How I Discovered Semaglutide and Its Impact on My Weight Loss Journey
I still remember the moment I first heard about semaglutide injections. Struggling with stubborn fat despite diet and exercise, I was desperate for a solution that worked. After some research and speaking with my doctor, I decided to try semaglutide—a medication gaining attention for its rapid fat-burning properties and FDA approval for weight loss. It wasn’t just hype; the science behind it made sense to me, especially after reading insights from clinical studies showing its effectiveness.
Preparing for the First Injection: What I Learned the Hard Way
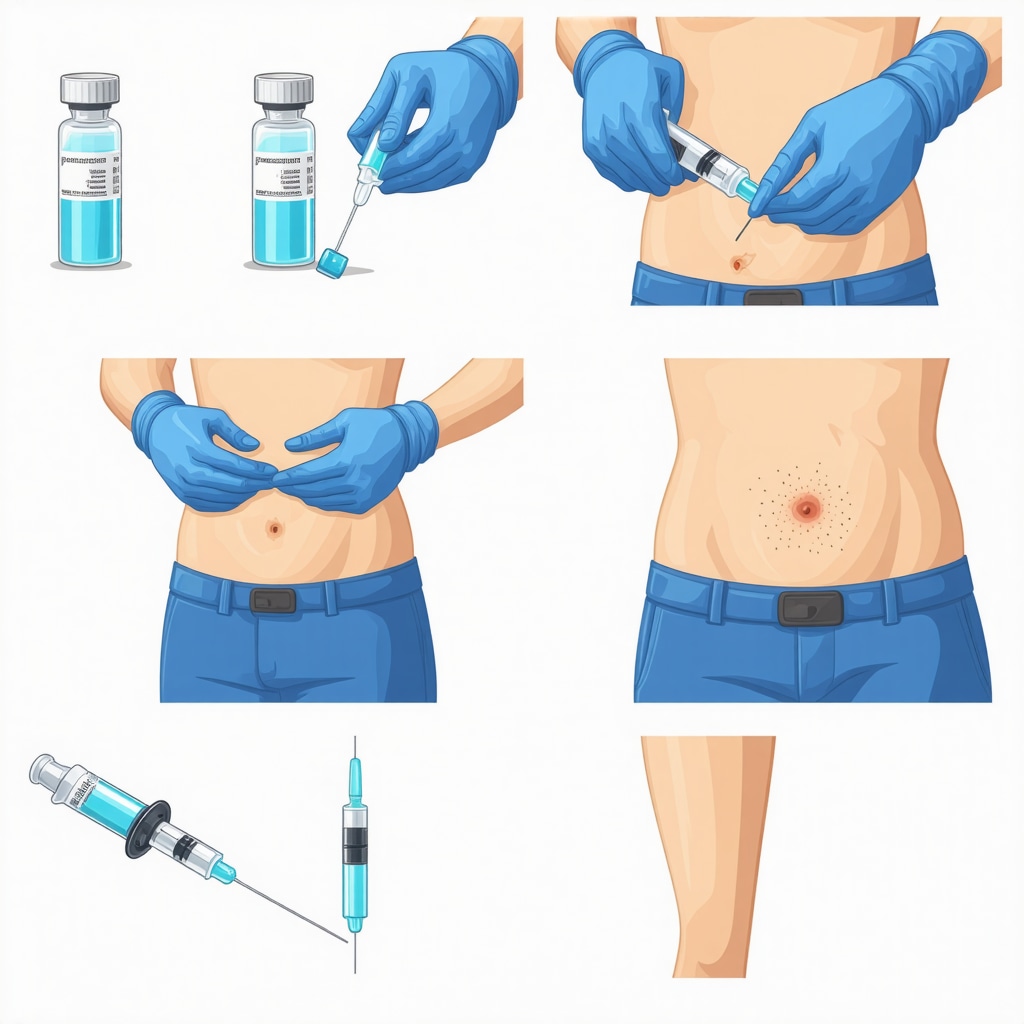
Before my first dose, I was nervous about the injection process itself. Luckily, I found a detailed step-by-step semaglutide injection guide that helped me understand everything from dosage to timing. I made sure to consult with my healthcare provider to personalize the dosage safely, as recommended in doctor-supervised protocols. The guide emphasized rotating injection sites to avoid irritation, something I initially overlooked and regretted when I experienced mild soreness.
