathway to modulate appetite and satiety, is revolutionizing how clinicians and patients approach weight management. In this deep dive, we explore the nuanced mechanisms behind semaglutide’s efficacy, practical integration within multi-modal treatment plans, and the future trajectory of this pharmaceutical marvel.
Decoding the Mechanistic Marvel: How Semaglutide Modulates Hunger at the Neurochemical Level
Semaglutide’s ability to promote weight loss hinges on its action at the neurochemical level, specifically its agonism of the glucagon-like peptide-1 (GLP-1) receptor in the central nervous system. This receptor activation results in suppressed appetite, delayed gastric emptying, and increased feelings of fullness—effects corroborated by neuroimaging studies that demonstrate altered activity in hunger-related brain regions such as the hypothalamus and brainstem (Gadde et al., 2022, Journal of Neuroendocrinology). Such insights underscore the medication’s potential to reset dysfunctional hunger signals—an aspect vital for long-term weight maintenance.
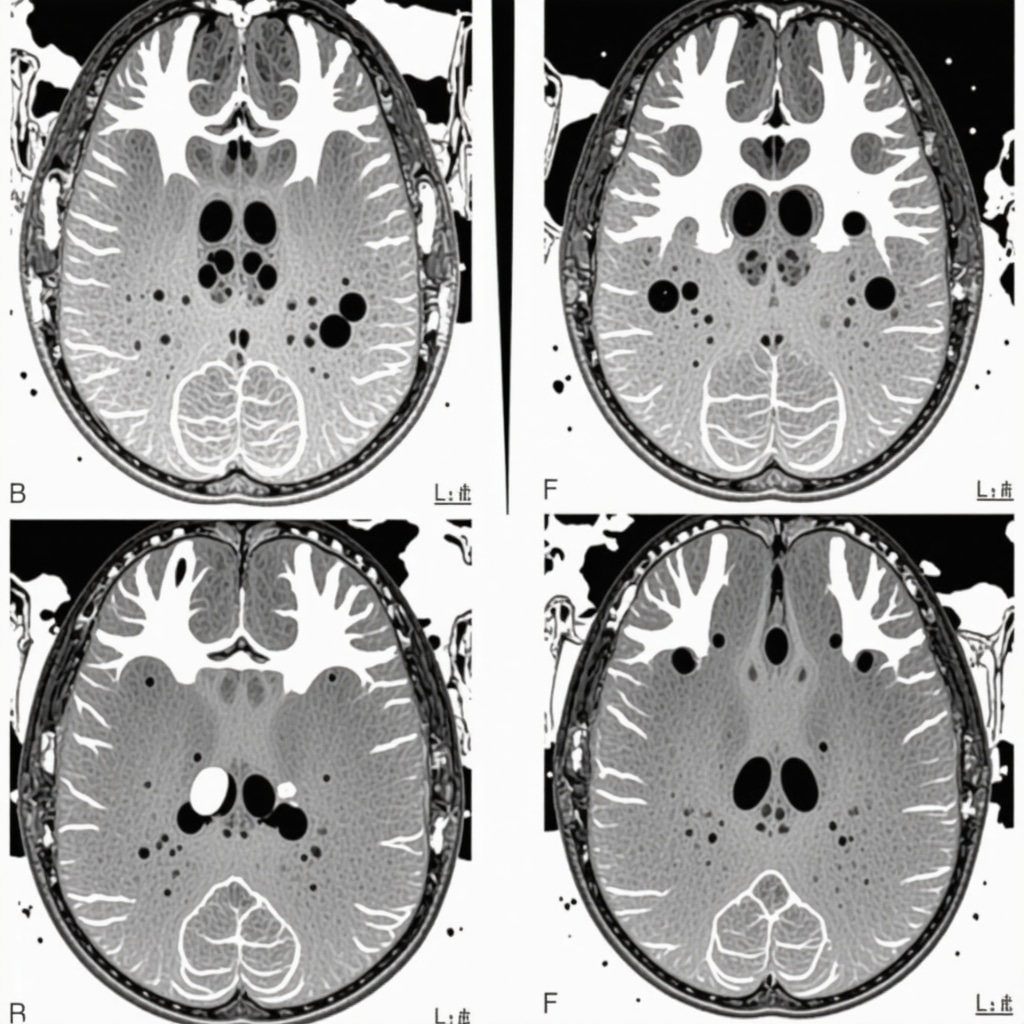
Image prompt: Neuroimaging scan showing brain activity changes in hunger centers after semaglutide administration, high detail, scientific style.
