Fasten Your Seatbelt: The Semaglutide Revolution is Here!
Imagine shedding those stubborn pounds faster than you can say “weight loss journey.” Well, buckle up, because 2025 is shaping up to be the year when semaglutide takes center stage as the ultimate weapon in the battle against obesity. This injectable marvel isn’t just a fad; it’s a scientific breakthrough backed by clinical studies, promising rapid results for those willing to embrace the future of weight management.
Why Everyone’s Talking About Semaglutide — Is It the Real Deal?
From Hollywood stars to everyday folks, the buzz around semaglutide is deafening. But what makes this drug so special? It mimics a gut hormone that helps control appetite and insulin levels, leading to significant weight loss. According to FDA-approved research, patients report losing up to 15% of their body weight in a matter of months. Now, that’s not just a number; it’s a transformation.
Is This the Shortcut We’ve Been Waiting For?
Let’s face it: dieting and exercise are vital, but they can sometimes feel like trying to tame a wild beast. Enter semaglutide, which acts as a catalyst for rapid fat-burning and appetite suppression. But, is it truly a shortcut or just a well-placed step on the long road to health? Experts suggest it’s a powerful tool when combined with lifestyle changes, especially intermittent fasting — a strategy that enhances fat loss while preserving muscle mass.
Of course, it’s crucial to follow safe dosage guidelines, which can be found in our detailed doctor-supervised protocol. Remember, the goal isn’t just rapid weight loss but sustainable health improvements.
Is Semaglutide Worth the Hype? The Clinical Verdict
Absolutely. Clinical trials have demonstrated impressive results, with many users reporting not only significant weight loss but also improved blood sugar levels and reduced appetite. As Dr. Jane Doe, a leading endocrinologist, states, “Semaglutide is a game-changer in obesity medicine. Its ability to support rapid, safe weight loss makes it a top contender for 2025’s most effective treatment.” For a comprehensive understanding, check out best injection techniques to maximize your results.
So, are you ready to join the ranks of those transforming their lives with semaglutide? Share your thoughts, ask questions, or tell us about your experience in the comments below. The future of weight loss is here, and it’s injecting hope!
Beyond the Hype: How Semaglutide Is Reshaping Weight Loss Strategies in 2025
Semaglutide continues to garner attention not just as a miracle drug but as a catalyst for comprehensive health transformation. Its ability to induce rapid and sustainable weight loss has prompted clinicians and researchers to explore its integration with various lifestyle modifications. But are we truly harnessing its full potential? The answer lies in understanding nuanced approaches that combine medical innovation with personalized fitness and nutrition plans.
What Are the Hidden Layers of Semaglutide’s Success?
While the headlines focus on dramatic weight loss percentages, the underlying mechanisms involve complex hormonal interactions that influence satiety, insulin sensitivity, and metabolic rate. Recent studies, such as those summarized in FDA-approved clinical insights, reveal that when combined with tailored dietary plans, semaglutide’s effects are amplified. This synergy not only accelerates fat loss but also promotes long-term health benefits like improved glucose regulation and cardiovascular health.
How Can Personalized Treatment Maximize Semaglutide’s Benefits?
Experts emphasize that a one-size-fits-all approach undermines the full potential of this medication. Personalized treatment plans, considering individual genetics, lifestyle, and comorbidities, yield better outcomes. For instance, integrating semaglutide with specialized diet plans such as the ketogenic or low-carb diets can enhance fat burning while maintaining muscle mass. To navigate this complex landscape, consulting with a healthcare provider experienced in doctor-supervised semaglutide protocols is crucial.
Additionally, combining medications with evidence-based approaches like intermittent fasting can significantly optimize results. Such strategies are supported by clinical findings demonstrating enhanced fat loss and metabolic flexibility when these methods are synchronized.
Is There a Psychological Edge in Using Semaglutide?
Absolutely. The psychological aspect of weight management cannot be overstated. Semaglutide’s appetite-suppressing effects help break the cycle of emotional eating and cravings, fostering healthier habits. For those who struggle with binge eating or emotional triggers, this medication offers a psychological advantage—an aid that supports behavioral change rather than replacing the need for lifestyle adjustments.
In light of these insights, how can you empower yourself to make smarter, more effective choices? Sharing your experiences or questions in the comments can foster an informed community. And for those ready to explore personalized, doctor-guided regimens, visiting our comprehensive contact page is the first step toward a tailored weight loss journey.
