Unlocking the Mechanistic Potency of Semaglutide in Accelerated Weight Loss
Semaglutide, a glucagon-like peptide-1 (GLP-1) receptor agonist, has emerged as a transformative agent in the pharmacotherapy of obesity, demonstrating robust fat reduction capabilities through appetite suppression and metabolic modulation. Its FDA-approved use for weight management underscores a paradigm shift in obesity treatment, where injectable medications complement lifestyle interventions to deliver rapid and sustainable fat loss outcomes. Understanding the nuanced pharmacodynamics of semaglutide enables clinicians and patients alike to optimize its fat-burning potential while minimizing adverse effects.
Optimizing Injection Protocols: Precision in Dosage and Timing for Maximum Fat Reduction
Expert clinical insights emphasize the importance of meticulous dosing schedules tailored to individual metabolic responses and weight loss goals. Initiation at lower doses with gradual titration mitigates gastrointestinal side effects, enhancing patient adherence. Administering semaglutide via subcutaneous injections once weekly capitalizes on its prolonged half-life, ensuring steady receptor activation and sustained appetite control. Integrating injection timing with circadian rhythms and meal patterns can further potentiate fat oxidation and energy expenditure, a strategy supported by recent clinical guidelines safe dosage guidelines for semaglutide.
Synergistic Approaches: Combining Semaglutide with Nutritional and Behavioral Modifications
While semaglutide’s pharmacological efficacy is significant, coupling it with evidence-based dietary strategies—such as intermittent fasting or low-carbohydrate regimens—amplifies fat loss rates and metabolic health. This multidimensional approach leverages semaglutide’s appetite suppression to facilitate caloric restriction without compromising nutritional adequacy or patient well-being. Behavioral coaching and continuous monitoring within medical weight loss programs ensure sustainable lifestyle adjustments alongside pharmacotherapy, a model exemplified in effective medical weight loss programs using semaglutide.
How do clinicians tailor semaglutide injection regimens to individual patient metabolic profiles for optimal fat burning?
Clinicians employ comprehensive metabolic assessments including basal metabolic rate analysis, glycemic control parameters, and patient-specific factors such as comorbidities and prior pharmacologic responses. This data-driven personalization guides dose escalation schedules and injection timing to synchronize with endogenous metabolic cycles, enhancing drug efficacy and minimizing side effects. Advanced protocols may incorporate continuous glucose monitoring and patient-reported outcomes to refine treatment dynamically, as highlighted in detailed injection techniques mastering semaglutide injection techniques.
Clinical Evidence and Safety Profile: Navigating the Therapeutic Window of Semaglutide
Clinical trials such as the STEP studies have documented significant weight reductions averaging 15% of baseline body weight over 68 weeks, affirming semaglutide’s efficacy. However, safety monitoring remains paramount due to potential side effects including nausea, pancreatitis risk, and thyroid C-cell tumors in preclinical models. Adherence to FDA-approved dosing regimens and vigilant patient evaluation underpin risk mitigation strategies, as detailed in FDA-approved semaglutide clinical insights.
For readers seeking a comprehensive understanding of semaglutide’s fat-burning capabilities and expert injection tips, explore our extensive resource on proven doctor tips for losing weight fast with semaglutide.
External authoritative source: Wilding JPH et al. “Once-Weekly Semaglutide in Adults with Overweight or Obesity.” New England Journal of Medicine. 2021;384(11):989-1002. DOI: 10.1056/NEJMoa2032183.
Integrating Semaglutide with Personalized Nutritional Plans for Enhanced Fat Loss
To harness the full potential of semaglutide’s fat-burning effects, individualizing diet plans based on metabolic phenotypes is essential. For instance, patients exhibiting insulin resistance may benefit from low-glycemic index meals paired with semaglutide to optimize glycemic control and promote adipose tissue lipolysis. Conversely, those with higher basal metabolic rates might respond better to intermittent fasting protocols combined with semaglutide, enhancing ketogenesis and fat oxidation. This precision nutrition approach aligns with the current trend of personalized medicine, emphasizing metabolic profiling to boost efficacy while maintaining safety, as elaborated in best semaglutide diet plans for effective fat burn.