Why Timing and Dosage Matter More Than You Think
One of the key lessons I learned was how crucial it is to stick to a consistent schedule. Semaglutide is usually administered once weekly, and I noticed that missing or delaying my shot affected my appetite control and energy levels. I followed tips from best practices for semaglutide injection dosage and timing to maximize the fat-burning benefits. Starting with a lower dose and gradually increasing it helped me avoid side effects like nausea, which some users experience.
Can Semaglutide Really Speed Up Fat Loss Safely?
This was my biggest question before starting. From my experience and extensive reading, semaglutide works by mimicking a hormone that reduces appetite and helps regulate blood sugar, leading to fewer cravings and better portion control. According to the FDA’s approval and research data, it’s considered safe when used under medical supervision. My weight loss was steady but noticeable week by week, which kept me motivated.
Practical Tips I Wish I Knew Before Starting Semaglutide Injections
Reflecting on my journey, I’d advise anyone considering semaglutide to join a doctor-supervised program for safe dosage and tailored plans. Also, combining injections with healthy eating habits and possibly intermittent fasting can amplify results—something I explored in this guide on semaglutide and intermittent fasting. Remember, injecting yourself can feel intimidating at first, but with the right technique and mindset, it becomes routine.
If you’re on this path or considering it, I’d love to hear about your experiences or questions. Feel free to share your story or ask anything in the comments below!
Understanding the Nuances of Semaglutide Dosage Adjustments
While starting semaglutide treatment, one critical factor that often gets overlooked is the individualized dosage adjustment. Each person’s metabolic response to the drug varies, so careful titration is essential to balance efficacy with tolerability. Clinicians typically begin at a low dose, slowly increasing over several weeks to minimize common side effects such as nausea or gastrointestinal discomfort. This gradual approach not only improves patient adherence but also maximizes the therapeutic benefits of the medication. For those interested in a comprehensive overview of safe dosage and usage tips for semaglutide injections, consulting medically supervised resources can be invaluable.
Combining Semaglutide with Lifestyle Interventions for Sustainable Fat Loss
Medication alone is rarely the silver bullet for long-term weight management. Integrating semaglutide therapy with evidence-based lifestyle modifications—such as balanced nutrition and regular physical activity—can significantly enhance outcomes. For instance, pairing semaglutide with intermittent fasting protocols has shown promising synergistic effects, accelerating fat oxidation and improving insulin sensitivity. Insights from this strategic guide demonstrate how timing meals and semaglutide injections can optimize metabolic benefits and minimize hunger pangs.
How Can Personalized Semaglutide Plans Address Individual Metabolic Differences?
Given the complex interplay of genetics, lifestyle, and metabolic health, a one-size-fits-all semaglutide regimen is suboptimal. Tailored plans that consider factors such as baseline insulin sensitivity, body composition, and co-existing conditions can refine dosage and timing for maximal benefit. Incorporating continuous monitoring via telemedicine or frequent clinical assessments allows adjustments responsive to patient feedback and progress. This approach aligns with modern precision medicine principles, amplifying both safety and efficacy. For those exploring personalized treatment, resources like the personalized semaglutide diet plans provide excellent frameworks.
Addressing Potential Challenges: Side Effects and Long-Term Considerations
Despite its impressive profile, semaglutide is not without potential challenges. Some users experience gastrointestinal side effects initially, which tend to diminish with proper dosing strategies. Long-term safety data, while reassuring, underscores the importance of ongoing medical supervision, particularly for populations with complex health profiles. Furthermore, psychological adaptation to appetite changes requires support to prevent compensatory behaviors. Engaging in medically supervised programs, such as those outlined in doctor-supervised semaglutide safe dosage guidelines, ensures comprehensive care and mitigates risks.
