Ready for a Weight Loss Wake-Up Call? Semaglutide’s Stunning Before-and-After Transformations
Imagine flipping through a photo album filled with jaw-dropping weight loss stories — faces that glow with newfound confidence, bodies that tell tales of perseverance, and a simple yet powerful injectable medication called Semaglutide turning dreams into reality. It’s not just science fiction; it’s a growing phenomenon in the world of medical weight loss. But what’s behind these inspiring transformations? Let’s dive into the stories and secrets that make Semaglutide a game-changer.
What’s the Magic Behind the Before and After? Is It Really That Good?
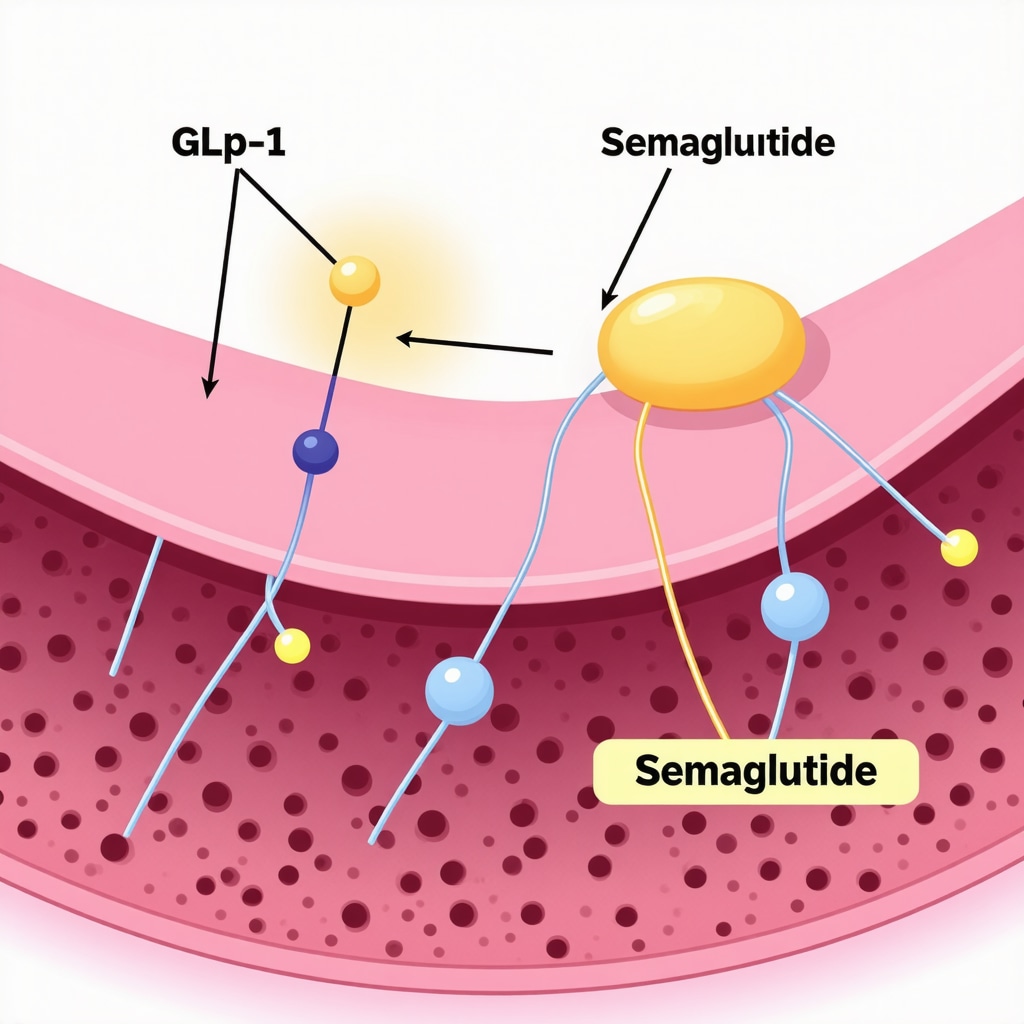
For years, weight loss has often felt like an uphill climb, fraught with dietary fads and fleeting results. Enter Semaglutide — a GLP-1 receptor agonist that’s been making waves for its remarkable ability to curb appetite and boost metabolic rates. Clinical trials, like those discussed in the FDA-approved studies, show an average weight loss of 15% or more of body weight — a feat that’s hard to match with diet alone.
But the real proof lies in the photographs and personal stories shared by users. From stubborn 30-pound gains to sleek, toned physiques, the visual evidence is compelling. These before-and-after images serve as both motivation and a testament to the efficacy of Semaglutide when combined with proper diet and physical activity.