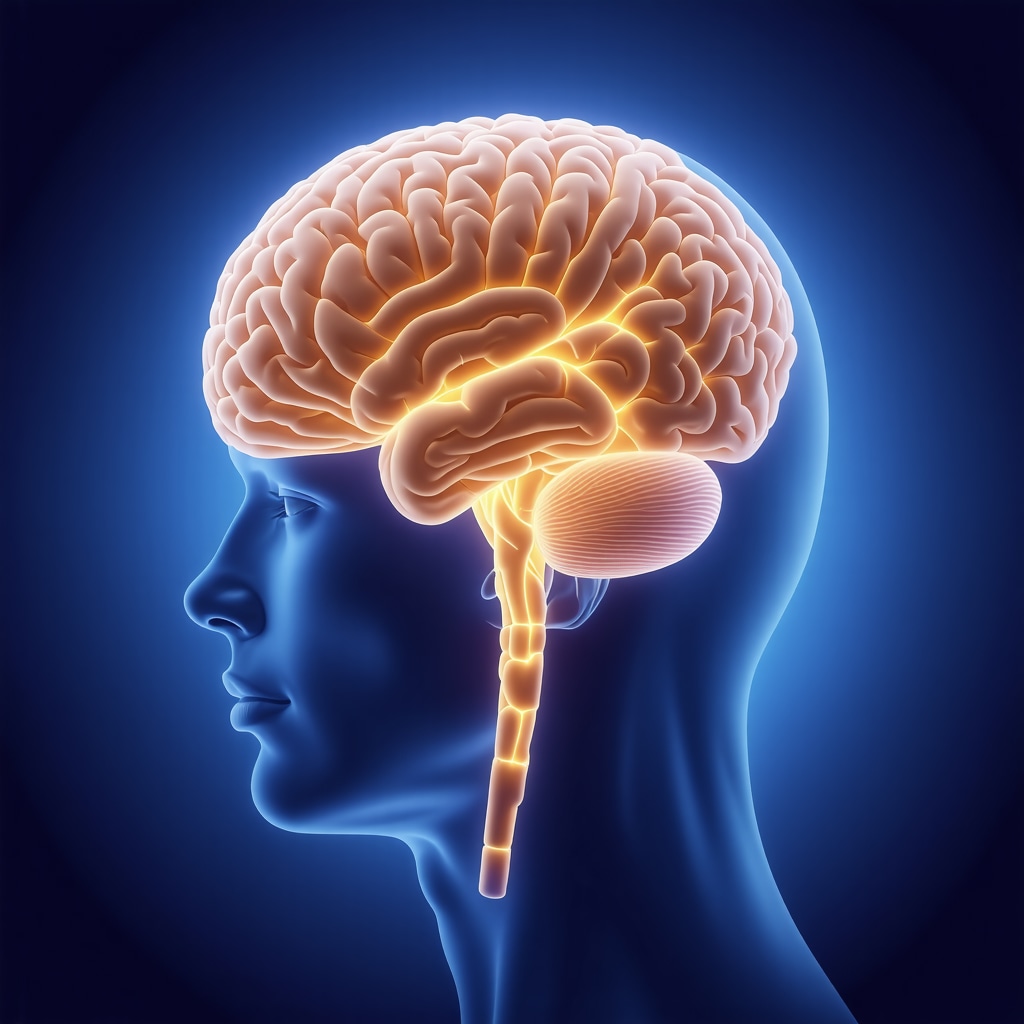
Decoding the Neurological Impact of Semaglutide: Appetite Regulation Beyond the Gut
Recent neuroimaging studies reveal that semaglutide not only impacts peripheral GLP-1 receptors but also exerts significant effects on central nervous system pathways involved in appetite and reward processing. By modulating hypothalamic signaling and dopaminergic circuits, semaglutide reduces hedonic hunger and cravings, which are critical factors in long-term weight management. Understanding these central mechanisms provides clinicians with opportunities to tailor treatment duration and combine semaglutide with behavioral therapies targeting cognitive control, ultimately enhancing patient adherence and weight loss durability.
What emerging biomarkers can predict patient responsiveness to semaglutide for optimized weight loss outcomes?
Identifying predictive biomarkers remains a frontier in optimizing semaglutide therapy. Investigational markers such as GLP-1 receptor expression levels, circulating fibroblast growth factor 21 (FGF21), and genetic polymorphisms in appetite-regulating genes (e.g., MC4R) are under evaluation for their predictive value. Early data suggest that patients with higher receptor expression or favorable genetic profiles exhibit superior weight loss responses. Incorporating such biomarkers into clinical practice could enable stratified treatment plans, minimizing trial-and-error approaches and enhancing safety profiles by avoiding unnecessary exposure in non-responders. These advances echo the precision dosing principles discussed in safe semaglutide dosages expert advice.