For readers interested in diving deeper into these advanced considerations or sharing their own experiences, please leave a comment below or explore our detailed discussions on doctor-supervised semaglutide weight loss programs. Your insights enrich the community’s understanding and empower others on this transformative journey.
According to a recent review published by the National Institutes of Health, semaglutide’s efficacy in weight management is significantly enhanced when combined with lifestyle interventions, supporting the integrated approach that I advocate based on my experience.
The Unexpected Emotional Journey Behind Semaglutide Use
Beyond the physical changes, one of the most profound aspects of my semaglutide experience has been the emotional adjustment. Initially, I hadn’t anticipated how appetite suppression could trigger a complex relationship with food—sometimes a sense of loss, sometimes liberation. It’s fascinating how a medication can shift not only how much you eat but how you mentally approach meals. This nuanced emotional terrain is rarely highlighted but deserves attention for anyone embarking on this path. Having a support system or counseling can be incredibly beneficial to navigate these subtler shifts alongside the physical transformation.
Why Consistency in Injection Technique Influenced My Results More Than I Expected
Early on, I treated the injection process as a routine task, but as I refined my technique—rotating injection sites carefully and ensuring proper needle angle—I noticed a clear difference in how well I tolerated the medication and how consistent my weekly results were. It’s a reminder that even small technical details affect outcomes significantly. For those interested, resources like the ultimate semaglutide injection guide for first-time users can be a treasure trove of practical tips beyond what’s typically shared in clinical settings.
How Can I Balance Semaglutide’s Benefits with Potential Long-Term Metabolic Adaptations?
This question became central to my thinking as I progressed. Semaglutide’s appetite regulation is powerful, but I wondered about the body’s natural tendency to resist prolonged weight loss through metabolic adaptations. Could extended use lead to a plateau or even metabolic slowdown? Emerging research, including findings summarized in NIH publications, suggests that combining semaglutide with intermittent fasting and tailored diet plans can mitigate some of these adaptive responses by enhancing insulin sensitivity and fat oxidation (source). This holistic approach feels more sustainable and aligns with my personal experience of maintaining momentum after initial weight loss.
Personalizing My Semaglutide Regimen: More Art Than Science
No two days were quite the same during my journey. Factors like stress, sleep quality, and even seasonal changes influenced how my body responded to semaglutide injections. I found that adjusting meal timing and sometimes even the injection day within the week, in consultation with my healthcare provider, optimized my energy and minimized side effects. This fluid, patient-centered approach was key to long-term adherence. For anyone looking to tailor their journey, exploring personalized semaglutide diet plans can offer valuable frameworks that accommodate these real-life variables without compromising safety or efficacy.
If you’re exploring your own semaglutide path or have encountered unexpected twists, I invite you to share your story or questions. Our collective experiences enrich this journey beyond clinical data and help build a community grounded in real-world wisdom.
Embracing the Complexity of Metabolic Feedback Loops During Semaglutide Treatment
Throughout my semaglutide journey, I became increasingly aware that weight loss is not a linear process, especially when influenced by potent agents like GLP-1 receptor agonists. The body’s intricate metabolic feedback mechanisms often respond to caloric deficits by slowing basal metabolic rate and altering hormone levels governing hunger and satiety. Semaglutide’s appetite suppression disrupts this natural homeostasis, yet the body seeks equilibrium, sometimes triggering subtle metabolic adaptations that can slow progress. Recognizing this dynamic helped me adjust expectations and fine-tune my approach rather than succumb to frustration. I explored scientific literature and found compelling evidence that combining semaglutide with intermittent fasting and personalized nutrition can counteract these adaptations by enhancing insulin sensitivity and promoting more effective fat oxidation, as thoroughly discussed in this strategic guide.