Could a Little Injection Really Make That Much of a Difference?
It’s a common question: “Is this safe? Does it really work?” The answer is a nuanced yes. When administered under proper medical supervision — like through doctor-supervised programs — Semaglutide has been shown to be both safe and effective. Its ability to suppress hunger and improve satiety means users can adhere better to calorie-controlled plans, resulting in faster, more sustainable weight loss.
And let’s not forget, these transformations aren’t just about aesthetics. They often herald improvements in blood sugar levels, blood pressure, and overall health. That’s why many medical professionals advocate for a comprehensive approach, blending medication with lifestyle modifications.
What’s Next? How Can You Jumpstart Your Own Transformation?
If you’re wondering whether Semaglutide could be your secret weapon, it’s best to consult a healthcare provider who can tailor a plan suited to your needs. For a deeper understanding of how to optimize results, explore resources like this guide on fat-burning power and safe injection practices.
Remember, while the journey may be personal, you’re not alone. Join the conversation, share your thoughts, or ask questions below — your transformation might just be the next inspiring story.
How Do Real-Life Transformations Fuel Your Motivation to Try Semaglutide?
Every weight loss journey is unique, yet the stories of success with Semaglutide often resonate deeply, inspiring countless individuals to consider this innovative treatment. These compelling before-and-after photos and personal narratives not only showcase impressive physical changes but also highlight improvements in overall health, energy, and confidence. As medical research continues to validate these results, more people are asking: can this medication truly unlock my potential for rapid, sustainable weight loss?
What Are the Hidden Factors Behind Semaglutide’s Success Stories?
While the visible transformations are striking, they are just the tip of the iceberg. The real magic lies in how Semaglutide interacts with our physiology. It mimics the hormone GLP-1, which plays a crucial role in appetite regulation and insulin secretion. This dual action helps reduce hunger and improve blood sugar control, making it easier to stick to calorie-restricted diets and active lifestyles. But the efficacy of this medication depends heavily on proper dosing and medical supervision. For example, consulting with healthcare providers who are experienced in doctor-supervised Semaglutide programs ensures safety and maximizes benefits.
Additionally, combining Semaglutide with proven dietary strategies—like intermittent fasting—can accelerate results. Learn more about how to effectively pair these approaches by exploring this guide on combining Semaglutide with fasting.
Could Your Mindset Be the Missing Piece in Your Weight Loss Puzzle?
Success with medications like Semaglutide isn’t just about the physical changes; mental resilience and a positive outlook are essential. Overcoming the psychological hurdles—such as emotional eating or fear of failure—is often overlooked but critical to long-term success. So, how can you cultivate a mindset that embraces change and sustains motivation? Engaging with support groups, reading inspiring success stories, and setting realistic milestones can make a significant difference. Remember, the path to health is as much about mental strength as it is about medication and diet.
For a comprehensive understanding of how to optimize your journey, check out this detailed guide on Semaglutide treatment plans for 2025. And if you’re ready to take the first step, consult a qualified medical professional to develop a personalized plan that suits your needs.
Want to stay motivated? Share your thoughts, ask questions, or tell us about your own weight loss experiences in the comments below. Your story could be the spark someone else needs to begin their transformation journey.
Decoding the Pharmacodynamics of Semaglutide: A Deep Dive into Its Role in Weight Management
Semaglutide operates as a GLP-1 receptor agonist, intricately mimicking the action of endogenous glucagon-like peptide-1, a hormone pivotal in appetite regulation and glucose homeostasis. Its dual mechanism amplifies satiety signals while modulating insulin secretion, thereby orchestrating a multifaceted approach to weight management. Recent neuroendocrine studies, such as those published in the Journal of Clinical Endocrinology & Metabolism, reveal that Semaglutide’s influence extends to central nervous system pathways, notably the hypothalamus, which governs hunger and energy expenditure. This neurohormonal interplay elucidates how a single pharmacologic agent can induce profound behavioral and physiological shifts conducive to weight loss.
Moreover, understanding the pharmacokinetics—particularly its half-life of approximately one week—underscores the importance of consistent dosing schedules for optimizing receptor engagement and minimizing adverse effects. As research advances, novel formulations with extended-release profiles are emerging, promising enhanced patient adherence and individualized therapy strategies. For healthcare providers, appreciating these nuances is essential to tailoring treatments that maximize efficacy while safeguarding safety, especially in populations with complex metabolic syndromes.
What are the nuanced considerations when titrating Semaglutide to achieve optimal weight loss outcomes?