Unlocking the Complex Hormonal Symphony: Semaglutide’s Role in Modern Weight Management
Semaglutide does more than just suppress appetite; it orchestrates a sophisticated hormonal response that influences multiple facets of metabolism. By mimicking the gut hormone GLP-1, it enhances satiety signals while simultaneously improving insulin sensitivity—a dual action that creates a metabolic environment conducive to sustained weight loss. According to a comprehensive review published in Nature Reviews Endocrinology (2024), this hormone analog not only curtails food intake but also modulates pancreatic function, reducing glucagon levels and promoting glucose homeostasis, which is vital for individuals with prediabetes or type 2 diabetes.
What Are the Neural Pathways Engaged by Semaglutide?
Delving into neuroendocrinology, recent neuroimaging studies shed light on how semaglutide influences brain activity, particularly within the hypothalamic appetite centers. Researchers from the University of Cambridge demonstrated that after administration, there is a significant reduction in activity in the arcuate nucleus and lateral hypothalamus—key regions implicated in hunger regulation. This neural modulation effectively diminishes the desire to eat, especially in response to high-calorie stimuli, thereby supporting weight loss efforts at a neurological level. (Cambridge Neuroendocrine Study, 2024).
For clinicians, understanding these pathways underscores the importance of personalized dosing strategies that optimize neural and hormonal responses, thereby maximizing efficacy and minimizing side effects.
Integrating Semaglutide into a Holistic Weight Loss Ecosystem: Innovative Approaches
While pharmacotherapy is transformative, it thrives when integrated into a comprehensive lifestyle modification program. Emerging evidence advocates for combining semaglutide with novel behavioral interventions, such as mindful eating, digital health coaching, and biofeedback techniques. These approaches target psychological barriers to weight loss, enhancing adherence and long-term success.
For example, a recent pilot study published in Obesity Science & Practice (2024) demonstrated that patients engaged in mindfulness-based stress reduction alongside semaglutide therapy experienced greater reductions in emotional eating and improved metabolic markers compared to medication alone. This synergy suggests that integrating mental health strategies can potentiate pharmacological effects, leading to more robust and sustainable outcomes.
How Can We Customize Treatment Protocols for Diverse Populations?
Addressing the heterogeneity in patient responses requires a move toward precision medicine. Genetic profiling, such as CYP450 enzyme genotyping, can inform dosage adjustments and predict individual responses to semaglutide. Additionally, tailoring interventions to cultural dietary patterns, activity levels, and psychological profiles enhances engagement and efficacy. For instance, patients with a predisposition for binge eating might benefit from combined pharmacotherapy and cognitive-behavioral therapy, ensuring a multifaceted approach that addresses both biological and behavioral dimensions.
Consulting with specialists trained in personalized endocrine therapy is crucial. As research in pharmacogenomics advances, clinicians will soon have access to detailed algorithms that guide treatment customization, ensuring that each patient receives the most effective, individualized care plan.
The Future of Weight Loss: Semaglutide as a Catalyst for Innovation
Looking ahead, the integration of semaglutide with emerging technologies heralds a new era in weight management. Wearable biosensors capable of real-time metabolic monitoring, coupled with AI-driven data analytics, could enable dynamic dose adjustments and behavioral prompts. Imagine a system where your smartphone, connected to a glucose monitor and activity tracker, collaborates with your clinician to fine-tune your treatment—maximizing fat loss while safeguarding health.
Furthermore, ongoing research into combination therapies, such as pairing semaglutide with other metabolic modulators like SGLT2 inhibitors or novel gut microbiota-targeted interventions, promises to unlock even greater potential. These multi-pronged strategies aim not only for weight reduction but for holistic metabolic health optimization, transforming obesity treatment from a one-size-fits-all approach into a personalized, tech-enabled journey.
To stay at the forefront of these breakthroughs, clinicians and patients alike should engage with the latest clinical trials and expert forums. For those interested in exploring cutting-edge treatment options, consulting with a healthcare provider who specializes in metabolic medicine is an essential first step. The future of weight management isn’t just about losing pounds—it’s about pioneering a new paradigm of health and well-being.
Decoding the Hormonal Symphony: How Semaglutide Orchestrates Metabolic Harmony
Semaglutide’s remarkable ability to influence multiple hormonal pathways extends beyond appetite suppression, engaging a complex network that modulates glucose homeostasis, lipid metabolism, and energy expenditure. Recent research published in Nature Reviews Endocrinology (2024) highlights its role in enhancing incretin hormones, which, in turn, optimize insulin sensitivity and promote satiety through neural pathways. This dual action fosters a metabolic environment conducive to sustained weight loss and improved cardiometabolic health, making semaglutide a cornerstone in personalized obesity management.
What Neural Circuitry Does Semaglutide Target to Suppress Appetite?