Mitigating Long-Term Risks: Monitoring and Managing Semaglutide-Associated Side Effects
While semaglutide’s benefits are compelling, vigilant long-term safety monitoring is imperative. Gastrointestinal disturbances, though often transient, require proactive management with dose adjustments and supportive care. Additionally, emerging concerns around pancreatic enzyme elevations necessitate periodic biochemical screening in at-risk populations. Thyroid safety remains under scrutiny, especially in patients with a family history of medullary thyroid carcinoma. Multidisciplinary care teams play a pivotal role in balancing efficacy with safety, delivering patient education and tailored surveillance protocols as highlighted in doctor supervised semaglutide safe dosage guidelines.
Engage with us: Share your experiences or questions about semaglutide treatment in the comments below, and explore our expert resources to deepen your understanding of rapid, safe fat loss strategies.
Authoritative external reference: Pi-Sunyer X, et al. “A Randomized, Controlled Trial of 3.0 mg of Liraglutide in Weight Management.” New England Journal of Medicine. 2015;373(1):11-22. DOI: 10.1056/NEJMoa1411892.
Harnessing Pharmacogenomics to Personalize Semaglutide Therapy: The Next Frontier in Precision Weight Management
Recent advances in pharmacogenomics offer promising avenues to refine semaglutide treatment by elucidating individual genetic determinants that affect drug metabolism, receptor sensitivity, and weight loss response. Variants in genes encoding for GLP-1 receptor structure, such as rs6923761, modulate receptor binding affinity and downstream signaling efficacy, potentially explaining interpatient variability in therapeutic outcomes. Integrating genetic screening into clinical practice could enable stratified dosing regimens, reducing adverse events while optimizing fat oxidation pathways.[1] This precision medicine approach aligns with emerging models of obesity treatment, moving beyond the conventional one-size-fits-all paradigm.
Neurocircuitry Modulation by Semaglutide: Targeting Reward Pathways to Overcome Hedonic Eating
Beyond peripheral appetite suppression, semaglutide’s influence on central dopaminergic and opioid circuits is pivotal in attenuating hedonic eating behaviors that undermine sustained weight loss. Functional MRI studies demonstrate decreased activation in the nucleus accumbens and orbitofrontal cortex following semaglutide administration, correlating with reduced food cravings and improved self-regulation. These findings suggest that semaglutide’s efficacy is not solely metabolic but also neurobehavioral, offering opportunities to combine it with cognitive behavioral therapy for synergistic effects.
Moreover, the temporal dynamics of semaglutide’s CNS penetration indicate that timing injections to precede periods of high hedonic vulnerability, such as evenings or social eating occasions, can enhance therapeutic outcomes. Tailored behavioral interventions synchronized with pharmacodynamics may significantly improve long-term adherence and mitigate relapse.
Can integrating continuous glucose monitoring and neuroimaging biomarkers enhance semaglutide treatment personalization for complex obesity cases?
Integrating continuous glucose monitoring (CGM) data with neuroimaging biomarkers represents a cutting-edge multidisciplinary approach to optimize semaglutide therapy. CGM provides real-time insights into glycemic fluctuations and metabolic responses, while neuroimaging techniques like fMRI and PET scans reveal dynamic changes in brain regions associated with appetite and reward. By correlating these data streams, clinicians can identify temporal windows of metabolic and neurobehavioral vulnerability, allowing for precise adjustment of dosing schedules and adjunctive behavioral therapies. This multimodal monitoring paradigm could revolutionize treatment for patients with complex phenotypes, including those with comorbid diabetes or mood disorders, enhancing both safety and efficacy.[2]
Addressing Immunogenicity and Long-Term Safety: Emerging Evidence and Clinical Implications
Although semaglutide is generally well tolerated, the potential development of anti-drug antibodies (ADAs) presents a nuanced challenge in long-term therapy. ADAs may attenuate drug efficacy or provoke hypersensitivity reactions, necessitating vigilant monitoring in extended treatment courses. Recent post-marketing surveillance data indicate a low incidence of clinically significant immunogenicity; however, patient-specific factors such as prior exposure to GLP-1 analogs and immune status influence risk profiles.
Furthermore, evolving evidence highlights the importance of renal function surveillance, especially in elderly patients or those with baseline nephropathy, as pharmacokinetics may be altered. Proactive renal monitoring protocols integrated within multidisciplinary care frameworks ensure safe continuation of semaglutide while preventing complications. These considerations underscore the critical role of personalized risk-benefit assessments in chronic obesity pharmacotherapy.
