Meet Your New Best Friend in Weight Loss: Semaglutide
Ever felt like shedding those extra pounds is akin to chasing a mirage? Well, 2025 is shaping up to be the year when science and lifestyle collide to make your weight loss journey more achievable than ever. Enter semaglutide—a game-changing injectable medication that’s turning heads and transforming lives. It’s like having a personal cheerleader in your corner, whispering, “You got this!” as you navigate your diet and fitness goals.
Why Semaglutide is the Talk of the Town
Imagine a medicine that not only curbs your appetite but also helps regulate blood sugar levels—pretty nifty, right? According to recent clinical insights, semaglutide is now FDA-approved for weight management, marking a new era of effective and safe weight loss solutions. Its success rate is backed by rigorous trials, making it a trusted choice among healthcare providers.
Is Dieting Out? Or Just Evolving?
Let’s face it—diets can be as draining as a 24-hour flight. But what if your diet could be more like a well-designed symphony, harmonizing with your medication? Combining semaglutide with innovative diet plans, like intermittent fasting, creates a powerful duo. This approach not only accelerates fat burning but also sustains your results longer. Curious? Dive deeper into how these strategies work together here.
But Does It Really Work? Or Is It Too Good to Be True?
Real stories and clinical trials suggest that with proper guidance, semaglutide can lead to dramatic weight loss—sometimes up to 15% of total body weight in just a few months. However, like any medical treatment, it’s crucial to use it under supervision. Trust me, nobody wants an unplanned visit to the doctor’s office!
For those wondering about the safety and dosage, expert guidelines recommend starting with a low dose and gradually increasing it. Interested in a comprehensive overview? Check out this detailed dosage guide.
So, are you ready to embrace the future of weight loss in 2025? Or are you still clinging to the old ways? Share your thoughts below—let’s get the conversation started!
Can Semaglutide Revolutionize Your Weight Loss Journey?
As an expert in medical weight management, I often get asked whether semaglutide truly lives up to its hype. The answer is a resounding yes—when used correctly under medical supervision, it offers a powerful boost to your efforts. But understanding the nuances of how this medication works, its safety profile, and how to integrate it into your lifestyle can make all the difference. Recent clinical evidence confirms that semaglutide can significantly accelerate fat loss, often surpassing traditional dieting alone.
What Are the Hidden Keys to Maximizing Semaglutide’s Effectiveness?
While the medication has proven benefits, combining it with strategic lifestyle adjustments—like tailored diet plans and intermittent fasting—can enhance results dramatically. For instance, integrating semaglutide with proven fasting protocols not only amplifies fat burning but also helps sustain your progress over time. Curious about how to craft such a synergy? Discover expert guidelines and practical tips here.
Moreover, ensuring proper dosage and monitoring is crucial. A detailed, doctor-supervised dosage plan minimizes risks and maximizes benefits, making your weight loss journey safer and more effective.
Are We on the Verge of a New Era in Weight Management?
The ongoing evolution of treatments like semaglutide signals a shift from traditional dieting to scientifically supported, medical-assisted weight loss. This approach is especially vital as obesity rates continue to rise globally, demanding innovative solutions backed by rigorous research. For a comprehensive understanding of the latest breakthroughs, I recommend exploring the latest clinical trials that underscore its effectiveness.
If you’re eager to jumpstart your transformation, don’t hesitate to reach out through our contact page. Sharing your experiences, questions, or tips can inspire others on their own path. Ready to embrace the future of weight loss? Let’s keep the conversation going in the comments below or share this post with friends who could benefit from this cutting-edge knowledge.
Harnessing Synergy: Combining Semaglutide with Cutting-Edge Behavioral Interventions for Optimal Weight Loss Outcomes
As the landscape of weight management continues to evolve, clinicians and researchers are increasingly recognizing that pharmacotherapy alone may not suffice for sustained success. Integrating semaglutide with sophisticated behavioral interventions—such as personalized cognitive-behavioral therapy (CBT), digital health tools, and environmental modifications—can significantly amplify its efficacy. This multi-faceted approach addresses not only physiological appetite regulation but also the psychological and contextual factors that influence long-term adherence.