Integrating Advanced Monitoring Tools for Real-Time Feedback and Adjustments
To optimize my regimen beyond the standard protocols, I incorporated continuous glucose monitoring and wearable metabolic trackers. These tools offered granular insights into how my body responded to semaglutide doses, meal timing, and activity levels. Early on, I noticed that blood glucose fluctuations closely mirrored appetite changes and energy dips, enabling me to preemptively adjust injection timing or carbohydrate intake. Additionally, tracking metrics like heart rate variability and sleep quality informed my stress management strategies, which significantly influenced metabolic responsiveness. This data-driven, personalized methodology echoes modern precision medicine philosophies advocated in professional doctor-supervised semaglutide programs, ensuring safety while maximizing efficacy.
How Can Semaglutide Regimens Be Tailored to Navigate Hormonal Fluctuations and Circadian Rhythms?
This question intrigued me deeply as I observed that certain days, particularly those correlating with hormonal cycles or altered sleep patterns, seemed to modulate semaglutide’s effectiveness. Understanding that GLP-1 receptor activity might interact with circadian biology and endocrine variations, I experimented with adjusting injection timing within the week and aligning meals to my circadian rhythm. This nuanced approach reduced side effects and enhanced satiety signals during vulnerable periods. Emerging research supports these observations, highlighting the value of chronotherapy in weight management, an area ripe for further exploration. For those navigating similar challenges, personalized plans like those in this personalized semaglutide diet resource offer valuable frameworks.
The Psychological Nuances of Appetite Suppression: Beyond Physical Effects
One aspect rarely discussed in clinical summaries is the psychological recalibration required when appetite signals are pharmacologically diminished. I found that the emotional landscape around food shifted—sometimes evoking feelings of disconnection or ambivalence toward meals that were once sources of comfort or social bonding. This transition necessitated intentional mindfulness practices and, occasionally, professional counseling to maintain a healthy relationship with eating. Addressing these psychological facets is crucial for sustaining long-term success and preventing compensatory behaviors. The doctor-supervised semaglutide protocols I followed included psychological support components, underscoring their importance.
If you’re journeying with semaglutide or contemplating it, I invite you to share your nuanced experiences or intricate questions. Engaging in this dialogue enriches our collective understanding and empowers a more sophisticated, empathetic approach to weight management.
Notably, a comprehensive meta-analysis published in The Lancet Diabetes & Endocrinology reinforces that integrating semaglutide with lifestyle and behavioral interventions yields superior outcomes compared to monotherapy, emphasizing the multidimensional nature of effective obesity treatment.
Things I Wish I Knew Earlier (or You Might Find Surprising)
The Emotional Complexity of Appetite Suppression
When I first started semaglutide, I didn’t expect how much it would change my relationship with food emotionally. Appetite suppression isn’t just about eating less; it can feel like losing a familiar comfort or ritual, which was surprisingly challenging. Taking time to acknowledge these feelings and even seeking support made a big difference in staying balanced throughout the journey.
Consistency in Injection Technique Really Matters
Early on, I underestimated how much proper injection technique impacted my results and comfort. Rotating sites and using the right needle angle helped reduce soreness and made the medication’s effects more consistent. Resources like the ultimate semaglutide injection guide for first-time users were invaluable in mastering the process.
Timing Your Dose with Your Daily Rhythm
I learned that semaglutide’s effectiveness can fluctuate based on hormonal cycles and even sleep quality. Adjusting injection days slightly and syncing meals to my natural circadian rhythm helped me feel more energetic and minimized side effects. This nuanced approach felt more like an art than strict science but made a big difference in my results.
Personalization Is Key—There’s No One-Size-Fits-All
Every day brought new variables: stress, sleep, activity levels. Working closely with my healthcare provider to tweak dosage and diet plans based on how I felt helped me stick with the program longer and avoid plateaus. Exploring personalized semaglutide diet plans offers a great framework for this tailored approach.