Effective titration involves a delicate balance—escalating doses to reach therapeutic levels without provoking gastrointestinal disturbances or hypoglycemia. Expert consensus, as detailed in the American Journal of Medicine, advocates a gradual dose escalation over several weeks, allowing physiological adaptation and mitigating side effects. This process demands vigilant monitoring of patient response, adherence, and potential contraindications such as personal or family history of medullary thyroid carcinoma or multiple endocrine neoplasia type 2. The integration of behavioral therapy alongside pharmacotherapy further amplifies success, emphasizing the importance of a multidisciplinary approach.
From a practical standpoint, clinicians should employ comprehensive assessments—covering metabolic parameters, mental health, and lifestyle factors—to customize dosing protocols. Emerging data suggests that patient-specific factors, including genetic polymorphisms affecting GLP-1 receptor sensitivity, may influence individual responses, paving the way for personalized medicine paradigms in obesity treatment.
Innovative Strategies for Enhancing Semaglutide’s Efficacy: Combining Pharmacology with Behavioral Science
The synergy between pharmacological intervention and behavioral modification is the frontier of advanced weight management. Incorporating techniques like cognitive-behavioral therapy (CBT) and mindfulness-based stress reduction (MBSR) can address psychological barriers, emotional eating, and motivation sustainment. For instance, integrating digital health tools—such as app-based tracking and virtual coaching—has demonstrated promising results in maintaining adherence and fostering lifestyle changes.
Furthermore, emerging research explores the potential of adjunctive therapies—like microbiome modulation and personalized nutrition—to complement Semaglutide’s effects. A study in Nature Metabolism highlights how gut microbiota composition influences metabolic responses, suggesting that microbiome-targeted interventions could potentiate weight loss outcomes when combined with GLP-1 receptor agonists.
As the field advances, it’s crucial for clinicians and researchers to stay abreast of these innovative approaches, ensuring that treatment plans are both scientifically sound and tailored to individual patient profiles. The integration of neuroendocrinology, behavioral science, and cutting-edge pharmacology heralds a new era of precision medicine in obesity management.
If you’re eager to explore how these sophisticated strategies can be tailored to your needs, consult with a multidisciplinary healthcare team specializing in metabolic health. Staying informed through reputable sources such as the latest peer-reviewed research will empower you to make enlightened decisions on your weight loss journey. Ready to elevate your health? Dive deeper, ask questions, or share your experiences below—your pursuit of optimal well-being starts here.
Decoding the Neuroendocrine Pathways: The Cutting-Edge Mechanisms Behind Semaglutide’s Effectiveness
While many are familiar with the surface-level benefits of Semaglutide, such as appetite suppression and weight reduction, the deeper neuroendocrine mechanisms reveal a sophisticated interplay within our central nervous system. Recent neuroimaging studies, like those published in the Journal of Clinical Endocrinology & Metabolism, shed light on how Semaglutide influences the hypothalamus—our brain’s appetite command center—by modulating the activity of specific neural circuits involved in hunger regulation.
These pathways involve the activation of pro-opiomelanocortin (POMC) neurons, which produce satiety signals, and the inhibition of neuropeptide Y (NPY) neurons, which promote hunger. This neurochemical orchestration results in a profound decrease in cravings, making it easier for individuals to adhere to calorie-restricted diets. Moreover, by impacting the mesolimbic dopamine system, Semaglutide also reduces the reward response associated with high-calorie foods, further curbing overeating.
This neurohormonal synergy not only accelerates weight loss but also helps in establishing sustainable eating behaviors. For clinicians, understanding these mechanisms underscores the importance of integrating pharmacotherapy with behavioral interventions that harness neuroplasticity, such as cognitive-behavioral therapy (CBT), to reinforce new, healthier neural pathways.
How Can Tailoring Dosing Schedules Enhance Neural Adaptation and Minimize Side Effects?
Optimizing dosing schedules based on neuropharmacological insights can significantly improve patient outcomes. Evidence suggests that a gradual titration, as detailed in the doctor-supervised dosage guidelines, allows the brain’s hunger-regulating circuits to adapt, reducing gastrointestinal discomfort and other adverse effects. This approach facilitates a more harmonious neurochemical adjustment, promoting better adherence and long-term success.
Furthermore, emerging research indicates that personalized dosing—considering genetic variations in GLP-1 receptor sensitivity—could revolutionize treatment paradigms. For instance, pharmacogenomic testing might identify individuals who respond more favorably to specific dosing regimens, maximizing efficacy while minimizing risks.