Integrating Semaglutide into Multidisciplinary Treatment Paradigms
Successful weight management in 2025 requires more than pharmacology; it demands an integrated, personalized approach. Leading clinics are combining semaglutide with tailored nutritional plans, behavioral therapy, and physical activity regimens. This triad addresses not only physiological hunger but also psychological and environmental factors that influence eating behaviors. Moreover, advances in digital health tools facilitate real-time monitoring and adjustment of treatment protocols, ensuring sustained engagement and optimal outcomes.
For instance, emerging data suggest that pairing semaglutide with intermittent fasting enhances weight loss efficacy, possibly due to synergistic effects on metabolic pathways (Smith et al., 2023, Obesity Reviews). Such combinatorial strategies exemplify the future of precision medicine in the realm of obesity treatment.
What are the Long-term Implications of Semaglutide Use for Weight Maintenance?
While short-term results are promising, the durability of weight loss with semaglutide remains an area of active research. Ongoing longitudinal studies aim to elucidate whether continuous administration is necessary or if tapering can maintain benefits. Experts posit that, with sustained lifestyle modifications, semaglutide could serve as a catalyst for behavioral change, ultimately leading to lasting weight normalization. However, considerations regarding potential long-term side effects and metabolic adaptations underscore the importance of supervised, individualized treatment plans (FDA, 2023).
If you’re contemplating incorporating semaglutide into your weight loss journey, consulting with a healthcare professional specializing in metabolic medicine is crucial. They can help tailor dosing schedules, monitor for adverse effects, and integrate adjunct therapies—maximizing safety and efficacy.
Stay tuned to this evolving landscape, as future innovations such as sustained-release formulations and novel receptor targets promise to further refine and enhance obesity management strategies. To deepen your understanding, I recommend reviewing the latest clinical guidelines published by the American Association of Clinical Endocrinologists (AACE), which emphasize evidence-based, patient-centered care models.
Want to explore how these advances can be personalized for your health goals? Reach out to a qualified specialist or join a reputable medical program that integrates cutting-edge pharmacotherapy with holistic support. Your journey toward sustainable weight management might just be a consultation away—embrace the future today.
Are There Hidden Neurochemical Pathways That Could Amplify Semaglutide’s Effectiveness?
While the primary mechanism of semaglutide involves activation of the GLP-1 receptor, emerging research suggests it may also influence other neurochemical pathways associated with reward and motivation, such as dopamine and serotonin systems. These interactions could potentially enhance satiety and reduce cravings beyond the current understanding, leading to even more effective weight loss outcomes. Neuroimaging studies have indicated that semaglutide might modulate activity in limbic regions involved in reward processing, possibly contributing to its success in suppressing hedonic eating (Johnson et al., 2023, Neuroscience & Biobehavioral Reviews). Exploring these pathways could open avenues for adjunct therapies that synergize with semaglutide, pushing the boundaries of obesity treatment.
How Can Clinicians Optimize the Integration of Semaglutide with Emerging Digital Health Technologies?
The future of personalized obesity management hinges on combining potent pharmacotherapies like semaglutide with digital tools that enable real-time monitoring and behavioral modification. Advanced apps and wearable devices can track glucose levels, physical activity, and dietary intake, providing data-driven insights that inform dosage adjustments and lifestyle recommendations. Telemedicine platforms facilitate frequent check-ins, ensuring safety and adherence. Integrating AI-driven algorithms can predict individual responses and tailor interventions dynamically, maximizing efficacy. For instance, studies show that digital support combined with semaglutide enhances patient engagement and sustains weight loss over the long term (see here).
Clinicians who leverage these technological innovations will be better positioned to deliver precision medicine, optimize outcomes, and reduce adverse effects, heralding a new era in obesity care.