Combining Semaglutide with Lifestyle Changes Amplifies Success
Semaglutide isn’t a magic bullet—it’s the combination with healthy habits that really seals the deal. Adding intermittent fasting and mindful eating boosted my fat-burning and kept cravings at bay. I found this synergy well-explained in this strategic guide, which I highly recommend.
Resources I’ve Come to Trust Over Time
FDA-Approved Semaglutide Clinical Insights: This resource provided the solid scientific grounding I needed to feel confident starting semaglutide. It breaks down the clinical trials and safety data clearly for everyday readers. Check it out here.
Doctor-Supervised Semaglutide Safe Dosage Guidelines: Managing dosage safely was a game-changer. This guide helped me understand how to titrate doses and avoid side effects responsibly under medical supervision. It’s a must-read for anyone new to semaglutide injections: read more.
Ultimate Semaglutide Injection Guide for First-Time Users: Injecting myself was intimidating at first, but this guide made it approachable and straightforward. It offers practical tips that go beyond the clinical basics: find the guide here.
Personalized Semaglutide Diet Plans for Maximum Weight Loss: Tailoring diet plans to your unique needs can boost semaglutide’s effectiveness. This resource helped me customize my approach and stay motivated: explore the plans.
Semaglutide and Intermittent Fasting: A Strategic Weight Loss Duo: Learning how to combine fasting with semaglutide injections enhanced my fat-burning potential. This guide shares evidence-based tips that really worked for me: check it out.
Parting Thoughts from My Perspective
Reflecting on my semaglutide journey, I realize it’s as much about understanding the subtle interplay of body, mind, and medication as it is about the physical results. The steady, safe fat loss I achieved wasn’t just from the injections themselves but from embracing a holistic, flexible approach that honored my individual rhythms and challenges. Semaglutide can be a powerful ally, especially when paired with mindful lifestyle choices and professional guidance, like those outlined in doctor-supervised programs.
If this perspective resonates with you or you’re considering starting your own semaglutide path, I warmly invite you to share your thoughts, questions, or stories. Together, we can build a community grounded in real experiences and mutual support.

Reading about your initial experience with semaglutide really resonated with me. I also struggled for years with fat that just wouldn’t budge despite exercising regularly and eating well. Like you, I was skeptical at first, especially about the injection part. What helped me was finding a detailed guide on injection techniques and dosage schedules before starting—kind of like the step-by-step guide you mentioned. One thing I wish I knew earlier was the importance of rotating injection sites; I too ended up with soreness after neglecting that. Your point about timing and dosage consistency is so crucial. I noticed on weeks where I missed or delayed my injection, my appetite spiked, which convinced me to be diligent with scheduling. I’ve been curious, though, about how others manage the psychological shifts you touched on—the emotional ups and downs from appetite suppression. Have others found strategies or support systems that help maintain a healthy relationship with food during this transition? I’m keen to hear about personal approaches since this journey is as much mental as it is physical.
I totally relate to the initial skepticism around semaglutide, especially when so many weight loss solutions promise quick results but fall short. What stood out to me in this post is the importance of personalizing the dosage and sticking to a strict injection schedule. In my own experience, consulting closely with my healthcare provider made all the difference—starting at a low dose helped me avoid nausea, which I had feared after hearing others’ side effects. It’s fascinating how semaglutide works by mimicking a hormone to reduce appetite, effectively aiding portion control. However, I was also surprised by how much the emotional and psychological side of appetite suppression played a role. Like the author mentioned, this wasn’t something I expected to navigate. Has anyone else found effective ways to balance this appetite control without feeling disconnected from the pleasure of eating? Also, has combining semaglutide with intermittent fasting or other lifestyle modifications worked well for others? I’d love to hear how different approaches have helped maintain both the physical and mental health aspects throughout the journey.