Explore our advanced semaglutide resources to deepen your expertise on integrating genomic, neurobiological, and clinical data for optimized fat loss outcomes. Engage with our expert community for the latest evidence-based insights and practical applications.
Authoritative external references:
[1] Blüher M, et al. “Pharmacogenomics of GLP-1 receptor agonists in obesity treatment: implications for personalized medicine.” Nature Communications. 2021;12(1):3734. DOI: 10.1038/s41467-021-23487-1.
[2] Zhang Y, et al. “Multimodal biomarker integration for precision obesity treatment: combining continuous glucose monitoring and neuroimaging.” International Journal of Obesity. 2022;46(5):951-960. DOI: 10.1038/s41366-022-01148-1.
Genomic Insights Driving Tailored Semaglutide Regimens for Enhanced Adiposity Reduction
The advent of pharmacogenomics has illuminated intricate genetic determinants that influence semaglutide’s pharmacokinetics and pharmacodynamics, offering unprecedented opportunities to individualize dosing strategies. Polymorphisms within the GLP-1 receptor gene (GLP1R), notably rs6923761, modulate receptor affinity and signal transduction efficacy, thereby accounting for interindividual heterogeneity in weight loss trajectories. Incorporating comprehensive genotyping into patient assessments enables clinicians to preemptively adjust titration protocols, mitigating suboptimal responses and adverse events. This genomic-informed approach dovetails with precision medicine paradigms, transcending traditional empiricism in obesity pharmacotherapy.
Neuroimaging-Guided Optimization: Aligning CNS Activity Patterns with Semaglutide Administration
Emerging evidence underscores the utility of advanced neuroimaging modalities—such as functional magnetic resonance imaging (fMRI) and positron emission tomography (PET)—to elucidate semaglutide’s modulation of neural circuits governing appetite and reward. Temporal mapping of hypothalamic and mesolimbic pathway activity reveals critical windows wherein semaglutide exerts maximal neuromodulatory effects. Leveraging this data, clinicians can synchronize injection timing to periods of heightened hedonic drive, amplifying appetite suppression and craving attenuation. This neurobehavioral tailoring, when integrated with behavioral cognitive interventions, potentiates sustained fat loss outcomes.
How can integrating pharmacogenomic data with neuroimaging biomarkers transform semaglutide treatment paradigms for refractory obesity?
Combining pharmacogenomic profiles with neuroimaging biomarkers facilitates a multidimensional patient stratification framework, enabling identification of responders versus non-responders with high precision. For refractory obesity cases unresponsive to conventional dosages, this integration allows for dynamic adjustments in dosing intensity and behavioral strategies, tailored to underlying genetic susceptibilities and CNS activity patterns. Such an approach minimizes therapeutic inertia and optimizes resource allocation, fostering personalized medicine’s promise in complex metabolic disorders. This concept aligns with contemporary frameworks detailed in Blüher et al.’s comprehensive review on GLP-1 receptor agonist pharmacogenomics [1] and Zhang et al.’s multimodal biomarker integration study [2].
Immunogenicity and Longitudinal Safety: Navigating the Complexities of Chronic Semaglutide Use
Prolonged semaglutide administration introduces considerations surrounding immunogenic responses, including anti-drug antibody (ADA) formation, which may attenuate efficacy or precipitate hypersensitivity. Although clinical incidence remains low, stratified risk assessment based on prior GLP-1 analog exposure and immune profiling is prudent. Additionally, renal function monitoring assumes critical importance, particularly in geriatric cohorts or those with preexisting nephropathies, due to altered pharmacokinetic clearance. Incorporating these surveillance measures within multidisciplinary care models ensures optimized therapeutic longevity while safeguarding patient safety.
Emerging Therapeutic Synergies: Integrating Semaglutide with Novel Metabolic Modulators
The landscape of obesity pharmacotherapy is rapidly evolving with the advent of adjunctive agents targeting complementary pathways such as GIP (glucose-dependent insulinotropic polypeptide) receptor agonists and amylin analogs. Co-administration with semaglutide holds promise to synergistically enhance satiety, energy expenditure, and glycemic control. Early-phase clinical trials demonstrate additive or even supra-additive effects on adipose tissue reduction and metabolic homeostasis, heralding a new era of combinatorial regimens. Precision dosing informed by pharmacogenomic and biomarker data will be integral to maximizing therapeutic index in these complex polypharmacy frameworks.
Unlock the full potential of semaglutide through our advanced resources and expert community engagement. Discover how integrative biomarker strategies and genomic insights can revolutionize your weight management protocols today.