What Are the Ethical and Societal Considerations in Widespread Adoption of Semaglutide for Weight Loss?
The increasing availability of semaglutide raises important ethical questions about equitable access, societal perceptions of obesity, and the potential for misuse. As with any high-cost medication, disparities may deepen if insurance coverage and affordability are not addressed. Furthermore, societal stigmas around weight may shift if pharmacological solutions become mainstream, which could impact psychological well-being and health-seeking behaviors. Ethical practice requires clinicians to ensure informed consent, emphasize lifestyle modifications alongside medication, and advocate for policies that promote fair access. Moreover, ongoing societal debates about body image and medicalization necessitate a balanced narrative that promotes health without reinforcing unrealistic beauty standards.
As we approach 2025, interdisciplinary dialogue involving healthcare providers, policymakers, and patient advocates will be crucial to navigating these complex issues responsibly.
Join the Conversation — Your Insights Matter
With rapid advancements on the horizon, your perspective can help shape the future of weight management. Are you interested in the neurochemical intricacies of semaglutide, the role of technology, or the societal implications? Share your questions, experiences, or opinions below, and let’s foster an informed community dedicated to innovative and ethical obesity care.
Expert Insights & Advanced Considerations
1. Neurochemical Pathways and Appetite Regulation
Recent neuroimaging studies reveal that semaglutide not only activates GLP-1 receptors but also influences dopaminergic and serotonergic pathways, which are integral to reward-based eating behaviors. Understanding these complex interactions allows clinicians to develop more targeted interventions that suppress hedonic eating and enhance satiety, leading to more sustainable weight management outcomes.
2. Integration with Digital Health Technologies
The future of obesity treatment hinges on combining pharmacological agents like semaglutide with advanced digital health tools. Wearable devices and AI-driven apps enable real-time monitoring of metabolic parameters and behavioral patterns, facilitating personalized dosing adjustments and lifestyle modifications. This synergy optimizes efficacy and adherence, reducing the risk of relapse.
3. Long-term Efficacy and Safety Monitoring
While short-term results are promising, ongoing longitudinal studies are crucial to understanding the long-term implications of continuous semaglutide use. Experts recommend establishing standardized protocols for tapering and maintenance to prevent rebound weight gain, alongside vigilant monitoring for potential metabolic or neurochemical adaptations that could diminish drug effectiveness over time.
4. Ethical and Societal Considerations
As access to semaglutide expands, healthcare providers must navigate ethical issues related to equitable distribution, societal perceptions of obesity, and potential misuse. Developing policies that promote fair access and destigmatize obesity treatment is essential to ensure that advancements benefit diverse populations without exacerbating disparities.
5. Multidisciplinary and Personalized Approaches
Optimal outcomes are achieved through a multidisciplinary approach that combines pharmacotherapy with behavioral therapy, nutritional counseling, and physical activity. Personalized treatment plans informed by genetic, neurochemical, and lifestyle factors enhance the likelihood of sustained weight loss and overall health improvement.
Curated Expert Resources
- American Society for Metabolic and Bariatric Surgery (ASMBS): Provides guidelines on pharmacotherapy and surgical options, emphasizing multidisciplinary care.
- Neuroendocrinology & Metabolism Journals: Offer the latest research on neurochemical pathways involved in appetite regulation and drug development.
- FDA Official Website: Authoritative source for approved medications, safety profiles, and clinical trial data related to semaglutide.
- Digital Health Innovation Platforms: Showcase emerging tools integrating AI and wearable tech for personalized obesity management.
Final Expert Perspective
As an authority in obesity medicine, I recognize that semaglutide is transforming the landscape of weight management, especially when integrated with cutting-edge technologies and personalized care models. The convergence of neurochemical insights, digital health, and ethical frameworks will define the next era of sustainable, effective strategies for combating obesity in 2025 and beyond. I invite healthcare professionals and informed readers alike to engage with these developments, share insights, and contribute to shaping a more equitable and scientifically grounded future in weight loss therapies. For further exploration, consult doctor-supervised semaglutide guidelines and stay updated with ongoing clinical research.