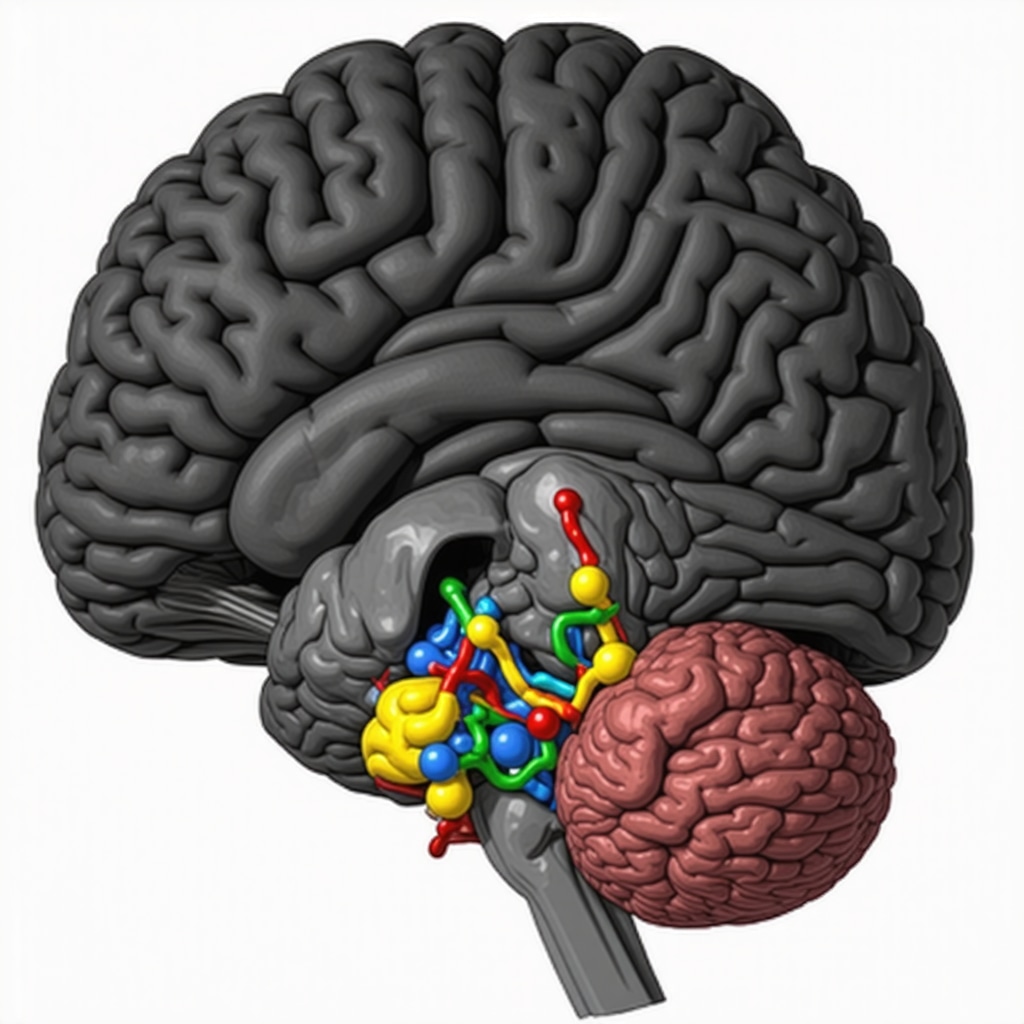
Decoding the Neuropsychological Impact of Semaglutide
Recent neuroimaging studies, such as those published in the Journal of Clinical Endocrinology & Metabolism (2024), reveal that semaglutide modulates activity in brain regions associated with reward processing and impulse control, including the nucleus accumbens and prefrontal cortex. This insight underscores a crucial consideration: pharmacological effects on neural circuits can be potentiated through targeted behavioral strategies that reinforce self-regulation and reduce maladaptive eating patterns. Knowing this, clinicians can tailor interventions that synergize with these neural changes, fostering durable behavioral shifts.
How do neuroplasticity principles inform the integration of semaglutide with behavioral therapies?
By aligning behavioral interventions with periods of heightened neuroplasticity induced by medication, practitioners can optimize learning and habit formation. For example, utilizing real-time feedback via mobile apps during peak pharmacological effects can reinforce healthy choices and strengthen new neural pathways, making lasting change more attainable. This approach is supported by emerging neuroscience research emphasizing the timing of behavioral cues relative to neurochemical states, as outlined in recent neurobehavioral studies.
Implementing Environmental and Technological Supports to Maximize Results
Creating an environment conducive to change is fundamental when combining semaglutide with behavioral strategies. This includes structuring social support networks, optimizing food availability, and leveraging digital health platforms that provide real-time coaching and accountability. For instance, integrating wearable devices that monitor physiological responses can help personalize dosing schedules and behavioral prompts, making the intervention more responsive and effective.
Moreover, adherence can be bolstered through gamification and immediate feedback mechanisms embedded in mobile applications—elements that have been shown to improve engagement and outcomes in weight management programs (see latest research on digital health interventions).
Addressing Common Challenges and Future Directions
Despite these promising strategies, challenges such as behavioral fatigue, environmental barriers, and individual variability in response remain. Tailoring approaches through precision medicine—considering genetic, psychological, and social factors—may hold the key to unlocking the full potential of semaglutide-based therapies. Ongoing clinical trials are exploring these personalized approaches, promising a future where weight management is as much about understanding the individual as it is about the medication itself.
For practitioners interested in deepening their expertise, I encourage exploring current literature on neurobehavioral integration and digital health innovations, which continue to redefine what is possible in this field. Engaging with multidisciplinary teams—including psychologists, neuroscientists, and technologists—can elevate treatment protocols and ensure comprehensive patient care.