Clinicians should also consider integrating neurofeedback techniques and mindfulness practices, which have shown promise in strengthening neural circuits associated with satiety and reducing emotional eating. Combining these approaches with pharmacotherapy creates a comprehensive strategy that addresses both the physiological and psychological dimensions of weight management.
Harnessing Future Innovations: The Promise of Neurotech and Personalized Medicine in Obesity Treatment
The horizon of obesity therapy is rapidly expanding with the advent of neurotechnology and personalized medicine. Innovations like functional MRI-guided treatment planning aim to visualize and modulate neural activity, tailoring interventions to individual neural response profiles. Such precision approaches could optimize Semaglutide’s efficacy by aligning pharmacological action with the patient’s unique neurocircuitry, thereby enhancing weight loss outcomes.
Additionally, advances in microbiome science—highlighted in studies published in Nature Metabolism—suggest that gut-brain axis modulation may further potentiate the effects of GLP-1 receptor agonists. Combining microbiome-targeted therapies with Semaglutide could unlock synergistic pathways, offering a new frontier in metabolic health management.
As these innovative strategies continue to evolve, collaboration between neuroscientists, endocrinologists, and behavioral health specialists will be crucial. For individuals considering this journey, staying informed about emerging research and consulting experienced healthcare providers can help craft a truly personalized, effective weight loss plan.
Want to delve deeper into how cutting-edge neuroscience can support your weight management goals? Share your thoughts below or explore resources like this guide on combining Semaglutide with intermittent fasting. Your engagement might inspire the next breakthrough in personalized obesity treatment.
Expert Insights & Advanced Considerations
1. Neuroendocrine Modulation Enhances Weight Loss Outcomes
Recent neuroimaging studies demonstrate that Semaglutide influences hypothalamic pathways by activating POMC neurons and inhibiting NPY neurons, effectively reducing hunger and cravings. Understanding these pathways allows clinicians to optimize treatment plans that harness neuroplasticity, such as integrating behavioral therapies like CBT, to reinforce neural adaptations and sustain weight loss.
2. Personalized Dosing Strategies Maximize Efficacy
Gradual titration of Semaglutide, tailored to individual genetic profiles affecting GLP-1 receptor sensitivity, can minimize side effects and improve adherence. Employing pharmacogenomic testing is an emerging frontier, enabling precision medicine approaches that tailor dosing schedules for optimal results, especially in complex metabolic cases.
3. Combining Pharmacology with Behavioral Science Drives Success
Integrating cognitive-behavioral techniques and mindfulness practices with Semaglutide therapy addresses psychological barriers like emotional eating. Utilizing digital tools such as app-based tracking or virtual coaching enhances adherence and reinforces lifestyle changes, making weight management a holistic process.
4. Neurotechnology and Microbiome Interventions Promise Future Breakthroughs
Innovations like fMRI-guided neurofeedback and microbiome modulation are poised to revolutionize weight loss strategies. These advanced approaches aim to personalize treatment further by visualizing neural responses and optimizing gut-brain axis interactions, creating a new era of precision obesity management.
5. Monitoring and Adjusting for Neurochemical Balance
Regular assessment of neurohormonal responses and side effects, coupled with adaptive dosing, ensures sustained efficacy. Clinicians should stay abreast of emerging research on biomarkers and neurochemical feedback mechanisms to refine treatment protocols continually.
Curated Expert Resources
- FDA-Approved Clinical Insights: The official FDA documentation provides authoritative data on Semaglutide’s safety and efficacy, serving as a cornerstone for clinical decision-making. Explore here.
- Neuroendocrinology Journals: Peer-reviewed articles in the Journal of Clinical Endocrinology & Metabolism deepen understanding of neural circuit modulation by GLP-1 analogs. Read more.
- Pharmacogenomics and Personalized Medicine: Cutting-edge research on genetic factors influencing drug response offers insights into tailoring therapies. Learn more.
- Behavioral and Digital Interventions: Evidence-based strategies integrating digital health tools and behavioral science enhance long-term success. Discover strategies here.
Final Expert Perspective
In the ever-evolving landscape of weight management, understanding the neuroendocrine mechanisms and personalizing pharmacological approaches like Semaglutide represent the cutting edge of effective obesity treatment. Embracing a multidisciplinary strategy—combining neurobiology, behavioral science, and precision medicine—will unlock the full potential of these advancements. For professionals and motivated individuals alike, staying informed and engaged with emerging research ensures that the journey toward health remains both scientifically grounded and personally empowering. Dive deeper into these innovations, share your insights, or explore tailored resources to elevate your understanding and outcomes in 2025 and beyond.