Reading about your initial discovery and cautious approach to semaglutide really resonated with me. Like many, I was initially hesitant because of the injection aspect and the idea of relying on medication for fat loss. What stood out is how much the science behind semaglutide, especially its appetite-regulating mechanism and FDA approval, influenced your decision. I also appreciate your emphasis on doctor supervision and personalized dosage—this seems crucial to manage side effects like nausea effectively.
One lesson I learned the hard way was underestimating how important the timing and consistent injection schedule would be. Missing doses disrupted my appetite control too, just like you experienced. Additionally, rotating injection sites is something I overlooked at first, leading to soreness that could have been avoided.
I’m curious about how others integrate lifestyle changes with semaglutide—have you found that intermittent fasting or mindful eating practices significantly boost results? Also, does anyone have tips on mentally navigating the emotional changes linked to appetite suppression? It seems like the psychological aspect deserves more attention, especially to help maintain a healthy relationship with food through this journey.
Reading through your detailed experience, I really appreciated the emphasis on combining semaglutide with lifestyle changes like healthy eating and intermittent fasting. When I started semaglutide therapy, I found that the science behind it—with appetite regulation and improved insulin sensitivity—was promising, but what really helped me maintain steady fat loss was that holistic approach. Like you, I initially struggled with the injection process and overlooked rotating injection sites, which caused some soreness that could have been avoided with better technique.
One insight I’d add is how critical it is to maintain an open dialogue with your healthcare provider throughout the process. Metabolic responses can vary greatly, and I found personalized dosage adjustments vital to balancing effectiveness and tolerability, especially when managing mild nausea at first. Also, syncing injection timing with your daily routine and even considering hormonal cycles—as you mentioned—can optimize outcomes.
Regarding the psychological shifts others have asked about, I’ve found that incorporating mindfulness practices and having access to counseling or support groups helped me reconcile the emotional nuances of appetite suppression. The sense of loss around habitual eating was unexpected but manageable with that support.
For others on this journey: how have you managed the balance between semaglutide’s physical effects and the emotional changes it brings? Have any of you tried different lifestyle modifications alongside the medication that improved your overall experience? It’d be great to exchange thoughts on these intertwined aspects of the process.
I really appreciate the detailed insights shared here about semaglutide injections and the balance between medication and lifestyle changes. When I first considered semaglutide, my main concern was the injection anxiety and how consistent timing affects results — which seems crucial. I also found that rotating injection sites, as others have mentioned, makes a big difference; ignoring this caused me some mild irritation early on. What stood out most is the importance of a doctor-supervised program to personalize dosage, helping to minimize side effects like nausea.
From my experience, combining semaglutide with intermittent fasting was a game changer in increasing fat loss while avoiding plateaus. The gradual titration helped my body adapt better than I expected. Also, the emotional aspect of appetite suppression is often overlooked — the feeling of detachment from food rituals can be tricky. Practicing mindfulness during meals and having an open support network made the emotional adjustment smoother for me.
I’m curious if anyone here has had success using continuous glucose monitoring or other wearable tools to fine-tune injection timing or meal planning? Has anyone noticed patterns correlating sleep quality or stress levels with semaglutide effectiveness? Sharing these personal tweaks might help us all get more from the treatment.
This post really hits home for me, especially the part about tailoring doses and paying close attention to injection technique. I’ve been using semaglutide for a few months now and found that rotating sites not only minimizes soreness but also helps me keep consistent results week to week. I’ve also been experimenting with syncing my injections with my circadian rhythms, which seems to help improve satiety and energy levels. What I’ve realized is that combining lifestyle habits like mindful eating and light exercise amplifies the medication’s effects and makes the process feel sustainable long-term. One challenge I’m still navigating is managing the emotional shifts that come with appetite suppression—sometimes I feel disconnected from my usual food rituals, which can be unsettling. How do others handle this aspect mentally? Do you find counseling or support groups helpful, or is mindfulness enough? Overall, I think the key is patience and adapting your routine as you go. Looking forward to hearing how others are integrating these strategies into their journeys.