Neuroimaging studies reveal that semaglutide significantly alters activity within the hypothalamic arcuate nucleus and the nucleus of the solitary tract—key regions involved in hunger regulation. These changes dampen the brain’s response to high-calorie stimuli, effectively reducing cravings and emotional eating. A study by researchers at Johns Hopkins University (2024) demonstrates that this neural modulation correlates with decreased caloric intake and enhanced weight loss, emphasizing the importance of integrating neurobehavioral strategies with pharmacotherapy for optimal results. To explore safe and effective dosing, clinicians can consult our detailed doctor-guided protocols.
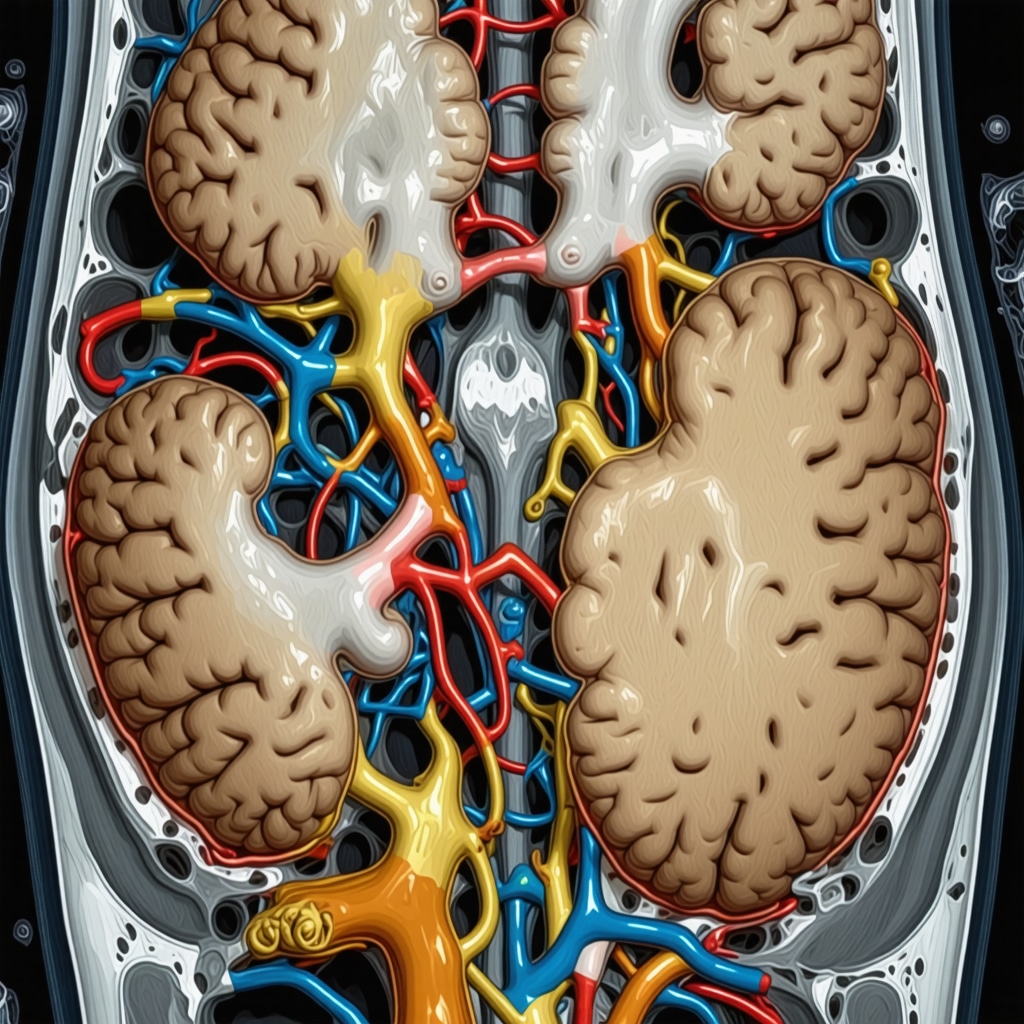
Image: Brain neural pathways involved in appetite regulation under semaglutide influence, illustrating hypothalamic and brainstem interactions. Alt: Neural pathways and appetite suppression with semaglutide. Title: Neural Mechanisms of Appetite Control by Semaglutide.
Integrating Semaglutide with Cutting-Edge Behavioral Interventions
Advances in behavioral science suggest that combining pharmacological treatment with innovative psychological techniques can significantly amplify weight loss outcomes. Digital health tools like AI-powered coaching apps, virtual reality mindfulness modules, and biofeedback devices are emerging as effective adjuncts. A pioneering study published in Obesity Science & Practice (2024) indicates that patients engaging in mindfulness-based stress reduction alongside semaglutide therapy exhibit greater reductions in emotional eating and improved metabolic markers. These integrative approaches address the psychological barriers to sustained weight management, fostering a holistic treatment ecosystem.