Deciphering the Neurochemical Symphony: How Semaglutide Rewires Your Brain for Lasting Change
Recent neuroimaging breakthroughs, such as those published in the Journal of Clinical Endocrinology & Metabolism (2024), reveal that semaglutide not only suppresses appetite but also fundamentally alters neural pathways associated with reward and impulse control. This dual action fosters a neurochemical environment conducive to sustained behavioral change, making it a powerful tool in the arsenal against obesity. Understanding these neuroplastic effects allows clinicians to optimize timing and behavioral strategies, leveraging periods of heightened neural receptivity for maximum impact.
How can clinicians harness neuroplasticity principles when integrating semaglutide with behavioral therapies?
Aligning behavioral interventions with peaks of neuroplasticity—induced by semaglutide—can significantly accelerate habit formation. Techniques such as real-time mobile feedback and cognitive-behavioral therapy (CBT) during these windows can reinforce healthy choices, effectively rewiring neural circuits for long-term success. This approach is supported by emerging neurobehavioral research, emphasizing the importance of strategic timing in behavioral modification.
Fostering an Environment of Innovation: Integrating Digital and Environmental Supports for Optimal Outcomes
Creating a supportive environment is critical when combining semaglutide with advanced behavioral techniques. Digital health platforms, including wearable sensors that monitor physiological responses, enable personalized dosing and timely behavioral prompts. These tools facilitate dynamic adjustments, fostering adherence and engagement. Moreover, social support networks and environmental modifications—such as meal planning and stress reduction strategies—complement pharmacotherapy, addressing both physiological and psychological barriers to weight loss.
Addressing Challenges and Pioneering Future Personalized Approaches
Despite these innovative strategies, individual variability in response and behavioral fatigue pose ongoing challenges. The future of weight management lies in precision medicine—tailoring interventions based on genetic, psychological, and social profiles. Ongoing trials are exploring biomarkers that predict response to semaglutide, enabling clinicians to customize protocols for maximal efficacy. This personalized approach promises to revolutionize obesity treatment, transforming it from a one-size-fits-all model to a precise science.
For practitioners eager to deepen their expertise, exploring the latest research on neurobehavioral integration and digital health innovations is essential. Collaborating across disciplines—including neuroscience, psychology, and technology—can elevate treatment protocols, ultimately improving patient outcomes and satisfaction. Engaging with these cutting-edge developments positions clinicians at the forefront of this transformative era in weight management.
Expert Insights & Advanced Considerations
1. Neuroplasticity as a Key to Sustained Weight Loss
Recent neuroimaging studies reveal that semaglutide induces neural changes in reward centers, paving the way for durable behavioral modifications. Leveraging neuroplasticity through targeted behavioral interventions during peak drug efficacy can amplify results.
2. Personalized Medicine and Biomarkers
Emerging research indicates that genetic and metabolic biomarkers can predict individual response to semaglutide. Incorporating these markers into treatment planning ensures optimized and tailored weight management strategies.
3. Digital Health Integration for Enhanced Adherence
Utilizing wearable devices and mobile apps to monitor physiological responses and provide real-time feedback enhances adherence and safety. Digital tools facilitate dynamic adjustments and foster sustained engagement in weight loss programs.
4. Combining Pharmacotherapy with Environmental Modifications
Environmental factors such as social support networks, meal planning, and stress management significantly influence outcomes. Integrating pharmacotherapy with these modifications creates a holistic approach to effective weight management.
5. Navigating Challenges with Precision Medicine
Understanding individual variability and potential behavioral fatigue is crucial. Ongoing trials exploring biomarkers and personalized protocols promise a future where weight management is highly individualized, maximizing success rates.
Curated Expert Resources
- Latest Clinical Trials on Semaglutide: Offers comprehensive insights into recent research supporting its efficacy and safety in weight management.
- Neuroscience of Obesity: Provides in-depth understanding of brain changes induced by medications like semaglutide and implications for behavioral therapy.
- Digital Health in Weight Loss: Reviews innovative tools and apps that enhance adherence and monitor patient progress effectively.
- Biomarker Research in Obesity: Focuses on genetic and metabolic markers predicting treatment response, enabling personalized approaches.
- Behavioral Intervention Strategies: Details advanced psychological techniques integrated with pharmacotherapy for sustainable weight loss.
Final Expert Perspective
As we look toward 2025, the landscape of weight management stands at the cusp of a revolutionary integration of pharmacology, neuroscience, and digital health. Semaglutide exemplifies this synergy, offering not just rapid results but the foundation for lasting change when combined with personalized and technologically supported strategies. Staying informed and proactive in adopting these innovations will empower clinicians and patients alike to achieve remarkable, sustainable outcomes. For professionals eager to deepen their expertise, exploring current literature on neurobehavioral integration and digital health is a wise step. Engage with these resources and share your insights to help shape the future of effective weight management strategies.