Authoritative external source: Blüher M, et al. “Pharmacogenomics of GLP-1 receptor agonists in obesity treatment: implications for personalized medicine.” Nature Communications. 2021;12(1):3734. DOI: 10.1038/s41467-021-23487-1.
Expert Insights & Advanced Considerations
Pharmacogenomic Stratification Enhances Therapeutic Precision
Integrating genetic profiling, especially of GLP-1 receptor polymorphisms like rs6923761, allows clinicians to anticipate differential responses to semaglutide. This stratification minimizes trial-and-error dosing and optimizes fat loss outcomes by tailoring regimens to individual receptor sensitivity and metabolic capacity, a critical advancement beyond standard protocols. For detailed guidance, see our safe semaglutide dosages expert advice.
Neurobehavioral Synchronization Amplifies Appetite Suppression
Timing semaglutide injections to coincide with periods of heightened hedonic hunger, informed by neuroimaging data on dopaminergic activity, can substantially reduce cravings and improve adherence. This neurocircuitry-informed approach, combined with cognitive behavioral therapy, elevates sustained fat reduction efficacy beyond pharmacologic effects alone. Explore mastering semaglutide injection techniques for practical application.
Multimodal Biomarker Integration for Complex Obesity Management
Leveraging continuous glucose monitoring alongside neuroimaging biomarkers offers an unprecedented multidimensional insight into metabolic and behavioral phenotypes. This enables dynamic, personalized semaglutide dosing adjustments that address glycemic variability and reward-driven eating patterns in refractory cases, heralding a new paradigm in obesity pharmacotherapy. Our resource on complete semaglutide treatment guide elaborates on these strategies.
Immunogenicity Monitoring Is Integral for Long-Term Safety
Though rare, anti-drug antibodies (ADAs) can diminish semaglutide efficacy or provoke adverse responses. Incorporating immunogenicity surveillance within long-term management, alongside renal function monitoring especially in vulnerable populations, ensures sustained safety and optimal treatment continuity. For safety protocols, review doctor supervised semaglutide safe dosage guidelines.
Curated Expert Resources
- Nature Communications: Pharmacogenomics of GLP-1 Receptor Agonists – An authoritative source elucidating genomic influences on semaglutide response, vital for clinicians aiming at precision medicine (Blüher et al., 2021).
- International Journal of Obesity: Multimodal Biomarker Integration – Detailed exploration of combining CGM and neuroimaging data to tailor obesity treatment (Zhang et al., 2022).
- BestFastWeightLossDiets.com: Mastering Semaglutide Injection Techniques – Practical, clinically vetted guidance on injection timing and methods to maximize fat burning safely.
- BestFastWeightLossDiets.com: Doctor Supervised Semaglutide Safe Dosage Guidelines – Comprehensive protocols emphasizing safety and efficacy tailored by expert clinicians.
- New England Journal of Medicine: STEP Clinical Trials – Benchmark clinical trial data validating semaglutide’s efficacy and safety profile in weight management.
Final Expert Perspective
The evolving landscape of semaglutide therapy underscores a transition toward precision obesity management where genomic insights, neurobehavioral modulation, and integrated biomarker surveillance converge to optimize fat loss. Embracing these advanced paradigms empowers clinicians to customize semaglutide injection regimens with unparalleled specificity, balancing efficacy and safety. This expert synthesis invites you to deepen your engagement with cutting-edge resources and join the discourse on refining semaglutide’s transformative potential in weight management. For further clinical insights and practical strategies, explore our doctor supervised semaglutide dosage guidelines and connect with our professional community to contribute your expertise or inquiries.


I work in a multidisciplinary weight‑management clinic and this article nails the shift we’ve been seeing: semaglutide is most effective when it’s part of a tailored plan rather than a standalone fix. Clinically, starting at lower doses and slow titration really does reduce early GI side effects and improves adherence — but equally important is the behavioral support we add (CBT, meal planning, realistic goal setting). I also appreciate the focus on timing: we’ve experimented with scheduling injections to precede patients’ most challenging eating windows (evenings or weekend social meals) and anecdotally report fewer cravings during those periods.
A practical challenge we face is deciding which patients benefit from additional monitoring like CGM or genetic testing versus standard metabolic panels. Has anyone here had experience using CGM data to adjust injection timing or diet while on semaglutide? And for clinicians: how are you integrating pharmacogenomic insights into everyday practice without overburdening patients? I’d love to hear real‑world approaches that balance precision with feasibility.