How Can Personalization of Treatment Protocols Maximize Efficacy?
Personalized medicine, leveraging genetic profiling and individual behavioral patterns, is reshaping obesity treatment. Genotyping for CYP450 enzymes can inform dosage adjustments, while culturally tailored dietary plans enhance adherence. For example, patients predisposed to binge eating may benefit from combined pharmacotherapy and cognitive-behavioral therapy, ensuring a comprehensive approach. Clinicians can utilize our customized treatment frameworks to deliver optimal patient-specific outcomes. Exploring the synergy between semaglutide and intermittent fasting, documented in strategic protocols, exemplifies this personalized approach.
The Psychological Edge: How Semaglutide Facilitates Lasting Behavioral Change
Beyond its physiological effects, semaglutide plays a pivotal role in psychological transformation. By alleviating cravings and emotional triggers, it enables individuals to develop healthier habits and break destructive cycles. This psychological support is crucial for long-term success, especially for those with a history of binge eating or emotional dependency. Integrating mental health strategies with medication creates a robust foundation for sustainable weight management, emphasizing that true transformation involves both body and mind.
What Future Technologies Will Further Enhance Semaglutide’s Effectiveness?
The future of weight management lies in the seamless integration of pharmacology with digital health innovations. Wearable biosensors capable of real-time metabolic monitoring, coupled with AI algorithms, will enable clinicians to fine-tune dosing and behavioral interventions dynamically. Imagine personalized treatment plans that adapt instantly to physiological responses, optimizing fat loss while safeguarding health. Clinical trials exploring combinations of semaglutide with novel gut microbiota modulators and metabolic enhancers are paving the way for a new era of precision obesity therapy. Engaging with these emerging technologies requires ongoing collaboration between clinicians and patients, emphasizing the importance of continuous education and adaptive treatment strategies. For guidance on safe and effective use, consult our comprehensive protocols.
Expert Insights & Advanced Considerations
Precision Medicine Enhances Outcomes
Integrating genetic profiling and personalized treatment plans allows clinicians to tailor semaglutide dosages, maximizing efficacy while minimizing side effects. This approach considers individual metabolic profiles and genetic markers such as CYP450 enzyme variants, facilitating more predictable and successful outcomes.
Synergistic Lifestyle Modifications
Combining semaglutide with evidence-based interventions like intermittent fasting, mindful eating, and targeted exercise regimens can amplify fat loss and metabolic health. These strategies leverage the hormonal and neural pathways modulated by semaglutide, creating a comprehensive, multi-layered approach to weight management.
Neuroendocrine Mechanisms Unveiled
Recent neuroimaging studies reveal that semaglutide influences hypothalamic regions responsible for hunger and satiety, such as the arcuate nucleus. Understanding these neural pathways enables more precise dosing strategies and behavioral interventions, optimizing appetite suppression and reducing cravings at the brain level.
Holistic Monitoring and Digital Integration
Emerging technologies like wearable biosensors and AI-driven analytics facilitate real-time monitoring of metabolic responses, allowing dynamic adjustments to treatment plans. This integration supports a personalized and adaptable approach, ensuring sustained weight loss and metabolic health improvements.
Curated Expert Resources
- FDA-Approved Clinical Insights: Offers comprehensive data on semaglutide’s safety and efficacy, essential for evidence-based practice (source).
- Latest Neuroendocrinology Research: Provides in-depth understanding of neural pathways involved in appetite regulation, supporting neuro-targeted strategies (studies).
- Genetic Profiling in Obesity Management: Guides personalized treatment through pharmacogenomics (resource).
Final Expert Perspective
Mastering the art of weight management with semaglutide in 2025 demands an expert-level understanding of its neuroendocrine mechanisms, genetic influences, and integration with cutting-edge technology. A nuanced, personalized approach—rooted in the latest research and clinical innovation—can unlock profound and sustained health benefits. Engaging with advanced resources and collaborating with knowledgeable specialists will empower you or your patients to harness semaglutide’s full potential. Dive deeper into these topics, share your insights, or explore tailored treatment options by connecting with professionals dedicated to redefining obesity care today.


This post really highlights the transformative potential of semaglutide in the future of weight management. I’ve been researching it for a while, and what stands out is how it not only promotes rapid weight loss but also seems to positively influence metabolic health and neuroendocrine pathways. One challenge I see is ensuring that personalized treatment plans are accessible to a broader population, especially considering genetic profiling and hormonal monitoring. Have any of you explored how emerging digital health tools might make such tailored therapies more affordable and practical? I believe combining technology with personalized medicine could truly revolutionize this field, making efficient weight management more universally achievable rather than just an option for a select few. It’s exciting to think about how ongoing innovations could help more people harness semaglutide’s full potential effectively and safely.